CARY, N.C. — Earl Gray was astonished by what he found when he cut into the laboratory rats. Some had testicles that were malformed, filled with fluid, missing, or in the wrong place. Others had shriveled tubes blocking the flow of sperm, while still more were missing glands that help produce semen.
For months, Gray and his team had been feeding rats corn oil laced with phthalates, a class of chemical widely used to make plastics soft and pliable. Working for the Environmental Protection Agency in the early 1980s, Gray was evaluating how toxic substances damage the reproductive system and tested dibutyl phthalate after reading some early papers suggesting it posed a risk to human health.
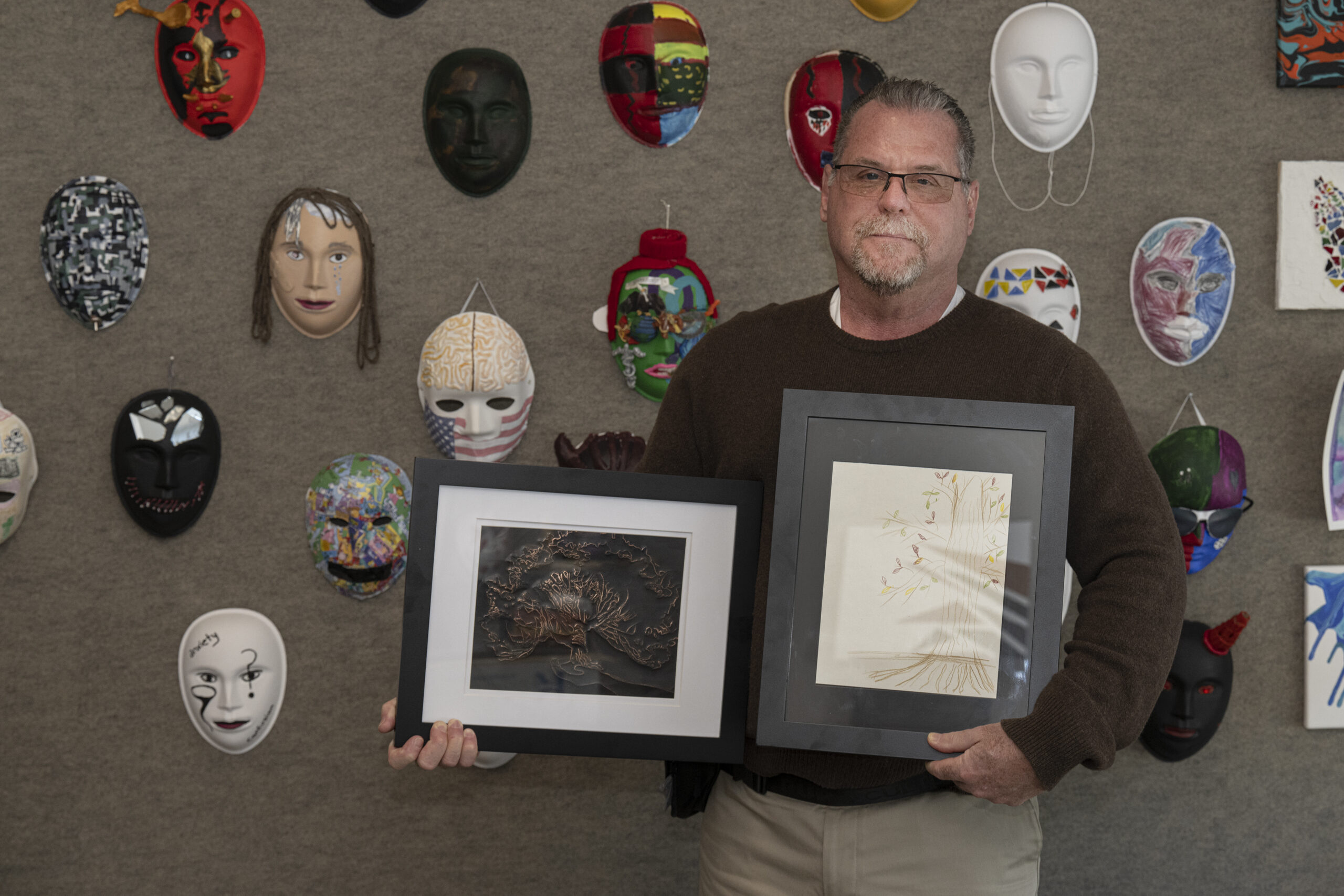
Sitting on a screened porch on a humid summer day more than 40 years later, Gray recalled the study and the grisly birth defects. “It was in enough animals, so we knew it wasn’t random malformations,” said Gray, 80, who retired after nearly 50 years with the agency.
Gray and other scientists were awakening to the potential dangers of phthalates, which were making their way into nearly every human being on the planet as plastics became a way of life in the 20th century.
Yet even as the dangers became more evident, the Food and Drug Administration, the EPA, and other regulators made only piecemeal efforts to limit their use over the next 50 years. This inaction allowed companies to continue to churn out millions of tons of phthalates for plastics manufacturing, leading these “everywhere chemicals” to become pervasive.
Today, most people are exposed to phthalates when they eat. Although industry has largely eliminated their use in food packaging — once one of the most common uses — phthalates are used in factories that make food, accumulating at high levels in ultra-processed foods. They also enter the environment through products including medical equipment, vinyl flooring, cars, cosmetics, and cheap plastic goods like shower curtains.
A large body of science has linked phthalates to a variety of serious health conditions, including premature birth and infertility. Studies have also tied the chemicals to neurodevelopment issues like ADHD. In April, a study led by New York University attributed 350,000 deaths from heart disease globally to phthalates exposure. And a University of Miami study linked phthalates’ disruption of hormones to breast cancer, a leading cause of death for women globally.
The costs to society are huge. A 2024 NYU-led study that cataloged health effects from phthalates exposure in the United States — including contributions to diabetes levels and infertility — estimated that dealing with phthalate-related diseases cost $66.7 billion in a single year. That is triple the economic impact of health impacts from “forever chemicals,” another class of chemicals widely implicated in disease. Treating all cancer, by comparison, costs the U.S. $209 billion annually, according to one estimate by the government-run National Cancer Institute.
The sporadic attention regulators have paid to this issue has allowed far more of these chemicals to circulate than what many experts consider safe. Many scientists say phthalates should have been banned or severely limited two decades ago and compare regulators’ slow response to delays in protecting the public from cigarettes and asbestos.
“If I was in charge, would I have removed it from products? Yes,” said Shanna Swan, an epidemiologist with the Icahn School of Medicine at Mount Sinai. “The only thing you can do is ban it.”
There was already “sufficient evidence” in the 2000s that pregnant women’s exposure to phthalates harmed fetal development, Swan said. At that time, studies by Swan and others found “phthalate syndrome” — telltale genital malformations — in humans that were similar to what Gray and others had found in rats.
“When you already see things in humans, that is too late,” said Maricel Maffini, an independent biochemist, who has worked with major corporations and nonprofit chemical advocacy groups. “When we see effects in humans, it is because we didn’t do a good job years earlier.”
After years of delay, federal regulators began limiting phthalates use in children’s toys in 2009, eventually banning eight compounds. The EPA is scrutinizing seven additional phthalates, but any possible action would be years away. Even the chemical Gray served to rats — dibutyl phthalate — is still on the market for use in adhesives and paints.
Industry associations say that their voluntary actions have already reduced public exposure to these chemicals.
By the mid-2000s, manufacturers had removed phthalates from plastic cling wrap. The FDA has worked with drug companies since 2012 to phase out two varieties, but others continue to be used. And in 2022, the agency granted a request from vinyl plastic manufacturers to withdraw approvals for 25 little-used phthalates in food packaging and manufacturing.
Industry groups say they have been unfairly portrayed as exposing the public to phthalates.
“It is a myth that consumer exposure to phthalates is through food packaging,” said the American Chemistry Council, the trade group that represents major phthalate manufacturers, in a statement.
These actions have reduced public exposure, but scientists say the current phthalate levels remain dangerous, especially for pregnant women and children.
“There are chemicals that in very, very, very small concentrations at certain times in your life will have a profound effect,” Maffini said. “We cannot go back and rewire the brain. We cannot go back and get the testes to be developed in a different way.”
The Washington Post spoke to 14 current and former regulators at the FDA and the EPA, who blamed an institutional culture based on weak laws and a fear of litigation for why they did not ban or restrict phthalates, as well as two dozen outside scientists and other experts.
Former regulators blame the decades of inaction on laws that did not require regulators to reexamine older chemicals that were introduced before the health dangers were known. Agency officials also feared that studies showing a link to disease would not hold up in court and companies would challenge regulators for taking action without a legal mandate.
The fact that the FDA, the EPA, and the Consumer Product Safety Commission all regulate chemicals in some fashion means that no single agency takes responsibility for all the ways people are exposed to phthalates, experts say.
“For the last 120 years of the modern chemical age, the country’s chemical safety laws were either nonexistent, ineffective, or rendered unusable, until only nine years ago,” said Michal Freedhoff, President Joe Biden’s EPA assistant administrator for chemical safety. “EPA will need to play catch-up for a very long time.”
In 2016, federal officials began to implement a 2016 amendment to the Toxic Substances Control Act that requires the EPA to systematically review chemicals already on the market. A similar process is being undertaken at the FDA, though it is not legally mandated.
Former FDA officials, including those who oversaw chemicals that come in contact with food, defended the agency’s past approach as being based on the best available science at the time.
“Within the confines of the statute and the available science, they are making the best decisions they can,” said Dennis Keefe, who headed the FDA’s Office of Food Additive Safety from 2011 until 2022.
The FDA takes decisive action when it is presented with clear proof of harms, Keefe said, and some studies may raise safety concerns but stop short of definitive proof.
The Health and Human Services Department did not respond to questions about the history of its approach to the chemicals, but spokesman Andrew Nixon said in a statement, “The FDA continues to work to better understand the safety and use of the nine phthalates still authorized for use in food contact applications, and phthalates are included on FDA’s list of chemicals in the food supply that are under review.”
EPA spokeswoman Brigit Hirsch said in a statement that before 2016, the law “did not provide a specific process or timeline for assessing and managing unreasonable risks from existing chemicals.” The agency is now prioritizing existing chemicals for review, she said, evaluating their harm and creating rules to manage unreasonable risk.
A century of exposure
Late 1800s-1940s: Phthalates, which are derived from petroleum, predate modern American regulation by decades. The chemicals were being commercially produced in the U.S. and Japan by the 1930s.
Plastic — invented in the late 1800s — was still in its infancy then. Early uses include camera film and Bakelite, an extremely hard plastic. For decades, Bakelite rotary phones and radios were the most common plastic items in an American home.
When World War II created a shortage of rubber for U.S. military equipment, scientists turned to phthalates, which make a rubberlike material when added to plastic, particularly vinyl and PVC.
1950s: After the war ended, the U.S. reoriented its newfound plastics manufacturing might toward an ever-increasing number of consumer products containing phthalates — rubber ducks, vinyl flooring, Dow Chemical’s Saran wrap — with little regulation.
In 1958, Congress directed the FDA to review new chemicals for use in food packaging and processing equipment — but the Food Additives Amendment grandfathered in approvals for most chemicals already broadly in use. Among them was di(2-ethylhexyl) phthalate (DEHP), the most commonly used phthalate and one of the most toxic, according to peer-reviewed studies by Gray and many other scientists.
1960s-1970s: The publication of Rachel Carson’s Silent Spring in 1962 led to a growing public awareness of the harms resulting from the use of pesticides. The EPA was established in 1970 but did not initially regulate chemicals already on the market. Scientists noticed the reproductive effects of phthalates on animals as early as the 1970s, but their research drew little public attention.
1980s-1990s: After Gray’s early experiments, a scientist named Theo Colborn embarked on a pioneering research program focused on chemicals that short-circuit the hormone system, including pesticides and DEHP, but later expanding to other phthalates and plastic additives.
Colborn co-wrote the 1996 book Our Stolen Future, which helped bring hormone-disrupting chemicals to public awareness, with pressure mounting over the next decade.
2000s: Amid concern over phthalates’ impact on children, the 2008 Consumer Product Safety Improvement Act banned DEHP and two other phthalates in toys like rubber ducks and dolls. A decade later, the Consumer Product Safety Commission banned using five additional phthalates in toys after determining they harm male reproductive systems.
To date, the commission’s actions on children’s toys stand out as one of the few limits that regulators have placed on phthalates.
Joint custody
The federal government has divided the primary responsibility for regulating phthalates between the FDA, which polices exposure to chemicals through food, drugs and cosmetics, and the EPA, which oversees them elsewhere, including in the environment.
For decades campaigners focused on food packaging, but companies have voluntarily addressed that concern. Nestlé, considered a leader in setting food standards, began limiting phthalates in its products in the mid-2000s, according to Stephen Klump, who helped develop tests for phthalates in his 21 years at the company. It gradually ratcheted up restrictions on its suppliers, banning the chemicals by 2018. The rest of the industry followed, Klump said.
The FDA, however, still allows nine phthalates to be used in factories processing food.
“You have hoses that are loaded with phthalates, you have plastic tanks that stuff is stored in, you have pumps that are plastic — that’s where you get a lot of phthalates,” said Tom Neltner, a longtime chemical campaigner and chemical engineer who worked in food manufacturing.
The American Chemistry Council said the FDA has approved using certain phthalates in food-contact applications like tubing, conveyor belts, and vinyl gloves, concluding that dietary exposures do not exceed safe levels.
“The leadership in FDA, both political and the senior career leadership, for decades in the food safety space, didn’t think chemicals merited much attention,” said Jim Jones, who was brought in as a deputy commissioner to overhaul food safety at the agency in 2023 after a career at the EPA.
Five phthalates that predate the 1958 food additives law, including DEHP, remain on the market. Four additional phthalates still in use were subsequently approved by the agency, though scientists say those approvals rely on outdated science.
Monsanto’s 1961 application to the FDA for the use of dicyclohexyl phthalate (DCHP) in food packaging and adhesives, obtained through a Freedom of Information Act request, relied heavily on a 1956 German study of 1,400 rats supported by Bayer (which acquired Monsanto in 2018). That study primarily looked at what doses of certain phthalates would kill them, or severely affect body and organ weight.
Gray chuckled at the study’s unsophisticated toxicology, noting it showed only how a rat would drop dead with a single dose. “It just shows things have improved quite a bit because that’s useless,” he said.
DCHP remains approved for use in contact with food.
Keefe agreed the science used in older applications “wasn’t that developed.”
Under the current process, teams of evaluators try to determine the level at which a chemical has no negative effect, and then estimate an even lower safe exposure threshold.
Historically, the agency has reconsidered legacy chemicals only on an ad hoc basis, which often happens when there is a citizen petition to reconsider a chemical, “a health concern” or public outcry, or “new evidence,” said Carrie McMahon, who worked in the Office of Food Additive Safety reviewing ingredients during her 20-year FDA career before retiring this year.
Susan Mayne, who was the director of food safety and nutrition at the FDA until 2023, said she went to Congress many times in her eight years there to request additional funding for post-market reviews of chemicals but never got it. “We were really at the mercy of what Congress would give that particular office,” she said. She said Congress also rebuffed the FDA’s efforts to charge companies a user fee to fund reviews, as is done for drugs.
One central issue in a lawsuit pushing for the FDA to revoke the approvals for dozens of phthalates is the standard that there be “reasonable certainty of no harm” for a chemical to be allowed on the market. Environmental groups argue that a substance should be banned if there is significant doubt about its safety.
But for reevaluating chemicals already in use, FDA officials require proof that a substance causes harm before removing it, a harder bar to clear.
FDA employees said the agency’s conservative approach requires clear evidence to ban or restrict chemicals, relying mostly on animal experiments rather than the many epidemiological studies showing links between exposure to phthalates and reproductive problems.
Despite voluntary corporate efforts, the chemicals are still making their way into consumers’ bodies: Centers for Disease and Control Prevention survey data show remnants of phthalates in virtually all Americans’ urine.
Last year, the Biden administration reorganized the food safety division, now called the Human Foods Program, which will set out to reevaluate old chemicals, including phthalates.
Health and Human Services Secretary Robert F. Kennedy Jr. has vowed to continue those reviews. President Donald Trump’s proposed budget asks for an additional 70 employees and $49 million to address “unsafe additives in our food supply.”
A moving target
While phthalates regulation has historically fallen mostly on the FDA, some experts say the EPA should now bear more responsibility since phthalates in the environment could be contaminating food before it’s even processed or packaged. Studies have shown the chemicals are broadly present in the environment, including in dust, rivers, and cow feed.
“Saying it’s food and pointing to the people who regulate food is not solving the problem. In fact, it’s distracting people from what the problem actually is,” said Mitchell Cheeseman, who worked at the FDA for 20 years and led its Office of Food Additive Safety.
For years, the EPA did little to regulate phthalates. In 1984 the agency set guidelines for plastics makers that put limits on discharging certain chemicals into waterways but put off action on phthalates.
In 1992, the agency established a limit on DEHP for drinking water, based primarily on data about the chemical’s cancer risk, but did note the potential reproductive concerns, according to Betsy Southerland, former science and technology director in the EPA’s Office of Water. Only in 2015 did the EPA recommend limits, in voluntary guidelines, for manufacturers discharging five phthalates.
Southerland said the agency failed to protect the public. “We knew about it in 1984,” said Southerland, who joined the EPA’s water office that year.
The EPA started to review seven phthalates under the first Trump administration and has found that two of them pose a risk to factory workers, but not the public.
But now the EPA’s chemical office has proposed reversing the Biden-era approach for evaluating toxic substances, potentially narrowing what exposure routes it considers and limiting broader actions on phthalates.
Finding safer alternatives
Other governments have taken a more aggressive approach to regulating phthalates.
European Union regulators have placed much heavier restrictions on common phthalates, because they damage the reproductive system, operating under the precautionary principle that action should be taken when any activity raises the threat of serious harm to human health or the environment, even if there is not full scientific certainty.
The EU has banned four phthalates in all but a narrow set of circumstances. And it has banned three additional phthalates in children’s toys and at least 12 in cosmetics.
“A law, a regulation, is always stronger than everything that you can achieve with voluntary agreements among the industry,” said Anne-Sofie Backär, executive director of ChemSec, a European advocacy group.
Safer Products for Washington is a program that focuses on preventing pollution and finding safer substitutes in the state. It assesses chemical classes and uses, rather than individual substances, said Marissa Smith, a toxicologist and the program’s technical lead, comparing a chemical’s hazardous properties to alternatives. If a safer substitute is available, then the chemical is phased out.
Launched in 2019, the program reviews a new batch of chemical uses every five years. In its first round it found at least seven safer alternative chemicals for phthalates in vinyl flooring and a dozen alternatives for cosmetics. Sealants, caulks, and adhesives are now under scrutiny.
Toxic-Free Future executive director Laurie Valeriano, who campaigned for the law, said this approach avoids the federal system’s pitfalls because comparing chemicals’ relative dangers is far easier than studying potential human exposure.
Smith said some substitutes might still pose health risks.
“That’s kind of a hard pill to swallow,” she said. “But it doesn’t mean that we still can’t make progress.”
Gray said he was pleased the EPA is using his research in its current assessments of phthalates, as are governments around the world. But he acknowledged regulators have taken too long to act.
“Why it took so long?” Gray asked. “I don’t know.”
Studies show levels of phthalate exposure are declining in Americans’ urine. A Harvard study found that markers of DEHP in the urine of 1,900 people in Boston fell by at least 11.9% from 2000 to 2017, although levels of some substitutes rose. But that does not erase the fact that regulators failed for decades to protect pregnant women and children from high levels of exposure, Gray said.
Gray’s own children had mostly grown up by the time he knew enough to be worried, meaning that he and other parents unknowingly dosed their children with phthalates over and over again.
“There were decades where the exposures were really high,” he said. “You don’t know what the consequences of those exposures were.”
Sitting on his neighbor’s porch, Gray recalled giving his children rubber duckies to play with in the bath. The danger now seems so clear: They were 40% phthalates.