html,body{margin:0}.inno :where(*:not(svg,svg *,.inno-no-reset,.inno-no-reset *),use){all:revert;margin:0;padding:0;border:0;list-style:none}@font-face{font-family:”Inquirer Headline”;font-weight:100;src:url(“https://media.inquirer.com/fonts/InquirerHeadline-ThinWEB.woff2”) format(“woff2”),url(“https://media.inquirer.com/fonts/InquirerHeadline-ThinWEB.woff”) format(“woff”)}@font-face{font-family:”Inquirer Headline”;font-weight:100;font-style:italic;src:url(“https://media.inquirer.com/fonts/InquirerHeadline-ThinItalicWEB.woff2”) format(“woff2”),url(“https://media.inquirer.com/fonts/InquirerHeadline-ThinItalicWEB.woff”) format(“woff”)}@font-face{font-family:”Inquirer Headline”;font-weight:300;src:url(“https://media.inquirer.com/fonts/InquirerHeadline-LightWEB.woff2”) format(“woff2”),url(“https://media.inquirer.com/fonts/InquirerHeadline-LightWEB.woff”) format(“woff”)}@font-face{font-family:”Inquirer Headline”;font-weight:300;font-style:italic;src:url(“https://media.inquirer.com/fonts/InquirerHeadline-LightItalicWEB.woff2”) format(“woff2”),url(“https://media.inquirer.com/fonts/InquirerHeadline-LightItalicWEB.woff”) format(“woff”)}@font-face{font-family:”Inquirer Headline”;font-weight:normal;src:url(“https://media.inquirer.com/fonts/InquirerHeadline-RegularWEB.woff2”) format(“woff2”),url(“https://media.inquirer.com/fonts/InquirerHeadline-RegularWEB.woff”) format(“woff”)}@font-face{font-family:”Inquirer Headline”;font-weight:normal;font-style:italic;src:url(“https://media.inquirer.com/fonts/InquirerHeadline-RegularItalicWEB.woff2”) format(“woff2”),url(“https://media.inquirer.com/fonts/InquirerHeadline-RegularItalicWEB.woff”) format(“woff”)}@font-face{font-family:”Inquirer Headline”;font-weight:500;src:url(“https://media.inquirer.com/fonts/InquirerHeadline-MediumWEB.woff2”) format(“woff2”),url(“https://media.inquirer.com/fonts/InquirerHeadline-MediumWEB.woff”) format(“woff”)}@font-face{font-family:”Inquirer Headline”;font-weight:500;font-style:italic;src:url(“https://media.inquirer.com/fonts/InquirerHeadline-MediumItalicWEB.woff2”) format(“woff2”),url(“https://media.inquirer.com/fonts/InquirerHeadline-MediumItalicWEB.woff”) format(“woff”)}@font-face{font-family:”Inquirer Headline”;font-weight:600;src:url(“https://media.inquirer.com/fonts/InquirerHeadline-SemiBoldWEB.woff2”) format(“woff2”),url(“https://media.inquirer.com/fonts/InquirerHeadline-SemiBoldWEB.woff”) format(“woff”)}@font-face{font-family:”Inquirer Headline”;font-weight:600;font-style:italic;src:url(“https://media.inquirer.com/fonts/InquirerHeadline-SemiBoldItalicWEB.woff2”) format(“woff2”),url(“https://media.inquirer.com/fonts/InquirerHeadline-SemiBoldItalicWEB.woff”) format(“woff”)}@font-face{font-family:”Inquirer Headline”;font-weight:700;src:url(“https://media.inquirer.com/fonts/InquirerHeadline-BoldWEB.woff2”) format(“woff2”),url(“https://media.inquirer.com/fonts/InquirerHeadline-BoldWEB.woff”) format(“woff”)}@font-face{font-family:”Inquirer Headline”;font-weight:700;font-style:italic;src:url(“https://media.inquirer.com/fonts/InquirerHeadline-BoldItalicWEB.woff2”) format(“woff2”),url(“https://media.inquirer.com/fonts/InquirerHeadline-BoldItalicWEB.woff”) format(“woff”)}@font-face{font-family:”Inquirer Headline”;font-weight:900;src:url(“https://media.inquirer.com/fonts/InquirerHeadline-BlackWEB.woff2”) format(“woff2”),url(“https://media.inquirer.com/fonts/InquirerHeadline-BlackWEB.woff”) format(“woff”)}@font-face{font-family:”Inquirer Headline”;font-weight:900;font-style:italic;src:url(“https://media.inquirer.com/fonts/InquirerHeadline-BlackItalicWEB.woff2”) format(“woff2”),url(“https://media.inquirer.com/fonts/InquirerHeadline-BlackItalicWEB.woff”) format(“woff”)}@font-face{font-family:”Inquirer Text”;font-weight:normal;src:url(“https://media.inquirer.com/fonts/InquirerTextWEB-RegularWEB.woff2”) format(“woff2”),url(“https://media.inquirer.com/fonts/InquirerTextWEB-RegularWEB.woff”) format(“woff”)}@font-face{font-family:”Inquirer Text”;font-weight:normal;font-style:italic;src:url(“https://media.inquirer.com/fonts/InquirerTextWEB-RegularItalicWEB.woff2”) format(“woff2”),url(“https://media.inquirer.com/fonts/InquirerTextWEB-RegularItalicWEB.woff”) format(“woff”)}@font-face{font-family:”Inquirer Text”;font-weight:bold;src:url(“https://media.inquirer.com/fonts/InquirerTextWEB-BoldWEB.woff2”) format(“woff2”),url(“https://media.inquirer.com/fonts/InquirerTextWEB-BoldWEB.woff”) format(“woff”)}@font-face{font-family:”Inquirer Text”;font-weight:bold;font-style:italic;src:url(“https://media.inquirer.com/fonts/InquirerTextWEB-BoldItalicWEB.woff2”) format(“woff2”),url(“https://media.inquirer.com/fonts/InquirerTextWEB-BoldItalicWEB.woff”) format(“woff”)}@font-face{font-family:”Grot 10″;font-weight:normal;src:url(“https://media.inquirer.com/fonts/Grot10-RegularWEB.woff2”) format(“woff2”),url(“https://media.inquirer.com/fonts/Grot10-RegularWEB.woff”) format(“woff”)}@font-face{font-family:”Grot 10″;font-weight:500;src:url(“https://media.inquirer.com/fonts/Grot10-MediumWEB.woff2”) format(“woff2”),url(“https://media.inquirer.com/fonts/Grot10-MediumWEB.woff”) format(“woff”)}@font-face{font-family:”Grot 10″;font-weight:bold;src:url(“https://media.inquirer.com/fonts/Grot10-ExtraboldWEB.woff2”) format(“woff2”),url(“https://media.inquirer.com/fonts/Grot10-ExtraboldWEB.woff”) format(“woff”)}@font-face{font-family:”Grot12″;font-weight:300;src:url(“https://media.inquirer.com/fonts/Grot12Condensed-LightWEB.woff2”) format(“woff2”),url(“https://media.inquirer.com/fonts/Grot12Condensed-LightWEB.woff”) format(“woff”)}@font-face{font-family:”Grot12″;font-weight:600;src:url(“https://media.inquirer.com/fonts/Grot12Condensed-SemiboldWEB.woff2”) format(“woff2”),url(“https://media.inquirer.com/fonts/Grot12Condensed-SemiboldWEB.woff”) format(“woff”)}body.is-scroll-locked{overflow:hidden;height:100%}.inno{-webkit-font-smoothing:antialiased;-moz-osx-font-smoothing:grayscale;font-family:”Grot 10″,sans-serif;color:#222;padding-block-end:64px;overflow:clip;font-size:14px;line-height:1}.inno–widget,.inno–embed{overflow:hidden;padding-block-end:0}.inno–widget .inno-layout–content>*,.inno–embed .inno-layout–content>*{max-width:none}.inno-anchorable:before{content:””;display:block;height:calc(var(–nav-height, 0) + 10px);margin:calc(0px – (var(–nav-height, 0) + 10px)) 0 0}.inno-spanner{padding:0 2px;margin:0 -2px;color:#222;font-family:”Grot 10″,sans-serif;font-weight:bold;font-size:16px}@media(min-width: 48em){.inno-spanner{font-size:18px}}.inno-spanner[data-populate=”27_22k_noEPTC”],.inno-spanner[data-populate=”27_35k_yesEPTC”],.inno-spanner[data-populate=”27_35k_noEPTC”],.inno-spanner[data-populate=”27_65k_noEPTC”],.inno-spanner[data-populate=”60_65k_noEPTC”]{font-weight:500}.inno-spanner–fulton-county,.inno-spanner–camden-county{font-family:”Inquirer Headline”,”Times New Roman”,serif;font-weight:600;padding:0;margin:0;font-size:18px}@media(min-width: 48em){.inno-spanner–fulton-county,.inno-spanner–camden-county{font-size:20px}}.inno-spanner–error,.inno-spanner–error-invalid-symbol{background-color:#fff;border:3px dashed #e11b22;box-shadow:none;padding-left:4px;padding-right:4px}.inno{–gutter: calc(50vw – 325px)}.inno *{box-sizing:border-box}.inno-layout–content>*{max-width:min(650px,100vw – 32px);margin-inline:auto}.inno-layout–align-full{max-width:100%}.inno-layout–align-wide{max-width:min(1250px,100vw – 32px);margin-inline:auto}.inno-layout–align-default{max-width:min(650px,100vw – 32px);margin-inline:auto}@media(min-width: 48em){.inno-layout–align-left{float:left;margin-inline-start:var(–gutter);margin-inline-end:24px;width:301px;margin-block-end:16px;padding-top:6px}}@media(min-width: 60em){.inno-layout–align-left{margin-inline-start:calc(var(–gutter) – clamp(0px,var(–gutter) – 100px,160px))}}@media(min-width: 48em){.inno-layout–align-right{float:right;width:301px;margin-inline-start:24px;margin-inline-end:var(–gutter);margin-block-end:16px;padding-top:5px}}@media(min-width: 60em){.inno-layout–align-right{margin-inline-end:calc(var(–gutter) – clamp(0px,var(–gutter) – 100px,160px))}}.inno-layout–stack>*+*{margin-block-start:24px}.inno-layout–stack-tight>*+*{margin-block-start:10px}.inno-layout–stack-loose>*+*{margin-block-start:30px}*+.inno-layout–isolate{margin-block-start:48px}.inno-layout–isolate+*{margin-block-start:48px}.inno-arrow-chart{position:relative;margin:0 auto;max-width:600px;display:flex;flex-direction:column;align-items:center;justify-content:center;width:100%;aspect-ratio:2/3.5}@media(min-width: 37.5em){.inno-arrow-chart{aspect-ratio:2/2.5;margin:0 16px}}@media(min-width: 48em){.inno-arrow-chart{max-width:1200px}}@media(min-width: 60em){.inno-arrow-chart{aspect-ratio:3/2}}.inno-arrow-chart__title{text-anchor:middle;font-size:16px;fill:#222;font-family:”Inquirer Headline”,”Times New Roman”,serif;font-weight:600}.inno-arrow-chart__title–2{font-size:24px}@media(min-width: 37.5em){.inno-arrow-chart__title{font-size:18px}.inno-arrow-chart__title–2{font-size:24px}}.inno-arrow-chart__axis-title{font-size:16px;font-family:”Grot12″,sans-serif;font-weight:bold;text-anchor:middle}@media(min-width: 37.5em){.inno-arrow-chart__axis-title{font-size:18px}}.inno-arrow-chart__x-axis .domain,.inno-arrow-chart__y-axis .domain{display:none}.inno-arrow-chart__svg{top:0;left:0;width:100%;height:100%;position:absolute;z-index:1}.inno-arrow-chart__line{stroke-width:4px;opacity:1}.inno-arrow-chart__x-axis-label,.inno-arrow-chart__y-axis-label{font-size:12px;font-family:”Grot 10″,sans-serif;color:#808284}@media(min-width: 37.5em){.inno-arrow-chart__x-axis-label,.inno-arrow-chart__y-axis-label{font-size:16px}}.inno-arrow-chart__x-axis-label–age-27,.inno-arrow-chart__x-axis-label–age-40,.inno-arrow-chart__x-axis-label–age-60,.inno-arrow-chart__y-axis-label–age-27,.inno-arrow-chart__y-axis-label–age-40,.inno-arrow-chart__y-axis-label–age-60{font-size:16px;font-weight:bold;color:#595760}@media(min-width: 37.5em){.inno-arrow-chart__x-axis-label–age-27,.inno-arrow-chart__x-axis-label–age-40,.inno-arrow-chart__x-axis-label–age-60,.inno-arrow-chart__y-axis-label–age-27,.inno-arrow-chart__y-axis-label–age-40,.inno-arrow-chart__y-axis-label–age-60{font-size:20px}}.inno-arrow-chart__y-axis-line{display:none}.inno-arrow-chart__y-axis-line–age-27,.inno-arrow-chart__y-axis-line–age-40,.inno-arrow-chart__y-axis-line–age-60{display:none}.inno-arrow-chartfboldz__label-end,.inno-arrow-chart__label-delta{font-family:”Grot 10″,sans-serif;text-anchor:start;font-size:12px}@media(min-width: 37.5em){.inno-arrow-chartfboldz__label-end,.inno-arrow-chart__label-delta{font-size:16px}}.inno-arrow-chart__label-delta{font-weight:bold;text-anchor:middle}.inno-arrow-chart__label-delta.inno-arrow-chart__label-delta-none{font-size:14px;text-transform:uppercase;font-family:”Grot12″,sans-serif}.inno-arrow-chart__x-axis-line,.inno-arrow-chart__grid-x .tick line{stroke:#222;stroke-opacity:.2;shape-rendering:crispEdges}.inno-arrow-chart__grid-x path.domain{display:none}.inno-select-county{display:inline-block;margin:0}.inno-select-county__select{border:1px solid #dcdcdc;font-family:”Inquirer Headline”,”Times New Roman”,serif;font-weight:600;font-size:18px;width:100%;padding:5px;border-radius:4px}@supports(field-sizing: content){.inno-select-county__select{field-sizing:content}}.inno-select-county__select:focus,.inno-select-county__select:active,.inno-select-county__select:focus-visible{border-color:#e11b22;outline:0}.inno-adbox{max-height:400px;transition:max-height .4s ease-in-out,padding .4s ease-in-out,margin .4s ease-in-out;overflow:hidden}.inno-adbox.is-hidden{max-height:0;margin:0;padding:0}.inno-adbox–banner{padding-block:48px;background:#222}@media(min-width: 0em)and (max-width: 48em){.inno-adbox–banner{display:none}}.inno-adbox–banner .inno-adbox__label{display:none}.inno-color–white .inno-adbox–banner{background:#f4f1eb}.inno-color–white .inno-adbox–banner .inno-ad__ad{background:#fff}.inno-color–black .inno-adbox–banner{background:rgb(54.4,54.4,54.4)}.inno-adbox__label{display:block;margin:0 auto 8px;text-align:center;font-size:12px;color:#808284;text-transform:uppercase}.inno-ad__ad{margin-inline:auto;background-color:#f4f1eb;display:flex;align-items:center;justify-content:center;overflow:hidden;width:300px;height:250px}@media(min-width: 48em){.inno-ad__ad{width:728px;height:90px}}@media(min-width: 63.9375em){.inno-ad__ad{height:auto;width:fit-content;min-width:728px;min-height:90px;max-width:970px;max-height:250px}}.inno-ad__ad–small{width:300px;height:250px;min-height:auto;min-width:auto}.inno-ad__ad iframe{position:unset !important}.inno-ad__ad .cnx-content-wrapper{position:relative !important}.inno-ad__ad .celtra-ad-inline-host,.inno-ad__ad .celtra-ad-inline-host *{position:relative !important;overflow:hidden !important}.inno-ad__placeholder{text-align:center;text-transform:uppercase;font-weight:bold;font-size:16px;color:#222}@media(min-width: 75em){.inno-ad__placeholder{padding:120px 0}}.inno-body__error{color:var(–color-text-primary);padding:24px;border:3px dashed #e11b22;font-family:monospace;white-space:pre-wrap;font-size:16px}.inno-body__error-head{display:block;font-weight:bold}.inno-button{position:relative;display:flex;flex-direction:row;justify-content:center;align-items:center;gap:8px;box-sizing:border-box;text-decoration:none;border-radius:4px;cursor:pointer;pointer-events:auto;transition:background-color .4s ease-in-out,border-color .4s ease-in-out,color .4s ease-in-out;background-color:var(–color-accent);color:var(–color-over-accent)}.inno-button:focus{outline:solid 4px var(–color-text-tertiary)}.inno-button:disabled{pointer-events:none}.inno-button–primary:hover{background-color:var(–color-text-primary);color:var(–color-background)}.inno-button–primary:disabled{background-color:var(–color-text-secondary);color:var(–color-text-tertiary);pointer-events:none}.inno-button–secondary{background-color:var(–color-background);color:var(–color-text-primary);border:solid 1px var(–color-accent)}.inno-button–secondary:hover{background-color:var(–color-accent);color:var(–color-over-accent);border:solid 1px var(–color-accent)}.inno-button–secondary:disabled{border-color:var(–color-text-tertiary);color:var(–color-text-tertiary)}.inno-button–minimal{background-color:rgba(0,0,0,0);color:var(–color-text-primary);padding:8px}.inno-button–minimal:hover{background-color:var(–color-accent);color:var(–color-over-accent)}.inno-button–minimal:hover .inno-button__label{opacity:1}.inno-button–minimal:disabled{background-color:var(–color-text-secondary);color:var(–color-text-tertiary);pointer-events:none}.inno-button–large{padding:16px 40px}.inno-button–medium{padding:10px 24px}.inno-button–small{padding:8px 16px}.inno-button–round{border-radius:99px}.inno-button–round.inno-button–small{padding:8px}.inno-button–round.inno-button–medium{padding:10px}.inno-button–round.inno-button–large{padding:16px}.inno-button__label{font-family:”Grot 10″,sans-serif;font-weight:700;line-height:1.2em;flex-grow:0;z-index:1}.inno-button–large .inno-button__label{font-size:20px}.inno-button–medium .inno-button__label{font-size:18px}.inno-button–small .inno-button__label{font-size:16px}.inno-button–has-image .inno-button__label{text-align:center}.inno-button__image{margin:0 auto;object-fit:contain}.inno-byline{border-block:1px solid var(–color-faint);padding-block:16px;font-family:”Grot 10″,sans-serif;font-size:14px;line-height:1.5}.inno-byline–center{border-block:none;padding-block:0}@media(min-width: 48em){.inno-byline{font-size:16px}}.inno-byline__content{display:flex;justify-content:space-between;align-items:center;gap:12px}.inno-byline–center .inno-byline__content{flex-direction:column;text-align:center}.inno-byline__text{flex:1 1 auto}.inno-byline .inno-gift{flex:0 0 auto}.inno-byline__timestamp-date{color:var(–color-text-primary)}.inno-byline__timestamp-label{color:var(–color-text-secondary)}.inno-byline__authors{color:var(–color-text-primary, #222222);line-height:1.5em;text-wrap-style:balance}.inno-byline__author{display:inline}.inno-byline__author-link,.inno-byline__authors a{color:var(–color-text-primary, #222222);text-decoration:none;transition:color .4s ease-in-out}.inno-byline__author-link:hover,.inno-byline__authors a:hover{color:var(–color-text-link, #004e96)}.inno-callout__content{padding:20px 15px;background-color:#fff;border:1px solid var(–color-faint)}.inno-callout:has(.inno-callout__cta) .inno-callout__content{padding-bottom:50px}.inno-callout__tag{font-family:”Grot 10″,sans-serif;font-size:16px;color:var(–color-text-primary)}@media(min-width: 48em){.inno-callout__tag{font-size:18px}}.inno-callout__title{font-family:”Grot12″,sans-serif;font-size:32px;font-weight:bold;text-transform:uppercase;color:var(–color-text-primary);text-wrap:balance}*+.inno-callout__title{margin-block-start:5px}.inno-callout__body{font-family:”Grot 10″,sans-serif;font-size:16px;color:var(–color-text-primary);line-height:1.65em}@media(min-width: 48em){.inno-callout__body{font-size:18px}}*+.inno-callout__body{margin-block-start:10px}.inno-callout__body .inno-p{font-family:inherit;font-size:inherit;color:inherit;line-height:inherit}.inno-callout__cta{display:flex;width:calc(100% – 30px);margin:-30px 15px 0 15px}.inno-callout__cta .inno-button{box-shadow:0 1px 4px rgba(89,87,96,.1),0 3px 6px rgba(89,87,96,.1);padding:20px 20px}.inno-callout__form-policy{font-size:15.2px;margin-top:20px;color:#808284;line-height:1.65}.inno-callout__form-policy a{color:#808284;transition:color .3s ease-in-out}.inno-callout__form-policy a:hover{color:var(–color-text-primary)}.inno-caption{color:var(–color-text-secondary);font-family:”Grot 10″,sans-serif;font-size:14px;line-height:1.5}.inno-caption a{color:inherit;box-shadow:inset 0 -1px 0 0 var(–color-text-secondary);transition:color .25s ease,box-shadow .25s ease;text-decoration:none}.inno-caption a:hover{color:var(–color-text-link);box-shadow:inset 0 -1px 0 0 var(–color-text-link)}.inno-caption__caption-text{display:block;text-wrap:pretty}.inno-caption__credit{color:var(–color-text-tertiary);display:block}.inno-credits{font-family:”Grot 10″,sans-serif}.inno-credits__header{color:var(–color-text-primary);font-size:16px;font-family:”Grot 10″,sans-serif;font-weight:normal;line-height:1.2;border-bottom:1px solid var(–color-faint);padding-bottom:4px;margin-bottom:8px}.inno-credits__roles{display:grid;gap:8px;color:var(–color-text-secondary);font-size:14px;line-height:1.5;text-align:pretty}@media(min-width: 48em){.inno-credits__roles{grid-template-columns:50% 50%}}.inno-gift{display:none}.inno-gift–default{justify-content:center}.inno-gift–default.is-available{display:flex}.inno-gift–default .inno-button{font-size:24px;padding:8px;min-width:200px;margin:0px auto}.inno-gift–minimal.is-available{display:inline-block}.inno-gift–minimal .inno-button{display:flex;align-items:center;font-size:16px;line-height:16px}.inno-gift–minimal .inno-button__label{font-size:14px;font-weight:normal;color:currentColor;opacity:.4;transition:opacity .4s ease-in-out;display:none}@media(min-width: 37.5em){.inno-gift–minimal .inno-button__label{display:inline-block}}.inno-gift–minimal .inno-icon{display:inline-block}.inno-gift.is-available{display:block}.is-app .inno-gift{display:none}.inno-gift .inno-icon–loading{animation:spin 1s linear forwards infinite}.inno-gift .inno-icon{display:none}.inno-gift [data-state=ready] .inno-icon–gift{display:initial}.inno-gift [data-state=loading] .inno-icon–loading{display:initial}.inno-gift [data-state=complete] .inno-icon–tickmark{display:initial}.inno-gift [data-state=error] .inno-icon–cross{display:initial}.inno-gift-toast-receiver{display:none}@keyframes spin{0%{rotate:0deg}100%{rotate:360deg}}.inno-graphic__iframe,.inno-graphic__datawrapper{width:100%}.inno-heading{font-family:”Inquirer Headline”,”Times New Roman”,serif;font-size:24px;font-weight:600;line-height:1.2;color:var(–color-text-primary);scroll-margin-top:calc(var(–sticky-height) + 16px);text-wrap:balance}@media(min-width: 48em){.inno-heading{font-size:36px}}.inno-heading–chapter{font-weight:300;border-bottom:1px solid var(–color-text-primary);text-transform:uppercase}.inno-layout–stack>*+.inno-heading{margin-block-start:48px}.inno-layout–stack>.inno-heading:has(+*){margin-block-end:-12px}.inno-layout–stack-tight>*+.inno-heading{margin-block-start:20px}.inno-layout–stack-tight>.inno-heading:has(+*){margin-block-end:-5px}.inno-layout–stack-loose>*+.inno-heading{margin-block-start:60px}.inno-layout–stack-loose>.inno-heading:has(+*){margin-block-end:-15px}.inno-hero{margin-block-start:0}.inno-hero–has-media .inno-hero__content{padding-bottom:72px}@media(min-width: 60em){.inno-hero–has-media .inno-hero__content{padding-bottom:128px}}.inno-color–white .inno-hero,.inno-mode–light .inno-hero–style-transparent{–color-accent: #ffffff;–color-over-accent: #222222}.inno-color–black .inno-hero,.inno-mode–dark .inno-hero–style-transparent{–color-accent: #222222;–color-over-accent: #ffffff}.inno-hero–style-transparent .inno-hero__content{background:rgba(0,0,0,0)}.inno-hero–layout-above{display:flex;flex-direction:column-reverse;background:var(–color-accent)}.inno-hero–layout-above .inno-hero__content{padding:24px 0}.inno-hero–layout-above .inno-hero__media{max-width:80%;margin:0 auto;padding-top:24px}.inno-hero–layout-above .inno-hero__media>*{max-width:350px}.inno-hero–layout-above .inno-hero__media .inno-caption{display:none}.inno-hero__content{padding-block:24px;text-align:center;background:var(–color-background);color:var(–color-over-accent)}@media(min-width: 60em){.inno-hero__content{padding-block:32px}}.inno-hero__eyebrow{font-family:”Grot12″,sans-serif;font-weight:bold;text-transform:uppercase;font-size:16px;font-weight:bold;padding:5px 8px;background:var(–color-over-accent);color:var(–color-accent);width:max-content;text-decoration:none;line-height:2}@media(min-width: 48em){.inno-hero__eyebrow{font-size:18px}}.inno-hero__icon{margin:auto;max-width:200px}.inno-hero__icon img{width:100%;height:auto}@media(min-width: 48em){.inno-hero__icon{max-width:250px}}.inno-hero__headline{font-family:”Inquirer Headline”,”Times New Roman”,serif;font-size:40px;font-weight:600;line-height:1;text-wrap:balance}@media(min-width: 48em){.inno-hero__headline{font-size:52px}}.inno-hero__subheadline{font-family:”Inquirer Headline”,”Times New Roman”,serif;font-size:20px;line-height:1.3;text-wrap:balance}@media(min-width: 48em){.inno-hero__subheadline{font-size:24px}}.inno-hero__media{position:relative;z-index:2;margin-top:-48px}@media(min-width: 60em){.inno-hero__media{margin-top:-96px}}.inno-hero__arrow{stroke-dasharray:1000;stroke-dashoffset:1000;animation:draw 2s ease forwards;animation-delay:.8s}.inno-hero__arrowhead{opacity:0;animation:arrowIn .4s ease-in-out forwards;animation-delay:1.6s}.inno-hero__state{opacity:0;animation:arrowIn .6s ease-in-out forwards}.inno-hero__state–de{animation-delay:.8s}.inno-hero__state–pa{animation-delay:1s}.inno-hero__state–nj{animation-delay:1.2s}@keyframes draw{to{stroke-dashoffset:0}}@keyframes arrowIn{to{opacity:1}}.inno-hover{position:relative;cursor:pointer;border:1px var(–color-accent) solid;padding:3px 4px;transition:border .4s ease-in-out;box-sizing:border-box}@media(min-width: 48em){.inno-hover{cursor:help}}.inno-hover:hover{border:1px var(–color-accent) solid}.inno-hover__box{position:fixed;bottom:0;left:0;right:0;z-index:20;background-color:var(–color-background);pointer-events:none;transform:translateY(100%);transition:transform .4s ease-in-out;padding:16px;border-top:1px solid var(–color-accent);white-space:normal;font-family:”Grot 10″,sans-serif;font-size:14px;line-height:1.5}@media(min-width: 48em){.inno-hover__box{position:absolute;top:100%;width:200px;left:-1px;right:0;bottom:auto;margin:auto;max-width:250px;padding:6px;opacity:0;transition:opacity .4s ease-in-out;transform:none;border:1px solid var(–color-accent)}}.inno-hover.is-visible .inno-hover__box{opacity:1;transform:translateY(0)}.inno-icon{display:inline-block;width:1.2em;height:1.2em;fill:currentColor}.inno-icon–white{fill:#fff}.inno-icon–black{fill:#222}.inno-icon–accent{fill:var(–color-accent)}.inno-icon–over-accent{fill:var(–color-over-accent)}.inno-icon__stroke{fill:rgba(0,0,0,0);stroke:currentColor;stroke-width:2px;vector-effect:non-scaling-stroke}.inno-icon–white .inno-icon__stroke{stroke:#fff}.inno-icon–black .inno-icon__stroke{stroke:#222}.inno-icon–accent .inno-icon__stroke{stroke:var(–color-accent)}.inno-icon–over-accent .inno-icon__stroke{stroke:var(–color-over-accent)}.inno-image__img{width:100%;display:block}.inno-looping-video__video{width:100%}.inno-note .inno-p{color:var(–color-text-secondary);font-family:”Grot 10″,sans-serif;font-size:14px;-webkit-font-smoothing:antialiased;line-height:1.5}.inno-note .inno-p a{color:var(–color-text-secondary);box-shadow:inset 0 -1px 0 0 var(–color-text-secondary);transition:color .25s ease}.inno-note .inno-p a:hover{color:#004e96;box-shadow:inset 0 -1px 0 0 #004e96}.inno-note .inno-heading{color:var(–color-text-primary);font-family:”Grot 10″,sans-serif;font-size:16px;font-weight:normal;text-transform:none;border-bottom:1px solid var(–color-faint);padding-bottom:4px}.inno-p{-webkit-font-smoothing:subpixel-antialiased;-mox-osx-font-smoothing:grayscale;color:#222;color:var(–color-text-primary);font-family:”Inquirer Text”,”Times New Roman”,serif;font-size:18px;line-height:1.666666;white-space:pre-line;text-wrap:pretty}@media(min-width: 37.5em){.inno-p{font-size:20px;line-height:1.6}}.inno-p–has-dropcap:first-letter{margin-top:1px;margin-right:12px;margin-bottom:0;margin-left:0;font-family:”Inquirer Headline”,”Times New Roman”,serif;font-size:3.2em;float:left;font-weight:bold;line-height:1;color:var(–color-text-accent)}@-moz-document url-prefix(){.inno-p–has-dropcap:first-letter{margin-top:10px;margin-bottom:0px}}@media(min-width: 37.5em){.inno-p–has-dropcap:first-letter{font-size:5.3em;margin-top:-3px;margin-bottom:-10px}@-moz-document url-prefix(){.inno-p–has-dropcap:first-letter{margin-top:12px;margin-bottom:0px}}}.inno-p a{transition:box-shadow .25s ease;color:var(–color-text-link);text-decoration:none}.inno-p a:hover{box-shadow:inset 0 -1px 0 0 var(–color-text-link)}.inno-p__endmark{display:inline-block;height:1.1em;width:1.1em;margin-left:5px;vertical-align:text-bottom;margin-bottom:2px;fill:var(–color-text-accent)}.inno-premium{padding:19px 26px 22px 8px;color:var(–color-text-primary);font-family:”Grot 10″,sans-serif;font-size:18px;line-height:1;font-weight:normal;background-color:var(–color-background-secondary)}.inno-premium .inno-icon{fill:#f0af13;width:24px;margin-right:7px}.inno-premium__header{display:flex}.inno-premium__hed{font-weight:bold;line-height:22px;font-size:16px;color:var(–color-text-primary);padding:3px 0 4px;font-family:”Grot 10″,sans-serif;text-wrap:pretty}.inno-mode–dark .inno-premium__hed{color:#fff}.inno-premium__message{font-weight:500;line-height:22px;font-size:16px;color:var(–color-text-secondary);font-family:”Grot 10″,sans-serif;margin-left:32px;text-wrap:pretty}.inno-settings{–color-background: #f4f1eb;–color-background-secondary: #f4f1eb;–color-accent: #004e96;–color-over-accent: #ffffff;–color-text-primary: #222222;–color-text-link: #1a6aff;–color-text-secondary: #595760;–color-text-tertiary: #808284;–color-text-accent: #004e96;–color-faint: #dcdcdc;–color-mask: rgba(34, 34, 34, 0.8);background:var(–color-background);color:var(–color-text-primary)}.inno-mode–dark{–color-background: #222222;–color-background-secondary: #595760;–color-accent: #8dd7f7;–color-over-accent: #222222;–color-text-primary: #ffffff;–color-text-secondary: #dcdcdc;–color-text-tertiary: #808284;–color-text-link: #8dd7f7;–color-faint: #595760;–color-mask: rgba(255, 255, 255, 0.8)}.inno-color–purple{–color-accent: #7b2589;–color-over-accent: #ffffff;–color-text-accent: #7b2589}.inno-color–pink{–color-accent: #cd0785;–color-over-accent: #ffffff;–color-text-accent: #cd0785}.inno-color–red{–color-accent: #e11b22;–color-over-accent: #ffffff;–color-text-accent: #e11b22}.inno-color–orange{–color-accent: #e66a1f;–color-over-accent: #222222;–color-text-accent: #e66a1f}.inno-color–yellow{–color-accent: #f0af13;–color-over-accent: #222222;–color-text-accent: #f0af13}.inno-color–green{–color-accent: #00a253;–color-over-accent: #ffffff;–color-text-accent: #00a253}.inno-color–teal{–color-accent: #00a69e;–color-over-accent: #ffffff;–color-text-accent: #00a69e}.inno-color–light-gray{–color-accent: #dcdcdc;–color-over-accent: #222222;–color-text-accent: #dcdcdc}.inno-color–light-blue{–color-accent: #8dd7f7;–color-over-accent: #222222;–color-text-accent: #8dd7f7}.inno-color–blue{–color-accent: #004e96;–color-over-accent: #ffffff;–color-text-accent: #004e96}.inno-color–black{–color-accent: #222222;–color-over-accent: #ffffff;–color-text-accent: #222222}.inno-color–white{–color-accent: #ffffff;–color-over-accent: #222222;–color-text-accent: #ffffff}.inno-color–white,.inno-color–black{–color-accent: #004e96;–color-over-accent: #ffffff;–color-text-accent: #222222}.inno-color–white.inno-mode–dark,.inno-color–black.inno-mode–dark{–color-accent: #8dd7f7;–color-over-accent: #222222;–color-text-accent: #ffffff}body:has(.inno-chrome–chromeless){overflow:hidden;width:100vw;height:100vh}@supports(width: 100dvw){body:has(.inno-chrome–chromeless){width:100dvw}}@supports(height: 100dvh){body:has(.inno-chrome–chromeless){height:100dvh}}body:has(.inno-chrome–chromeless) .global-app-bar,body:has(.inno-chrome–chromeless) .footer,body:has(.inno-chrome–chromeless) .footer-wrapper{display:none}body:has(.inno-chrome–chromeless) #inq-article-completion{height:0px}.inno-heading{font-family:”Inquirer Headline”,”Times New Roman”,serif;font-size:24px;font-weight:600;line-height:1.2;color:var(–color-text-primary);scroll-margin-top:calc(var(–sticky-height) + 16px);text-wrap:balance}@media(min-width: 48em){.inno-heading{font-size:36px}}.inno-heading–chapter{font-weight:300;border-bottom:1px solid var(–color-text-primary);text-transform:uppercase}.inno-layout–stack>*+.inno-heading{margin-block-start:48px}.inno-layout–stack>.inno-heading:has(+*){margin-block-end:-12px}.inno-layout–stack-tight>*+.inno-heading{margin-block-start:20px}.inno-layout–stack-tight>.inno-heading:has(+*){margin-block-end:-5px}.inno-layout–stack-loose>*+.inno-heading{margin-block-start:60px}.inno-layout–stack-loose>.inno-heading:has(+*){margin-block-end:-15px}.inno-image__img{width:100%;display:block}.inno-steps__steps{margin-top:-20vh;padding-bottom:80vh}.inno-steps__step{position:relative;z-index:2;-webkit-transform:translate3d(0, 0, 0);margin:70vh auto;padding:8px;background-color:var(–color-background);border:var(–color-faint) 1px solid;overflow:auto;max-width:min(100% – 32px,650px)}@media(min-width: 37.5em){.inno-steps__step{padding:12px;margin:70vh auto}}.inno-steps__step:first-of-type{margin-top:-60vh}.inno-steps__step:last-of-type{margin-bottom:0}.inno-steps__step–transparent{background-color:rgba(0,0,0,0);box-shadow:none}@media(min-width: 60em){.inno-steps__step–left{width:calc(50vw – 32px);margin-left:auto;margin-right:calc(50% + 16px)}}@media(min-width: 60em){.inno-steps__step–right{width:calc(50vw – 32px);margin-right:auto;margin-left:calc(50% + 16px)}}.inno-steps__step–full{max-width:none;width:100%;padding:24px 0;border-left:none;border-right:none}.inno-steps__step–full .inno-steps__body{max-width:100%;margin:0 auto}.inno-steps__step–full .inno-steps__body>*:not([class*=inno-layout–align-]){max-width:min(100% – 32px,650px);margin-inline:auto}.inno-steps__step .inno-hero__content{background-color:rgba(0,0,0,0);color:var(–color-text-primary)}.inno-steps__step .inno-caption{padding-top:6px;border-top:1px solid #dcdcdc}.inno-steps__step .inno-byline{border-top:0;border-bottom:0;padding:0;margin-block-start:0;text-align:center}.inno-steps__step .inno-byline__content{flex-direction:column}.inno-steps__step .inno-premium{display:none}.inno-steps__step .inno-steps__body+.inno-caption{margin-top:6px}.inno-steps__content{position:sticky;height:100vh;width:100%;top:0;left:0;right:0;margin:auto;display:flex;align-items:center;justify-content:center;overflow:hidden;isolation:isolate;z-index:1;background-color:#fff}@supports(height: 100dvh){.inno-steps__content{height:100dvh}}.inno-steps__custom{z-index:1;position:absolute;width:100vw;height:100%;top:0;left:0;right:0;bottom:0;margin:auto;display:flex;align-items:center;justify-content:center}@media(min-width: 60em){.inno-steps__custom–left{width:50%;right:auto}}@media(min-width: 60em){.inno-steps__custom–right{width:50%;left:auto}}.inno-steps__custom:empty{display:none;pointer-events:none}.inno-steps__background{position:absolute;object-fit:cover;inset:0;opacity:0;transition:opacity .4s ease-in-out;z-index:0;background-color:var(–color-background);display:flex;justify-content:center;align-items:center}.inno-steps__background .inno-graphic{width:100%}.inno-steps__background .inno-looping-video,.inno-steps__background .inno-image{width:100%;height:100%}.inno-steps__background .inno-looping-video__video,.inno-steps__background .inno-image__img{height:100%;width:100%;object-position:center;object-fit:cover}.inno-steps__background–contain{background-color:var(–color-background);padding:8px}@media(min-width: 48em){.inno-steps__background–contain{padding:16px}}.inno-steps__background–contain .inno-looping-video__video,.inno-steps__background–contain .inno-image__img{object-fit:contain}.inno-steps__background–left .inno-image__img{object-fit:contain}@media(min-width: 60em){.inno-steps__background–left{width:50%;right:auto}}.inno-steps__background–right .inno-image__img{object-fit:contain}@media(min-width: 60em){.inno-steps__background–right{width:50%;left:auto}}.inno-steps–has-backgrounds[data-index=”-1″] .inno-steps__background–0{opacity:1;z-index:1}.inno-steps–has-backgrounds[data-index=”0″] .inno-steps__background–0{opacity:1;z-index:1}.inno-steps–has-backgrounds[data-index=”1″] .inno-steps__background–1{opacity:1;z-index:1}.inno-steps–has-backgrounds[data-index=”2″] .inno-steps__background–2{opacity:1;z-index:1}.inno-steps–has-backgrounds[data-index=”3″] .inno-steps__background–3{opacity:1;z-index:1}.inno-steps–has-backgrounds[data-index=”4″] .inno-steps__background–4{opacity:1;z-index:1}.inno-steps–has-backgrounds[data-index=”5″] .inno-steps__background–5{opacity:1;z-index:1}.inno-steps–has-backgrounds[data-index=”6″] .inno-steps__background–6{opacity:1;z-index:1}.inno-steps–has-backgrounds[data-index=”7″] .inno-steps__background–7{opacity:1;z-index:1}.inno-steps–has-backgrounds[data-index=”8″] .inno-steps__background–8{opacity:1;z-index:1}.inno-steps–has-backgrounds[data-index=”9″] .inno-steps__background–9{opacity:1;z-index:1}.inno-steps–has-backgrounds[data-index=”10″] .inno-steps__background–10{opacity:1;z-index:1}.inno-steps–has-backgrounds[data-index=”11″] .inno-steps__background–11{opacity:1;z-index:1}.inno-steps–has-backgrounds[data-index=”12″] .inno-steps__background–12{opacity:1;z-index:1}.inno-steps–has-backgrounds[data-index=”13″] .inno-steps__background–13{opacity:1;z-index:1}.inno-steps–has-backgrounds[data-index=”14″] .inno-steps__background–14{opacity:1;z-index:1}.inno-steps–has-backgrounds[data-index=”15″] .inno-steps__background–15{opacity:1;z-index:1}.inno-steps–has-backgrounds[data-index=”16″] .inno-steps__background–16{opacity:1;z-index:1}.inno-steps–has-backgrounds[data-index=”17″] .inno-steps__background–17{opacity:1;z-index:1}.inno-steps–has-backgrounds[data-index=”18″] .inno-steps__background–18{opacity:1;z-index:1}.inno-steps–has-backgrounds[data-index=”19″] .inno-steps__background–19{opacity:1;z-index:1}.inno-steps–has-backgrounds[data-index=”20″] .inno-steps__background–20{opacity:1;z-index:1}.inno-steps–has-backgrounds[data-index=”21″] .inno-steps__background–21{opacity:1;z-index:1}.inno-steps–has-backgrounds[data-index=”22″] .inno-steps__background–22{opacity:1;z-index:1}.inno-steps–has-backgrounds[data-index=”23″] .inno-steps__background–23{opacity:1;z-index:1}.inno-steps–has-backgrounds[data-index=”24″] .inno-steps__background–24{opacity:1;z-index:1}.inno-steps–has-backgrounds[data-index=”25″] .inno-steps__background–25{opacity:1;z-index:1}.inno-steps–has-backgrounds[data-index=”26″] .inno-steps__background–26{opacity:1;z-index:1}.inno-steps–has-backgrounds[data-index=”27″] .inno-steps__background–27{opacity:1;z-index:1}.inno-steps–has-backgrounds[data-index=”28″] .inno-steps__background–28{opacity:1;z-index:1}.inno-steps–has-backgrounds[data-index=”29″] .inno-steps__background–29{opacity:1;z-index:1}.inno-steps–has-backgrounds[data-index=”30″] .inno-steps__background–30{opacity:1;z-index:1}.inno-steps .inno-arrow-chart__label-end{opacity:0 !important}.inno-subscribe{display:none;position:relative}.inno-subscribe.is-unsubscribed{display:block}.inno-subscribe.is-preview{display:block}.inno-subscribe.is-dev{display:block}.inno-subscribe.is-dev::before{content:”Non-subscribers only”;display:block;position:absolute;left:-20px;border:1px dashed red;font-size:8px;text-transform:uppercase;padding:5px;font-weight:bold;writing-mode:vertical-lr}.inno-tags{border-top:1px solid var(–color-faint);padding-block:12px}.inno-tags__title{font-family:”Grot 10″,sans-serif;font-size:14px;font-weight:normal}.inno-tags__buttons{display:flex;flex-wrap:wrap;gap:8px}.inno-tags__buttons .inno-button{flex:0 0 auto}.inno-video{width:auto}.inno-video__video{width:100%}.inno-toast{position:fixed;bottom:16px;left:0;right:0;width:max-content;margin:0px auto;z-index:120;display:flex;align-content:center;justify-content:center;text-align:center;font-size:20px;border-radius:5px;background-color:var(–color-text-primary);color:var(–color-background);padding:24px 48px;box-shadow:0 1px 4px rgba(89,87,96,.1),0 3px 6px rgba(89,87,96,.1);translate:0% calc(100% + 18px);transition:translate .4s;opacity:0}.inno-toast b,.inno-toast strong{font-weight:normal}.inno-toast.is-active{translate:0 0;opacity:1}
If you pay for your doctor visits with an Affordable Care Act health plan – Pennie in Pennsylvania., Get Covered NJ in New Jersey, or Healthcare.gov in Delaware – the cost of your premium might be about to go way up. Experts say costs could rise fivefold unless lawmakers move to review or replace tax credits – that ensure no one pays more than 8.5% of their income on premiums – before they expire at the end of the year.
Without these tax credits, people on ACA health plans will need to pay for a greater share of the premium themselves. This was a central issue in the recent standoff between congressional Republicans and Democrats that led to the longest ever U.S. government shutdown.
story continues after advertisement
The shutdown ended after eight senators broke ranks with the Democrats and voted on compromise legislation to reopen the government. Senate Majority Leader John Thune of South Dakota pledged to hold a vote in December on the ACA subsidies. Congress would need to approve extending tax credits.
If they’re not extended, here is how much premiums could increase across the region, according to estimates by KFF, an independent source for health policy research, polling, and journalism:
-
For an average 27-year-old from
AdamsAlleghenyArmstrongBeaverBedfordBerksBlairBradfordBucksButlerCambriaCameronCarbonCentreChesterClarionClearfieldClintonColumbiaCrawfordCumberlandDauphinDelawareElkErieFayetteForestFranklinFultonGreeneHuntingdonIndianaJeffersonJuniataLackawannaLancasterLawrenceLebanonLehighLuzerneLycomingMcKeanMercerMifflinMonroeMontgomeryMontourNorthamptonNorthumberlandPerryPhiladelphiaPikePotterSchuylkillSnyderSomersetSullivanSusquehannaTiogaUnionVenangoWarrenWashingtonWayneWestmorelandWyomingYorkAtlanticBergenBurlingtonCamdenCape MayCumberlandEssexGloucesterHudsonHunterdonMercerMiddlesexMonmouthMorrisOceanPassaicSalemSomersetSussexUnionWarrenKentNew CastleSussex
, making $35,000 a year, insurance premiums could go from costing 27_35k_yesEPTC to 27_35k_noEPTC, an increase of 27_35k_diffEPTC.
-
The expiration of tax credits could mean the end of free insurance for the lowest earners, according to KFF’s estimates. For example, a 27-year-old from
AdamsAlleghenyArmstrongBeaverBedfordBerksBlairBradfordBucksButlerCambriaCameronCarbonCentreChesterClarionClearfieldClintonColumbiaCrawfordCumberlandDauphinDelawareElkErieFayetteForestFranklinFultonGreeneHuntingdonIndianaJeffersonJuniataLackawannaLancasterLawrenceLebanonLehighLuzerneLycomingMcKeanMercerMifflinMonroeMontgomeryMontourNorthamptonNorthumberlandPerryPhiladelphiaPikePotterSchuylkillSnyderSomersetSullivanSusquehannaTiogaUnionVenangoWarrenWashingtonWayneWestmorelandWyomingYorkAtlanticBergenBurlingtonCamdenCape MayCumberlandEssexGloucesterHudsonHunterdonMercerMiddlesexMonmouthMorrisOceanPassaicSalemSomersetSussexUnionWarrenKentNew CastleSussex
making $22,000 a year will have to pay 27_22k_noEPTC if these tax credits expire.
This can be a meaningful amount for someone making less than $2,000 a month. Especially as those in lower income brackets are more likely to forgo health insurance to steer limited financial resources to other household expenses, according to KFF surveys.
-
Enshrined into the original ACA are coverage subsidies for those who earn less than $62,600. As a result, anyone who makes below that threshold would be impacted similarly.
ACA calculates this value at 4 times the poverty rate, which is currently at $15,650.
-
The expiring tax credits were added later to ensure that nobody pays more than 8.5% of their income in premiums. In
AdamsAlleghenyArmstrongBeaverBedfordBerksBlairBradfordBucksButlerCambriaCameronCarbonCentreChesterClarionClearfieldClintonColumbiaCrawfordCumberlandDauphinDelawareElkErieFayetteForestFranklinFultonGreeneHuntingdonIndianaJeffersonJuniataLackawannaLancasterLawrenceLebanonLehighLuzerneLycomingMcKeanMercerMifflinMonroeMontgomeryMontourNorthamptonNorthumberlandPerryPhiladelphiaPikePotterSchuylkillSnyderSomersetSullivanSusquehannaTiogaUnionVenangoWarrenWashingtonWayneWestmorelandWyomingYorkAtlanticBergenBurlingtonCamdenCape MayCumberlandEssexGloucesterHudsonHunterdonMercerMiddlesexMonmouthMorrisOceanPassaicSalemSomersetSussexUnionWarrenKentNew CastleSussex
, a 27-year-old making $65,000 could pay a premium of 27_65k_noEPTC, while a 60-year-old in the same income bracket could pay 60_65k_noEPTC. Older people in higher income brackets, who are generally charged more since they are generally less healthy than younger people, are set to see large premium increases.
-
The impact will be greatest in some rural parts of Pennsylvania. For example, in Fulton County, 60-year-olds making $65,000 could pay an estimated 60_65k_diffEPTC more a month, an almost five times increase from existing premiums.
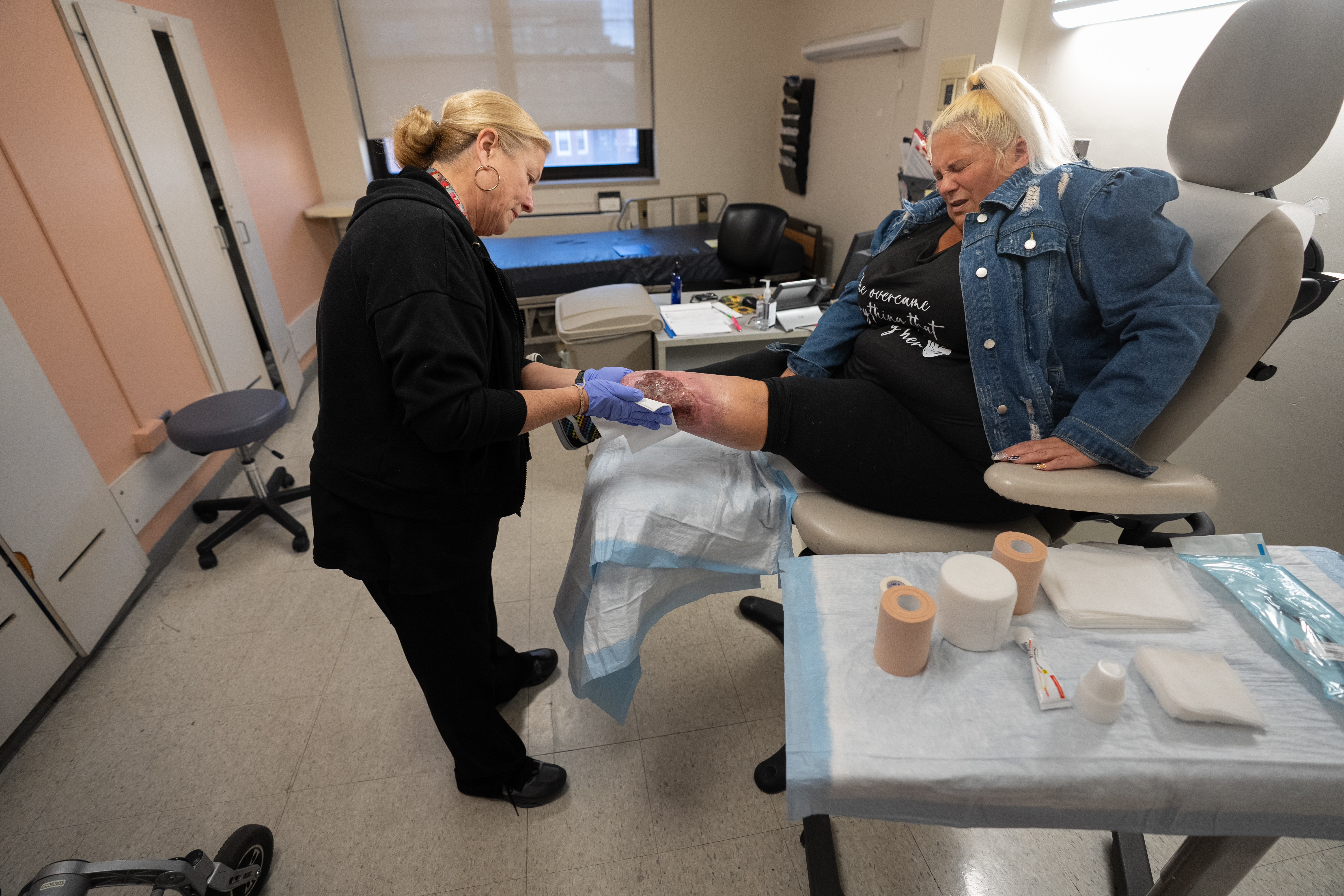
Lisa Davis, director at Pennsylvania Office of Rural Health, explained that generally, “in rural communities, there’s often very little competition” between providers and rural populations “are generally older, poorer, and have more chronic health conditions.”
-
New Jersey could see larger price increases than Philadelphia and the collar counties. In Camden County, for instance, 60-year-olds making $65,000 could pay almost 60_65k_diffEPTC more a month.
Premium estimates are uniform across New Jersey because the state does not have rates that vary by region, as seen in Pennsylvania.
-
See what price increases look like for those across Pennsylvania, New Jersey, and Delaware. Select your county:
AdamsAlleghenyArmstrongBeaverBedfordBerksBlairBradfordBucksButlerCambriaCameronCarbonCentreChesterClarionClearfieldClintonColumbiaCrawfordCumberlandDauphinDelawareElkErieFayetteForestFranklinFultonGreeneHuntingdonIndianaJeffersonJuniataLackawannaLancasterLawrenceLebanonLehighLuzerneLycomingMcKeanMercerMifflinMonroeMontgomeryMontourNorthamptonNorthumberlandPerryPhiladelphiaPikePotterSchuylkillSnyderSomersetSullivanSusquehannaTiogaUnionVenangoWarrenWashingtonWayneWestmorelandWyomingYorkAtlanticBergenBurlingtonCamdenCape MayCumberlandEssexGloucesterHudsonHunterdonMercerMiddlesexMonmouthMorrisOceanPassaicSalemSomersetSussexUnionWarrenKentNew CastleSussex
As a result of these changes, the Congressional Budget Office estimates that 4.2 million Americans will choose to drop their coverage. Pennie administrators estimate about 150,000 of the 500,000 people who bought plans this year will drop out because they find the plans unaffordable.
“Individuals who are least likely to be able to afford these premium increases will not be enrolled. Of course, people want to have health insurance, whether or not they can afford it is a different conversation. It’s a tough, challenging situation,” Davis said.
story continues after advertisement
In addition to tax credits shrinking, premium prices are rising. Rates requested by insurers for 2026 reflected the expectation that only the sickest (and most expensive to cover) individuals will continue to prioritize buying health insurance, Pennsylvania Insurance Commissioner Michael Humphreys said during a call with reporters in September. If this happened, there would be fewer healthier people to share the cost, resulting in higher premiums for those who stay enrolled.
Already, many uninsured people cite the high cost of insurance as the main reason they lack coverage. Sixty-three percent of uninsured adults ages 18-64 said that they were uninsured because the cost of coverage was too high in a 2024 KFF survey.
The impact of this is that those without insurance coverage are more likely to delay or forgo care because of costs, which could lead to worse healthcare outcomes for the individual.
Subscribe to The Philadelphia Inquirer
Our reporting is directly supported by reader subscriptions. If you want more journalism like this story, please subscribe today
Devon Trolley, Executive Director of Pennie expressed, although it is still early in this year’s open enrollment, the uncertainty could already be having an impact. “So far this year, Pennie is seeing 16-18% less new enrollees and a lot more people drop enrollment compared to prior years” said Trolley.
“When people call in, they are making the connection between congressional debate around healthcare subsidies and rising premiums on the consumer side.”
The focus remains on D.C., where lawmakers will determine whether the existing tax credits are extended. President Donald Trump said last week that “some kind of an extension may be necessary” but didn’t go into specifics.
Davis said “Pennie extended the enrollment deadline through to the end of January, but we’re running out of time.”
story continues after advertisement
Methodology
Every year, KFF collects premium information from a variety of sources, such as contacting the state insurance regulator in Pennsylvania. From these data, KFF identifies the benchmark silver plan (typically the second-lowest cost silver plan) by county.
Premiums are calculated based on the age and location of the individuals. KFF then calculates the premium tax credits based on family size and income, using the applicable percentage tables produced by the IRS.
You can use KFF’s calculator tool to find out how much you or your family would pay in premiums with and without the ACA's Enhanced Premium Tax Credits.
- Design, data analysis, and reporting: Jasen Lo
- Development: Jasen Lo and Garland Fordice
- Data: KFF
- Editing: Sam Morris
- Copy Editing: Brian Leighton
(()=>{var X0=(t,e)=>()=>(e||t((e={exports:{}}).exports,e),e.exports);var f5=X0(F=>{var G2={0:”Jan.”,1:”Feb.”,2:”March”,3:”April”,4:”May”,5:”June”,6:”July”,7:”Aug.”,8:”Sept.”,9:”Oct.”,10:”Nov.”,11:”Dec.”};function _5(t){return t===void 0&&(t=new Date),G2[t.getMonth()]}var U2={0:”Jan”,1:”Feb”,2:”Mar”,3:”Apr”,4:”May”,5:”Jun”,6:”Jul”,7:”Aug”,8:”Sep”,9:”Oct”,10:”Nov”,11:”Dec”};function n5(t){return t===void 0&&(t=new Date),U2[t.getMonth()]}function e7(t){return t==null}function i5(t){return typeof t==”number”&&isFinite(t)}function H4(t){return i5(t)&&Math.floor(t)===t}var K2=[“one”,”two”,”three”,”four”,”five”,”six”,”seven”,”eight”,”nine”],Q2=[“million”,”billion”,”trillion”,”quadrillion”,”quintillion”,”sextillion”,”septillion”,”octillion”,”nonillion”,”decillion”],o5=[“th”,”st”,”nd”,”rd”,”th”,”th”,”th”,”th”,”th”,”th”],Z2=[11,12,13];function r5(t){if(e7(t))return””;var e=+t;return H4(e)?Z2.indexOf(e%100)>-1?o5[0]:o5[e%10]:””}var j2=[“first”,”second”,”third”,”fourth”,”fifth”,”sixth”,”seventh”,”eighth”,”ninth”],t3=new RegExp(/s+([^s]*)s*$/);F.apdate=function(t){return t===void 0&&(t=new Date),_5(t)+” “+t.getDate()+”, “+t.getFullYear()},F.apdatetab=function(t){return t===void 0&&(t=new Date),n5(t)+” “+t.getDate()+”, “+t.getFullYear()},F.apmonth=_5,F.apmonthtab=n5,F.apnumber=function(t){if(e7(t))return””;var e=+t;return H4(e)?e=10?t.toString():K2[e-1]:t.toString()},F.aptime=function(t){t===void 0&&(t=new Date);var e,_,n=t.getHours(),o=t.getMinutes(),r=o===0;if(r){if(n===0)return”midnight”;if(n===12)return”noon”}return n0?n:12):(e=”p.m.”,_=n===12?n:n-12),r?_+” “+e:_+”:”+(o<10?"0"+o:o)+" "+e},F.capfirst=function(t){if(e7(t))return"";var e=String(t);return""+e.charAt(0).toUpperCase()+e.slice(1)},F.intcomma=function(t){if(e7(t))return"";var e,_=+t;return i5(_)?((e=_.toString().split("."))[0]=e[0].replace(/B(?=(d{3})+(?!d))/g,","),e.join(".")):t.toString()},F.intword=function(t){if(e7(t))return"";var e=+t;if(!H4(e))return t.toString();var _=Math.abs(e);if(_<1e6)return t.toString();var n=Math.ceil(Math.log(_+1)/Math.LN10)-1,o=n-n%3,r=e/Math.pow(10,o);return(r=Math.round(10*r)/10)+" "+Q2[Math.floor(o/3)-2]},F.ordinal=function(t,e){if(e===void 0&&(e=!1),e7(t))return"";var _=+t;return H4(_)?e&&_{e3.exports={type:”FeatureCollection”,features:[{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-80.1485003817312,40.67377700705386],[-80.15106538492087,40.713146014559456],[-80.15195038744453,40.73341401817142],[-80.15551339286351,40.79224302938789],[-80.15853339818746,40.85510404053717],[-80.18309540648127,40.85466803981863],[-80.2531264277616,40.85396003614894],[-80.26371043126875,40.85403803569461],[-80.33144545183418,40.85291903287482],[-80.42254248025027,40.85227802832385],[-80.51904750960591,40.85134702412079],[-80.51907750202118,40.75359100613331],[-80.51892549985179,40.71843899949148],[-80.51901449152022,40.60836697861208],[-80.51886548693399,40.55930496928591],[-80.51923148549422,40.5334679640156],[-80.51891448434692,40.52141396195939],[-80.5190414809271,40.477370953392786],[-80.46680546513859,40.47734895586173],[-80.43817845604087,40.47779095700122],[-80.39351644250593,40.47729395910577],[-80.36080443222788,40.47759896013245],[-80.27802941104602,40.536743975716554],[-80.25142340476681,40.556030980083385],[-80.22709239880315,40.57416198470331],[-80.21791339570557,40.58188198678515],[-80.21455239452814,40.580826986405754],[-80.20797939387703,40.58808198853686],[-80.20416639226066,40.58857598815154],[-80.19328439018042,40.5969409906512],[-80.18652238724073,40.596133990843974],[-80.18475638756911,40.603592991974736],[-80.18056638682842,40.6073519927766],[-80.17602838492395,40.60812099348085],[-80.1648473814831,40.60696499393572],[-80.16082838107565,40.609498993937876],[-80.15501637851989,40.608020994547516],[-80.15164537828412,40.611152994698564],[-80.14511337650778,40.613454995906714],[-80.1485003817312,40.67377700705386]]]},properties:{geoid:”42007″,name:”Beaver”,state_name:”Pennsylvania”,county_state_name:”Beaver County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.84,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:59.62,”60_65k_diff”:643.96,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:431.46,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:426.45,”40_65k_eptc”:460.42,”60_65k_eptc”:460.41,”27_95k_eptc”:426.45,”40_95k_eptc”:520.04,”60_95k_eptc”:672.91,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.88,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.87,”27_65k_no_eptc”:426.45,”40_65k_no_eptc”:520.04,”60_65k_no_eptc”:1104.37,”27_95k_no_eptc”:426.45,”40_95k_no_eptc”:520.04,”60_95k_no_eptc”:1104.37}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-79.09509910453046,41.34066617808423],[-79.0947321069197,41.375121184450315],[-79.09359111023376,41.42329419374372],[-79.06515710074572,41.423202195026406],[-79.06352310305736,41.45321520026171],[-78.97666107492586,41.45176920372955],[-78.97666007378795,41.43697120093783],[-78.95896006853444,41.437069202253845],[-78.95913107364252,41.50012321380402],[-78.9579720766536,41.54608722210068],[-78.95742107926122,41.579230228574126],[-78.95614108170575,41.62334223674294],[-78.99394509445023,41.62455323594927],[-79.03423310718746,41.62542623361825],[-79.1141661319451,41.626669230462696],[-79.15296414406511,41.626787228674395],[-79.2298861685434,41.62618122564164],[-79.29669418896145,41.625832222478465],[-79.36111620951795,41.62642421955074],[-79.47547324548292,41.625168214210916],[-79.51207325623581,41.62456721291854],[-79.51122324671415,41.50042619015656],[-79.51227924362554,41.46524818329263],[-79.52202724658234,41.465227182805364],[-79.52160224510307,41.44056217791718],[-79.47816623197481,41.440142179939826],[-79.4778252278428,41.386487170539894],[-79.40044220355337,41.38658717331184],[-79.40027220653694,41.436153182452536],[-79.35758919358544,41.43624918503158],[-79.35765619292512,41.43244018425832],[-79.23823015547583,41.43135118860565],[-79.20719914587748,41.4309301904883],[-79.20707514462796,41.41754918747527],[-79.20787514383271,41.39532018307157],[-79.20888113941976,41.331869171319774],[-79.20250913661447,41.32679817057028],[-79.19195513318786,41.32428217120739],[-79.18618313155586,41.32853117196495],[-79.18700813241763,41.337318174004096],[-79.17964113049442,41.33917617418591],[-79.17514312866017,41.335977173828425],[-79.17557512780411,41.32696717200439],[-79.1703621261033,41.326748171949916],[-79.16664912616604,41.332139173662604],[-79.16917012739228,41.339657174423216],[-79.16809012652219,41.343102175602375],[-79.16272712528983,41.34322217560438],[-79.1599311243672,41.33995317552967],[-79.16243912410732,41.331836173434],[-79.15473612185849,41.32865817378142],[-79.14823612003578,41.33166517438042],[-79.13979411837829,41.34143917678051],[-79.1321891159564,41.3389671764145],[-79.12390111267158,41.33096417464439],[-79.11190110807432,41.32502417412582],[-79.10588810602283,41.32671117515465],[-79.10448710566186,41.331317176083154],[-79.1072341079237,41.336415176544975],[-79.104980106717,41.34153417818739],[-79.09966210520813,41.3425951783638],[-79.09509910453046,41.34066617808423]]]},properties:{geoid:”42053″,name:”Forest”,state_name:”Pennsylvania”,county_state_name:”Forest County, Pennsylvania”,”27_22k_diff”:66.19,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.84,”40_35k_diff”:131.84,”60_35k_diff”:131.84,”27_65k_diff”:72.39,”40_65k_diff”:189.32,”60_65k_diff”:919.39,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:706.89,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.42,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:532.81,”40_95k_eptc”:649.74,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.19,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.88,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:532.81,”40_65k_no_eptc”:649.74,”60_65k_no_eptc”:1379.81,”27_95k_no_eptc”:532.81,”40_95k_no_eptc”:649.74,”60_95k_no_eptc”:1379.81}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-77.59928064783205,41.54227927870558],[-77.54727263168708,41.54288228076386],[-77.50549661820207,41.543129283307785],[-77.40009858463696,41.54403928702144],[-77.33787156505268,41.54408929029585],[-77.2985075526741,41.544398291666866],[-77.28499154889735,41.5441262921611],[-77.11718549517981,41.5471422995759],[-77.02264746595856,41.54961430372033],[-76.96048144606146,41.55137930631721],[-76.96325144765193,41.55478030745259],[-76.95239344456407,41.56505830955726],[-76.94307944181269,41.56933131042403],[-76.9329644381753,41.56900031065257],[-76.92657243629604,41.571099311548416],[-76.92217343659406,41.58104531391339],[-76.91743743464743,41.58271131449052],[-76.90843443116232,41.58147131446468],[-76.88288842362711,41.58838331691312],[-76.87833342247934,41.59055431734416],[-76.87471642231779,41.59692731835535],[-76.87870142514262,41.62035232263616],[-76.88126642812813,41.648418327905645],[-76.88435843069173,41.673130332653024],[-76.8986094440092,41.79447335521799],[-76.89931744461023,41.809336357297624],[-76.90211844687775,41.82492236054189],[-76.90774345129306,41.86380236759786],[-76.90891245253471,41.875252369977446],[-76.91680845944805,41.9342563800028],[-76.921691464285,41.967520386692996],[-76.92706146812547,42.001583392652776],[-76.9657934800738,42.00112239085535],[-77.1032545244112,41.999841385179074],[-77.16142154210746,41.999613382737266],[-77.17911854766089,41.99976938193274],[-77.23941056689313,41.999609379636475],[-77.30533058805483,41.99972337647955],[-77.39582861692263,42.00007937271468],[-77.51196365378915,42.00008536783416],[-77.56285867054972,41.999614365715594],[-77.61002968473923,41.99937636391792],[-77.60916168244414,41.96125735717078],[-77.6079186790435,41.9242993498308],[-77.60671167456668,41.87507734067145],[-77.6045216650633,41.759960319762264],[-77.60386466396925,41.74458131659821],[-77.60093765393819,41.61604529293923],[-77.59928064783205,41.54227927870558]]]},properties:{geoid:”42117″,name:”Tioga”,state_name:”Pennsylvania”,county_state_name:”Tioga County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.83,”40_35k_diff”:131.83,”60_35k_diff”:131.83,”27_65k_diff”:52.73,”40_65k_diff”:165.35,”60_65k_diff”:868.49,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:655.99,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.42,”40_65k_eptc”:460.42,”60_65k_eptc”:460.41,”27_95k_eptc”:513.15,”40_95k_eptc”:625.77,”60_95k_eptc”:672.91,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.87,”27_65k_no_eptc”:513.15,”40_65k_no_eptc”:625.77,”60_65k_no_eptc”:1328.9,”27_95k_no_eptc”:513.15,”40_95k_no_eptc”:625.77,”60_95k_no_eptc”:1328.9}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-76.56634122940726,40.196652061278385],[-76.56953422974124,40.19608106139943],[-76.59133824030455,40.25209507125608],[-76.61264925076011,40.30818808192341],[-76.62625725716038,40.341166087824114],[-76.63627126258514,40.36644709160926],[-76.66565527653916,40.44217110521599],[-76.67804228244565,40.47472511183401],[-76.62468926767616,40.504689119566926],[-76.58926025762597,40.52488512429168],[-76.53541624302886,40.555165132401825],[-76.58448226107602,40.58511813672627],[-76.64143528138806,40.6209301411894],[-76.66882529015679,40.63760714298005],[-76.70162630200974,40.65809014635093],[-76.70392630245547,40.65537814551448],[-76.71316930592054,40.65955914576016],[-76.71827530775207,40.65839714531215],[-76.72173130826788,40.653491144517204],[-76.73276231210131,40.65474114461708],[-76.74589631637652,40.654472143704844],[-76.75623431864581,40.64809614178823],[-76.7782833260665,40.645994140779706],[-76.78585532847747,40.641740139575354],[-76.7938533302861,40.640522139411416],[-76.80249433312115,40.64728814008554],[-76.80990433538666,40.64192413867473],[-76.8101513356167,40.634854137257335],[-76.81320433560245,40.63331713675045],[-76.82740734036804,40.63395413606591],[-76.83316434163825,40.627610134842165],[-76.84010634422437,40.625447134496255],[-76.85460134820646,40.62572813376081],[-76.86425635213506,40.627593133988],[-76.86948535293409,40.62348913279815],[-76.86953035323971,40.61839113217414],[-76.87271935385373,40.61632113132385],[-76.88682435827764,40.617716131061336],[-76.89025635877779,40.61628713071878],[-76.89004135828907,40.61033912938864],[-76.89887136138961,40.61046012901371],[-76.90334436270884,40.61190012925881],[-76.92549837017538,40.608899127984145],[-76.93696437326714,40.612849128282434],[-76.9491503790798,40.62817513019318],[-76.95083837954778,40.62705213019682],[-76.95355337937883,40.61477812813541],[-76.95310737857493,40.60451212606339],[-76.95875737940123,40.59286312300894],[-76.96527038138056,40.58706812188669],[-76.98367538565506,40.57826711969231],[-76.98816338713436,40.5745931190414],[-76.99239838828788,40.56788511761984],[-76.99186438787949,40.56128011619062],[-76.98199138343647,40.54342311308903],[-76.98054838188659,40.53834011177554],[-76.98153238272425,40.531931110479235],[-76.98566538275155,40.52500510916726],[-76.98510638193332,40.51635710786342],[-76.9783533798435,40.50715710621244],[-76.96909237641292,40.49757010482572],[-76.95308537037515,40.490629103392244],[-76.94946836908707,40.48453510286069],[-76.9493993682219,40.46904509972373],[-76.95281136906067,40.462475098438276],[-76.9611453701622,40.45579809704878],[-76.96949837337904,40.45274009619361],[-76.9804543762205,40.44714409423317],[-76.98943237801534,40.438171092561404],[-76.99791738045631,40.43367809120451],[-77.00323738162888,40.42680808905617],[-77.0162723859632,40.42518108866887],[-77.0158493858497,40.41565808643745],[-77.01173638335233,40.407420085635806],[-77.01312738396928,40.40235708390083],[-77.02147138627397,40.39792808275546],[-77.02864738797967,40.3912050816005],[-77.02914638733353,40.38662108097122],[-77.02684338677759,40.38054807963006],[-77.02306938452588,40.37640707888868],[-77.02165238384814,40.36837607732739],[-77.01918038347867,40.36479307638985],[-77.00819337868134,40.35845707633103],[-76.99802437599497,40.35668707628473],[-76.98199837040093,40.357328076707354],[-76.97062736684151,40.35631307693482],[-76.96115236402991,40.35804107795481],[-76.93754935719393,40.3574890781702],[-76.93267435452191,40.35532607808746],[-76.92852335361007,40.34799307714929],[-76.9261823519384,40.34098807583628],[-76.91727234909479,40.332723074200416],[-76.9149723475798,40.32849207415658],[-76.91213134626389,40.32550307374626],[-76.91348734603557,40.31755607206771],[-76.9229773480045,40.30096406808397],[-76.92447834868742,40.29130206643648],[-76.92016134634287,40.28301806480924],[-76.91604234471195,40.279904064078245],[-76.91375434393403,40.271137062633336],[-76.90465233957491,40.26072506133496],[-76.89777333730781,40.254673059636225],[-76.88973633412527,40.24932105920165],[-76.87870933055864,40.2438970590094],[-76.86647532574476,40.231165056284354],[-76.85902532342105,40.2263360555814],[-76.8394703169858,40.221623056105244],[-76.83478731503212,40.21797005525046],[-76.82886131270374,40.20502805270404],[-76.82164031014557,40.20135105244922],[-76.80058730276451,40.200119053175456],[-76.7876702986242,40.191558051771054],[-76.77401629427925,40.184099051328225],[-76.76303628985261,40.17896305080871],[-76.75319728649042,40.176051050167295],[-76.74911428493915,40.167121048716055],[-76.74826128375427,40.1557690461917],[-76.74579228264591,40.145801044192794],[-76.74557028204892,40.13930604311691],[-76.7435392813275,40.13085804214603],[-76.73265427715316,40.122740040219476],[-76.72162227347948,40.120078040625785],[-76.71590927245836,40.13148704323797],[-76.71120027113828,40.133280043373304],[-76.70569826998616,40.14302004568767],[-76.69987626760226,40.145118046631055],[-76.69616026767065,40.150125047669796],[-76.69559626726935,40.154105047891804],[-76.68315326319943,40.15180304802415],[-76.67056525897385,40.15449504946997],[-76.67274426060267,40.1576160496791],[-76.66204525737413,40.16347505115567],[-76.65506725572591,40.16396705151812],[-76.65310625494529,40.16605805218553],[-76.64410525200736,40.16491405198994],[-76.63474624962872,40.170548053611654],[-76.63210424854324,40.17062405362638],[-76.62768724701395,40.17674705525871],[-76.62320824627285,40.179320055983425],[-76.61595024419172,40.180615056823626],[-76.6129892432841,40.18538905773438],[-76.60652124210938,40.18999805818924],[-76.59986723948677,40.188272058879946],[-76.58268423467301,40.19096005939916],[-76.5790532337508,40.19486406077949],[-76.57026223010514,40.19456706045131],[-76.56634122940726,40.196652061278385]]]},properties:{geoid:”42043″,name:”Dauphin”,state_name:”Pennsylvania”,county_state_name:”Dauphin County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.83,”60_35k_diff”:131.83,”27_65k_diff”:230.11,”40_65k_diff”:381.65,”60_65k_diff”:1327.83,”27_95k_diff”:17.61,”40_95k_diff”:169.15,”60_95k_diff”:1115.33,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.05,”27_65k_eptc”:460.41,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:672.91,”40_95k_eptc”:672.92,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:690.52,”40_65k_no_eptc”:842.07,”60_65k_no_eptc”:1788.25,”27_95k_no_eptc”:690.52,”40_95k_no_eptc”:842.07,”60_95k_no_eptc”:1788.25}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-74.69558171005325,41.35761535692806],[-74.70009871112774,41.35466335634183],[-74.70953271371309,41.352334354850704],[-74.71762371637949,41.3485733545044],[-74.7259527186385,41.34620035329603],[-74.75239972740916,41.346544352966916],[-74.75609372899716,41.34519835183622],[-74.76082273002328,41.339518350580576],[-74.76348673035191,41.33127934954884],[-74.77265873298373,41.32478934752068],[-74.78414073599781,41.32429334749309],[-74.79158573844181,41.323027346438224],[-74.79607073924886,41.319611345515725],[-74.79192373733228,41.31121834462583],[-74.80742974168739,41.302820342107054],[-74.81203474285957,41.29816634146788],[-74.82121274587499,41.29432133996029],[-74.83034874839414,41.28707333828771],[-74.83778875063497,41.27801733633676],[-74.84044175035011,41.27199233524771],[-74.84645675217196,41.262421332706886],[-74.84488475084702,41.25813833182708],[-74.8496187521527,41.25112233099044],[-74.85567075425728,41.250139330376655],[-74.86111875586262,41.24365332884987],[-74.86233575573938,41.23743932719478],[-74.86617475658244,41.23270132606037],[-74.86743875674972,41.2274283258417],[-74.86083875353667,41.22232632455106],[-74.85947475363075,41.21878132404941],[-74.86897975615628,41.206126321377006],[-74.8747947573105,41.19724731942597],[-74.8790267579908,41.186519316692575],[-74.88233275887643,41.18082931623074],[-74.8899897602379,41.173225313786084],[-74.90073976268518,41.16519731211815],[-74.9052577644432,41.15567631031102],[-74.9244707688835,41.13753830618384],[-74.93114777098627,41.13374230526721],[-74.94449977513176,41.12998230386473],[-74.94811377532336,41.123200302086744],[-74.96323477948313,41.114684300332435],[-74.97359178267516,41.11319429921634],[-74.97998678481467,41.11051529880122],[-74.99171978728133,41.09229229512348],[-74.98826478643308,41.08823029448086],[-74.98131578450409,41.08986829509079],[-74.97689078305659,41.093188295318555],[-74.96943578034174,41.09608229599501],[-74.96690777928738,41.09441829601194],[-74.93889376892372,41.068777292481236],[-74.90188975554999,41.03409828703728],[-74.85933573857217,40.994742280488786],[-74.82309172526212,40.960527275527625],[-74.81540772277236,40.95367527483489],[-74.7694267048059,40.91094226777644],[-74.76606070404603,40.91274226852151],[-74.75553570124255,40.91365726918971],[-74.74758469825223,40.919989270458096],[-74.7375426956782,40.91892527031376],[-74.73192969365786,40.920860271184715],[-74.72871869215855,40.916485269963275],[-74.71816868912747,40.91229926979687],[-74.71261668668765,40.90742226935539],[-74.71425868683734,40.90128826810535],[-74.71151868569376,40.89917626765361],[-74.7034806838432,40.90171326809056],[-74.69687668197041,40.90743127009911],[-74.68953367942677,40.90733026982029],[-74.6861056781489,40.91000427060703],[-74.67949867614766,40.909164270804055],[-74.6699346739208,40.91394727163545],[-74.66531167234787,40.917482272936326],[-74.65832167038756,40.91809227313653],[-74.65161066794822,40.92305727421596],[-74.65403766870081,40.926650274864485],[-74.65034566776936,40.93139027650897],[-74.64158266526279,40.93365527648278],[-74.63689866459042,40.94174927832542],[-74.63487966387805,40.949666279944964],[-74.63641366548478,40.954028280706005],[-74.64135466706112,40.9593962814614],[-74.64156166753405,40.96220728245534],[-74.63327266561781,40.97103128426349],[-74.63237966534106,40.97372528474556],[-74.60634565878523,40.99837929076163],[-74.54711064262524,41.04859630285594],[-74.52194163643034,41.070742307475875],[-74.50321363138539,41.08588131128435],[-74.48313662537768,41.10439631577114],[-74.47676162340859,41.109666316639036],[-74.42126160956751,41.160542328430175],[-74.39001060035551,41.18580333516015],[-74.36751159449284,41.20324933920463],[-74.3955936050459,41.217950340796335],[-74.42875361607328,41.23442334274419],[-74.45786362636616,41.24843534446867],[-74.49126463842,41.263477346438336],[-74.5075156436161,41.27153734678985],[-74.53983765489872,41.2867413488731],[-74.64158369101027,41.332949354225875],[-74.69558171005325,41.35761535692806]]]},properties:{geoid:”34037″,name:”Sussex”,state_name:”New Jersey”,county_state_name:”Sussex County, New Jersey”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:84.32,”60_65k_diff”:696.41,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:483.91,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.05,”27_65k_eptc”:446.7,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:446.7,”40_95k_eptc”:544.74,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:446.7,”40_65k_no_eptc”:544.74,”60_65k_no_eptc”:1156.83,”27_95k_no_eptc”:446.7,”40_95k_no_eptc”:544.74,”60_95k_no_eptc”:1156.83}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-75.35918591495425,41.239214309331466],[-75.35049791215027,41.244397310735735],[-75.34491391042774,41.249302311983],[-75.34136590934745,41.254458312735125],[-75.34439791154658,41.257849313778244],[-75.35013691336232,41.25954431355456],[-75.34724691200435,41.26603831490596],[-75.33460490883935,41.26972831604154],[-75.33172590825484,41.27519831759509],[-75.33364590909751,41.279455318326725],[-75.32975790853102,41.28558431967719],[-75.3246089069467,41.288885319944505],[-75.3278139085912,41.295330321095506],[-75.32761090870744,41.29901632209708],[-75.32228290670975,41.299890322404345],[-75.31500090484333,41.30906532477796],[-75.31356490434682,41.31270532509839],[-75.31626890597275,41.315985325361446],[-75.31205190537841,41.32113132652273],[-75.31114490550351,41.33144732884627],[-75.31755390746828,41.33467332939602],[-75.32245190907493,41.34004833053448],[-75.32595791051399,41.34068333025532],[-75.32938191117374,41.335550329072184],[-75.34297891596945,41.33609732827783],[-75.34435791684828,41.341036329279795],[-75.336752913986,41.345502330703894],[-75.34204191674901,41.35527533211749],[-75.3464159179517,41.35728933226503],[-75.35064992083129,41.367702334362725],[-75.3377599170202,41.376260336793706],[-75.33067191416852,41.36960133506279],[-75.32365891175681,41.366053335519226],[-75.31429390822377,41.36861433587826],[-75.30906890765222,41.37468733724181],[-75.30606190669961,41.37423133754844],[-75.29814990320396,41.367293336562504],[-75.27829489750037,41.372489338033134],[-75.26571389291506,41.37239033887329],[-75.26263489325046,41.37509733883289],[-75.2619058923322,41.381962340597426],[-75.25507489056659,41.38699434200121],[-75.25308489032504,41.3913023421206],[-75.25671089216056,41.394073343145],[-75.25490689221785,41.39913534393123],[-75.24681088975325,41.402443345111315],[-75.24843489037085,41.40849134621179],[-75.25179789136065,41.41046934669578],[-75.25008689117914,41.41822734792362],[-75.24234788930696,41.42131934837994],[-75.2295188858653,41.42497935021844],[-75.21831688150212,41.424125349878594],[-75.20686187857176,41.43095335168361],[-75.19962987622601,41.43365135301268],[-75.19942187671418,41.43753635313231],[-75.19138187407255,41.438902354179504],[-75.18623787259548,41.44284435528641],[-75.18928587339401,41.44726735570923],[-75.18691887304408,41.45359135700118],[-75.18763687380384,41.45825235755934],[-75.1783558709969,41.461961358585214],[-75.17792387110015,41.46538735934803],[-75.16894486874119,41.47510936197387],[-75.12461785914262,41.53185937456616],[-75.10982885547489,41.551052378317756],[-75.09746685222011,41.566215381483175],[-75.06956084631189,41.601882389725894],[-75.07447684844527,41.60813339047357],[-75.06823184637229,41.610228391256726],[-75.05972984292126,41.61042339192467],[-75.06153884428603,41.61528239209462],[-75.05973284367803,41.61756439319045],[-75.05302184185912,41.618523393587246],[-75.04838283947545,41.61593039344417],[-75.04427583891052,41.61765239346647],[-75.0436368390976,41.62283639453979],[-75.04848984138968,41.63250239596716],[-75.0494988420361,41.64157039768085],[-75.0477278415315,41.64567039914561],[-75.04923584294204,41.650542399496594],[-75.04888184335353,41.65781640130521],[-75.05020884417958,41.66254240180634],[-75.05942684764932,41.67354540376082],[-75.05125384515004,41.68002640508809],[-75.05262884646281,41.688118406316946],[-75.05993784898257,41.699986408582056],[-75.06669185127693,41.704819409301244],[-75.06891885278579,41.70980241007586],[-75.0633958514946,41.713066411387395],[-75.05311184783159,41.71152941092263],[-75.04984984713329,41.71307441194511],[-75.05355884894824,41.72687641432924],[-75.0547228495632,41.73649541592891],[-75.052680849762,41.744834417081826],[-75.0531988503082,41.75243341901994],[-75.0596348535671,41.76300242087909],[-75.06475985541861,41.76669542093187],[-75.07246585778805,41.76855642159535],[-75.07577185961003,41.77167542207414],[-75.09281186439807,41.76836942032864],[-75.10019886669936,41.769022420283896],[-75.10471286861589,41.77439242131699],[-75.10221586868506,41.78644242326977],[-75.09263986572581,41.79666842577706],[-75.07907186229112,41.79704842629797],[-75.07565386155551,41.79956342681762],[-75.07251686101118,41.80600742868084],[-75.07224986052408,41.81413942953351],[-75.07936386319699,41.8151084294835],[-75.0855268647449,41.811720429152295],[-75.08988186668383,41.811709428374314],[-75.10056687060316,41.81893542930781],[-75.11267887420365,41.82240343007306],[-75.11501787597305,41.8270664310371],[-75.11314687527985,41.83617343249965],[-75.1133338759794,41.841675433887396],[-75.116596877277,41.845457434103814],[-75.13047988121589,41.84517243326073],[-75.13987788534381,41.852066434120765],[-75.15150588900545,41.849079433831605],[-75.1576568905553,41.848700433069915],[-75.16396689344134,41.851298433451284],[-75.16805689426641,41.85797643421197],[-75.16795189486123,41.867525436464966],[-75.17056689663436,41.871616437295664],[-75.17631989838854,41.87243143686512],[-75.18218790008011,41.8623864345029],[-75.18678590101808,41.86031143415059],[-75.19490590337638,41.86758843526707],[-75.20646890729866,41.869907435653644],[-75.21478290985159,41.86749143420262],[-75.22316791185838,41.85792443293247],[-75.23114491557399,41.85924843269461],[-75.24114891910061,41.867260433241704],[-75.2487949211386,41.86274743247543],[-75.25758592382796,41.86196543230113],[-75.26159192483226,41.86494843257316],[-75.26407392689072,41.87076243327179],[-75.25746192422528,41.8768504346033],[-75.26062492589695,41.883791436348815],[-75.27136192955626,41.88752143656613],[-75.2730369305342,41.89632143753654],[-75.26729792928583,41.9030384390252],[-75.2677359306781,41.90787644036772],[-75.27672293456344,41.922523442528096],[-75.27725193546429,41.933722444798185],[-75.27871093601965,41.9385314460514],[-75.28852693932971,41.94246644607496],[-75.29158194083313,41.946478446503065],[-75.29256594140593,41.953874447606495],[-75.30047694428158,41.95384644783668],[-75.30258694417252,41.94802044647996],[-75.31094294717455,41.949111446076415],[-75.31753494940958,41.95358644716056],[-75.3195389508016,41.96011444822797],[-75.32909095344318,41.96858544932056],[-75.34159295828924,41.97222444935336],[-75.34187995865356,41.97535945011218],[-75.33754795823907,41.984273451756216],[-75.34108095987492,41.99286445331375],[-75.35964696545872,41.999562454353175],[-75.48314200543223,41.999259448848285],[-75.48067500191777,41.958359441619926],[-75.47674399496942,41.87755442655227],[-75.4744679924526,41.8519634216627],[-75.47014298538085,41.772114407152905],[-75.46705198121998,41.72239639739235],[-75.46241297497549,41.641595382526575],[-75.45932896964635,41.58769137262985],[-75.45729296590626,41.546363364721415],[-75.45501296363192,41.51683635901951],[-75.45226895971464,41.47602735125495],[-75.45121295821163,41.44699934531825],[-75.44881295369622,41.40353233786683],[-75.44700295115975,41.36317733008492],[-75.44333894541562,41.29930331808209],[-75.44142294249704,41.260061310692016],[-75.44523594350929,41.25454130900015],[-75.4566869461302,41.25394630835841],[-75.4610869480694,41.24727630752537],[-75.46749994936674,41.24798730737139],[-75.47213195065932,41.24348330607199],[-75.4771239531072,41.24643030631951],[-75.48447895446124,41.24598230560803],[-75.48506095481743,41.242656304904436],[-75.49605895846172,41.24295630494504],[-75.50103695923991,41.236355303814854],[-75.50560896099414,41.23254730249383],[-75.45905994632388,41.23421230483277],[-75.37462891996248,41.23779130831702],[-75.35918591495425,41.239214309331466]]]},properties:{geoid:”42127″,name:”Wayne”,state_name:”Pennsylvania”,county_state_name:”Wayne County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.83,”60_35k_diff”:131.84,”27_65k_diff”:110.27,”40_65k_diff”:235.51,”60_65k_diff”:1017.48,”27_95k_diff”:0,”40_95k_diff”:23.01,”60_95k_diff”:804.98,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.41,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:570.68,”40_95k_eptc”:672.92,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:570.68,”40_65k_no_eptc”:695.93,”60_65k_no_eptc”:1477.9,”27_95k_no_eptc”:570.68,”40_95k_no_eptc”:695.93,”60_95k_no_eptc”:1477.9}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-79.99801728452181,39.98332988111519],[-80.00693028767851,39.98470688154405],[-80.01100728849738,39.983205880675925],[-80.01802029071354,39.9774968791331],[-80.02825829368155,39.98303388033254],[-80.03371129487277,39.98333587996504],[-80.03194029427982,39.977698878915966],[-80.03978129696563,39.9741078783723],[-80.04893729987988,39.97926887856549],[-80.04785929979363,39.984760879668215],[-80.05028630096884,39.990149880418166],[-80.04386029896979,39.994532881846055],[-80.04717130168571,40.00513088334372],[-80.05480430396408,40.00429788311617],[-80.060317305745,40.00946088348026],[-80.06799530702447,40.00292188220571],[-80.08611731236522,39.99032087902004],[-80.09211731408313,39.992016879316814],[-80.10573531804295,39.99096387814929],[-80.11128831950494,39.98817487728055],[-80.11831132201404,39.99129687819874],[-80.12951332551486,39.98841387705936],[-80.13641232772036,39.99259487720348],[-80.150986332874,39.99442087727096],[-80.1552743343635,39.996549877665785],[-80.16045933634993,40.003346878474396],[-80.17592434117547,40.008145878426696],[-80.18126634249231,40.006599878445016],[-80.18241734255642,40.00323887730971],[-80.19123634501113,40.001938876587985],[-80.19389334603328,40.00492087730274],[-80.19944334738283,40.00320387659746],[-80.20821235090008,40.005119876572905],[-80.21479535247855,40.00281187586705],[-80.2228133553759,40.00466987576961],[-80.22564335613,40.00753387673097],[-80.24014136064835,40.00948387649625],[-80.24430336168379,40.00705287596891],[-80.25175836385559,40.00779087554824],[-80.25293936511132,40.0051918746875],[-80.26659536852152,40.00169787344317],[-80.27503637144297,40.003560873806194],[-80.27196937081699,40.0077368749699],[-80.2732583713609,40.01328787579633],[-80.28484837514674,40.01263687496705],[-80.28742437656835,40.01921387627995],[-80.29441337784236,40.018554876127595],[-80.30139938040212,40.02056687587533],[-80.31021638308131,40.01766187510216],[-80.30911738226519,40.00585787239372],[-80.31257138230916,40.00330087206078],[-80.3210583858453,40.00562787192443],[-80.32835938737733,40.004711871930745],[-80.3517693951141,40.00015486943617],[-80.35432739509248,39.99730186865283],[-80.36907639983373,39.997196868450835],[-80.37950840271554,39.994132867579296],[-80.39060640536687,39.98837186612512],[-80.39578140730796,39.98352486497414],[-80.39647840697343,39.97789786383014],[-80.40169040871668,39.97868286300317],[-80.40671641034915,39.976763863199196],[-80.41292441194179,39.97696286254143],[-80.41995541345787,39.975423862018474],[-80.42538241462485,39.971887860791945],[-80.42976341730585,39.97584486151484],[-80.43479041850303,39.977512862061914],[-80.44300342110134,39.97607586083898],[-80.44697842158203,39.97115985988548],[-80.45391142381371,39.97310885990505],[-80.45638442416471,39.969404859378486],[-80.46129742643994,39.96738885836987],[-80.45870042472254,39.96408885772531],[-80.46360342618611,39.96091285760635],[-80.46611842716138,39.956810856495174],[-80.47528042933043,39.9520728554003],[-80.49074043425456,39.95532085475689],[-80.48662343313202,39.9602298564564],[-80.49977043689351,39.95760585540199],[-80.5021524373651,39.95416885421142],[-80.50988544032583,39.95930685475578],[-80.51909444277933,39.962207855205236],[-80.5193424408249,39.934708850366746],[-80.51889443772289,39.89097184122427],[-80.51901643517601,39.84472983294898],[-80.51942643248877,39.8061888250944],[-80.51934542548624,39.721410808408415],[-80.4954844186743,39.72122380992763],[-80.41010139277633,39.72117781360401],[-80.3722793809098,39.72143581542884],[-80.2495173432308,39.72100982011046],[-80.22392233486579,39.72121782110149],[-80.14917031172861,39.72122982450903],[-80.12690930492971,39.72106482582098],[-80.07595028965405,39.72135782742329],[-80.00001126667885,39.721171830769045],[-79.94067424770053,39.72067883360615],[-79.91628324083872,39.720784834208565],[-79.9061772380032,39.7334018374001],[-79.90350923820215,39.73926683834142],[-79.90368223795308,39.74348583886292],[-79.90718223949258,39.74748584013832],[-79.91438224249089,39.75218484016307],[-79.92248324475104,39.753484840665756],[-79.9300832469168,39.75708584045004],[-79.93468324884887,39.764684842405245],[-79.93298224935882,39.771484842919136],[-79.93441425058286,39.781284844773474],[-79.92929424866358,39.78628584631799],[-79.9139812448323,39.78798484767768],[-79.90858024354105,39.793484848396915],[-79.91018024418143,39.79958484976826],[-79.92017124862501,39.81228585206009],[-79.92118024917646,39.815684852776435],[-79.92171925000478,39.831331855175804],[-79.92437925155336,39.8381838565219],[-79.9364802558998,39.841683856640365],[-79.93798025613295,39.84668385740793],[-79.92465325296637,39.85506385971221],[-79.92478025320611,39.858790860774064],[-79.93067925530599,39.868083862310826],[-79.92767825520511,39.87198386295578],[-79.91685025133094,39.87661186416449],[-79.91528125147357,39.88030786546687],[-79.92843325728248,39.90229086890017],[-79.92960125812098,39.90774686984449],[-79.92332825688246,39.91774687194799],[-79.92560025757369,39.92480287318289],[-79.9350562610185,39.93360287450329],[-79.94272026470819,39.94297887635991],[-79.94766426687883,39.94734687672413],[-79.95724926979697,39.95328187706338],[-79.96513727253998,39.95515387777972],[-79.97424127482776,39.955121876981956],[-79.99371428084116,39.949393874827464],[-79.99881928250949,39.95089787532447],[-80.00934728604254,39.958801876511714],[-80.01073828808586,39.9711538788762],[-80.00913828783145,39.97715387951456],[-80.00585828673277,39.98020988016414],[-79.99801728452181,39.98332988111519]]]},properties:{geoid:”42059″,name:”Greene”,state_name:”Pennsylvania”,county_state_name:”Greene County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.83,”40_35k_diff”:131.83,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:31.55,”60_65k_diff”:584.35,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:371.85,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:403.43,”40_65k_eptc”:460.42,”60_65k_eptc”:460.41,”27_95k_eptc”:403.43,”40_95k_eptc”:491.97,”60_95k_eptc”:672.91,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.87,”27_65k_no_eptc”:403.43,”40_65k_no_eptc”:491.97,”60_65k_no_eptc”:1044.76,”27_95k_no_eptc”:403.43,”40_95k_no_eptc”:491.97,”60_95k_no_eptc”:1044.76}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-79.20888113941976,41.331869171319774],[-79.20917013610776,41.2925651638198],[-79.20977813315318,41.24995515577148],[-79.21020112753713,41.17367114227784],[-79.2111841225111,41.112345129921415],[-79.2113231206853,41.07874512377721],[-79.2144971222464,41.07878312423414],[-79.21521711998865,41.05052311844085],[-79.21020011784044,41.04909911852806],[-79.21264111262849,40.966491102275135],[-79.21254811215468,40.96053510192483],[-79.21570911137539,40.94005809799634],[-79.21531310952638,40.911354092495806],[-79.12472708101028,40.910579095423174],[-79.0699320642312,40.90980109819462],[-78.99975804231453,40.90914610122693],[-78.94642402552712,40.90844710258313],[-78.86747400050072,40.90622710554256],[-78.80516998044637,40.905988108225486],[-78.80404998435297,40.95182211683906],[-78.8040439892539,41.01819912942067],[-78.8045549941375,41.09077014365945],[-78.80453499787805,41.132194151314394],[-78.781192993038,41.174794160524534],[-78.76637999048735,41.20276716623405],[-78.71025097311792,41.201867168791466],[-78.71006197495215,41.23025117385549],[-78.73821698371718,41.23068017279338],[-78.73910398541629,41.25377617671173],[-78.73528298574165,41.2629231787482],[-78.74977699095443,41.269528179796445],[-78.81196701213878,41.29687218244804],[-78.874757033943,41.32496918458002],[-78.95916006279981,41.362169188277235],[-78.95944906340542,41.37115218953436],[-78.96654706584556,41.37094018958921],[-78.96981006741947,41.37590419007209],[-78.97448106865815,41.37548418992503],[-78.98155107051939,41.36776118799514],[-78.99269107355127,41.368624187575065],[-79.0038200763276,41.3590251856226],[-79.01405608003626,41.357642184388276],[-79.01635707986401,41.35100718353058],[-79.02033208179826,41.35050218302616],[-79.02778908458339,41.35721318396196],[-79.03996408821595,41.35668418386103],[-79.05221809183755,41.35113018209302],[-79.06624209615103,41.35038918116007],[-79.07670909898594,41.35425718169105],[-79.08112910110286,41.35269918056809],[-79.09160910311122,41.34096117872043],[-79.09509910453046,41.34066617808423],[-79.09966210520813,41.3425951783638],[-79.104980106717,41.34153417818739],[-79.1072341079237,41.336415176544975],[-79.10448710566186,41.331317176083154],[-79.10588810602283,41.32671117515465],[-79.11190110807432,41.32502417412582],[-79.12390111267158,41.33096417464439],[-79.1321891159564,41.3389671764145],[-79.13979411837829,41.34143917678051],[-79.14823612003578,41.33166517438042],[-79.15473612185849,41.32865817378142],[-79.16243912410732,41.331836173434],[-79.1599311243672,41.33995317552967],[-79.16272712528983,41.34322217560438],[-79.16809012652219,41.343102175602375],[-79.16917012739228,41.339657174423216],[-79.16664912616604,41.332139173662604],[-79.1703621261033,41.326748171949916],[-79.17557512780411,41.32696717200439],[-79.17514312866017,41.335977173828425],[-79.17964113049442,41.33917617418591],[-79.18700813241763,41.337318174004096],[-79.18618313155586,41.32853117196495],[-79.19195513318786,41.32428217120739],[-79.20250913661447,41.32679817057028],[-79.20888113941976,41.331869171319774]]]},properties:{geoid:”42065″,name:”Jefferson”,state_name:”Pennsylvania”,county_state_name:”Jefferson County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.83,”40_35k_diff”:131.83,”60_35k_diff”:131.83,”27_65k_diff”:99.43,”40_65k_diff”:222.29,”60_65k_diff”:989.41,”27_95k_diff”:0,”40_95k_diff”:9.790000000000077,”60_95k_diff”:776.91,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.41,”40_65k_eptc”:460.42,”60_65k_eptc”:460.41,”27_95k_eptc”:559.84,”40_95k_eptc”:672.92,”60_95k_eptc”:672.91,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.87,”27_65k_no_eptc”:559.84,”40_65k_no_eptc”:682.71,”60_65k_no_eptc”:1449.82,”27_95k_no_eptc”:559.84,”40_95k_no_eptc”:682.71,”60_95k_no_eptc”:1449.82}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-76.93988537592816,40.638150133375355],[-76.92762737258052,40.64571513487032],[-76.9201103711701,40.65587813711906],[-76.91495236997831,40.66467013871434],[-76.9038513672514,40.674104141365206],[-76.8962533653373,40.67868214283424],[-76.88709036315949,40.68259714381775],[-76.87985236101403,40.68720014449526],[-76.87432435928652,40.6929131458696],[-76.86525935662442,40.7046141483077],[-76.86118635593319,40.71160615056564],[-76.85649435566683,40.72263815266689],[-76.85540935604647,40.735051154587005],[-76.85752335767532,40.74962015736064],[-76.85628335836286,40.754795158365496],[-76.85925435985067,40.777051162845744],[-76.8560963603354,40.79121916539816],[-76.85216535987203,40.800847167819434],[-76.84906835882175,40.80550116857012],[-76.84981735975815,40.80893816900033],[-76.84062835708737,40.821332171767125],[-76.82968735493546,40.83103717409476],[-76.81802835189433,40.84330117723425],[-76.81281434980428,40.84711417841852],[-76.81025334956811,40.8545731798576],[-76.80070634851397,40.87260318335964],[-76.79871634774426,40.87837418437519],[-76.80024434817499,40.88200218499756],[-76.80166234906407,40.879376184593305],[-76.80797635048505,40.87859318409021],[-76.82555735735393,40.88800318583532],[-76.83427136036109,40.889575185618604],[-76.84127036145634,40.886897184822146],[-76.84986836426604,40.88643618416462],[-76.85196636505776,40.888687184759426],[-76.85905836811389,40.889149184090265],[-76.878152373982,40.884507183220514],[-76.89124337835139,40.88866918352235],[-76.90528538249399,40.88497618224403],[-76.91923738643929,40.885198181033786],[-76.92779838970483,40.88739418106972],[-76.94070839399488,40.88803118133647],[-76.94714739574438,40.88576718027199],[-76.97001140271976,40.880936178315594],[-76.9731654030328,40.877140178106536],[-76.99366240995961,40.87514717690038],[-76.99535940964165,40.872728175940644],[-77.00483041286827,40.8721371756581],[-77.01131141489715,40.86877617414526],[-77.01547541574035,40.86093217264284],[-77.0198754162516,40.857937172491035],[-77.02490341859709,40.857497172047765],[-77.03186642067621,40.86412217241912],[-77.0432574245809,40.863674172767084],[-77.05202942782067,40.86939517331683],[-77.07406043394893,40.86834117189172],[-77.12957645132688,40.8538021673612],[-77.2436384848722,40.832017158695024],[-77.32164150936067,40.81711015213323],[-77.35663051877414,40.80734214893679],[-77.3553295149466,40.759422140162386],[-77.35409951060336,40.70167512903524],[-77.28794348934467,40.693603130207315],[-77.24101247417678,40.68766713103992],[-77.17132545249125,40.67906613172311],[-77.1505184452931,40.67708213195915],[-77.14909144546566,40.680546132557566],[-77.13984644280598,40.683592133772514],[-77.1250554384698,40.68580613481427],[-77.1095994336048,40.69158613651165],[-77.10152243117815,40.68898713647085],[-77.09745242864616,40.68209013505291],[-77.09732942919749,40.678373134656105],[-77.09360942723572,40.676129134179405],[-77.06808541984108,40.679848135599784],[-77.06580341914415,40.678285135886334],[-77.05328341456253,40.67519913543562],[-77.04577141270036,40.675645135891685],[-77.03934141071441,40.679966136817534],[-77.03555140961416,40.676926136755135],[-77.03544440805982,40.66852413539191],[-77.03242140704583,40.66468013458357],[-77.03441140759656,40.659936133373364],[-77.02950340624483,40.65557013317452],[-77.02575540496463,40.65607113266371],[-77.02251640440937,40.66089413375927],[-77.01915240261172,40.65950813410491],[-77.01379440117437,40.662172134647285],[-77.00842039977319,40.65992013482245],[-77.0079013985805,40.65194113265318],[-77.00404739649554,40.64558013149567],[-77.00605639805518,40.64262313159293],[-77.00313339615921,40.63872513040861],[-76.99755139398188,40.63588613057034],[-76.98804639182005,40.64359913212339],[-76.97658338859574,40.64538213305072],[-76.97644238829824,40.643077132675785],[-76.96860238560117,40.64123113218729],[-76.96546338477303,40.64722013395909],[-76.96181638414971,40.64568213341827],[-76.9452233791158,40.65034113532396],[-76.9406583769769,40.646183134553795],[-76.93988537592816,40.638150133375355]]]},properties:{geoid:”42109″,name:”Snyder”,state_name:”Pennsylvania”,county_state_name:”Snyder County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.84,”27_65k_diff”:188.06,”40_65k_diff”:330.38,”60_65k_diff”:1218.95,”27_95k_diff”:0,”40_95k_diff”:117.88,”60_95k_diff”:1006.45,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.42,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:648.48,”40_95k_eptc”:672.92,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:648.48,”40_65k_no_eptc”:790.8,”60_65k_no_eptc”:1679.37,”27_95k_no_eptc”:648.48,”40_95k_no_eptc”:790.8,”60_95k_no_eptc”:1679.37}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-79.68933527613534,41.16947912034348],[-79.68150127428069,41.16293111943461],[-79.6802472726846,41.15574911839148],[-79.68625327444197,41.14855711678488],[-79.68618727390948,41.14380111558659],[-79.6797102717183,41.137225114254754],[-79.67866826991664,41.13067611359766],[-79.67982126998805,41.125539112736405],[-79.6792772693661,41.11586911038757],[-79.68134326992855,41.10659710914628],[-79.68006026761216,41.09371810625139],[-79.67695226697064,41.08573810532415],[-79.67403626544716,41.08251810449971],[-79.66603626285844,41.07886310438338],[-79.65905425942941,41.07348610365012],[-79.65550625847295,41.06674210217122],[-79.65896725916848,41.06256510171677],[-79.66542626018179,41.05854610018663],[-79.66720326072088,41.05546009989999],[-79.66576526031952,41.04913109898814],[-79.66247625894655,41.047344098125016],[-79.65126025564686,41.04506509833156],[-79.63293924948832,41.037255097512464],[-79.61957824466378,41.03340409789704],[-79.61091024236457,41.03397309870447],[-79.60200823925138,41.037169099246256],[-79.59893523809971,41.0322190981841],[-79.60261023806227,41.020827096264874],[-79.60918923941779,41.012252094728325],[-79.60763023878515,41.00542409349687],[-79.59539623450476,41.00510009348832],[-79.58795423300386,41.003251093776306],[-79.5822562306974,40.99864909272217],[-79.58185622930476,40.993597091974806],[-79.58610223065145,40.991302090956566],[-79.59701623431856,40.99439609113168],[-79.60337123649042,40.99480609143884],[-79.61043023859604,40.993232090976825],[-79.61907024087189,40.98896808932655],[-79.62349424193606,40.98456808882739],[-79.62429324251123,40.97875308757594],[-79.61835523918171,40.97415008693723],[-79.60122023412134,40.969292086326405],[-79.59342523157267,40.968827086335864],[-79.58898623076358,40.97086508750056],[-79.58156322912761,40.98003008918595],[-79.57279022619385,40.98530809036567],[-79.56222622353528,40.98544509155814],[-79.553801219824,40.98170009118383],[-79.54533421811979,40.98225609144403],[-79.53943021620613,40.984296091771284],[-79.53582521420397,40.98007109133436],[-79.52861721244588,40.97842109131371],[-79.52168021014668,40.975076091150044],[-79.51468820806123,40.979033092524666],[-79.51776520934536,40.98305309234463],[-79.5140152081382,40.98681709349887],[-79.50667620578304,40.98308009337365],[-79.50334220433075,40.97643209168891],[-79.49366120083555,40.97790909256466],[-79.49478820211739,40.986189094603866],[-79.48852020043168,40.995377096174295],[-79.48172919816457,40.994078096149195],[-79.4756061969547,40.99491009660862],[-79.46954819540615,40.99346209704042],[-79.46466319253553,40.99031109610318],[-79.45696119118794,40.99115309663957],[-79.45589519047276,40.98818309664366],[-79.46188619207314,40.98529409536581],[-79.46187819193776,40.98268009519146],[-79.45102518805469,40.981738095187545],[-79.44475118660188,40.98644909679827],[-79.43962118489732,40.98741509671953],[-79.43065218229502,40.98536109672166],[-79.42465218079194,40.98897309825988],[-79.42086718003573,40.99904209980209],[-79.42027818008607,41.00398610102527],[-79.41288917793578,41.008325101835524],[-79.41006917708067,41.005306101391234],[-79.41503817897409,41.00071410089916],[-79.41349617733113,40.998245100020604],[-79.40659517613814,40.99858010001359],[-79.4042861747442,40.995672099635065],[-79.40602617497339,40.99103309876859],[-79.40178717298136,40.987858098841464],[-79.39746617263533,40.990070099380375],[-79.3947171718319,40.99475809982042],[-79.38946417029155,40.9935590998543],[-79.37966616747927,40.99510810064422],[-79.37798216618698,40.99077509986516],[-79.38554016862464,40.98977409931418],[-79.38305916744434,40.98498509903689],[-79.37476516513422,40.98374809943403],[-79.38097716601612,40.979889097691185],[-79.38219416552539,40.97119309598035],[-79.37908916465507,40.96841409576728],[-79.37425216338497,40.96889709614984],[-79.3695631620287,40.974928097793274],[-79.37156916336916,40.98256909866172],[-79.37101816391466,40.990173100800746],[-79.3659741629707,41.00080810300363],[-79.36102916172722,41.0037711035241],[-79.35634416026572,40.99980410297233],[-79.34503815579195,40.998078102938635],[-79.34159915511832,41.00138810391991],[-79.3360381535404,41.00011510383581],[-79.32027314866214,41.00154510495744],[-79.3024791442184,41.013543107557744],[-79.29949614292613,41.01176910730565],[-79.28500113851052,41.00930310751323],[-79.28152213781216,41.010372108050646],[-79.2739881358208,41.017623109612956],[-79.26757313334844,41.020233110905906],[-79.26065913244923,41.0293531126086],[-79.24204912732014,41.03535111484478],[-79.2364821261477,41.04203911616071],[-79.23006512467299,41.0460281173461],[-79.21906812079983,41.048593117587814],[-79.21521711998865,41.05052311844085],[-79.2144971222464,41.07878312423414],[-79.2113231206853,41.07874512377721],[-79.2111841225111,41.112345129921415],[-79.21020112753713,41.17367114227784],[-79.20977813315318,41.24995515577148],[-79.20917013610776,41.2925651638198],[-79.20888113941976,41.331869171319774],[-79.20787514383271,41.39532018307157],[-79.20707514462796,41.41754918747527],[-79.20719914587748,41.4309301904883],[-79.23823015547583,41.43135118860565],[-79.35765619292512,41.43244018425832],[-79.35758919358544,41.43624918503158],[-79.40027220653694,41.436153182452536],[-79.40044220355337,41.38658717331184],[-79.4778252278428,41.386487170539894],[-79.47814322323372,41.33571616107335],[-79.54143324326604,41.33595915761161],[-79.5414772424663,41.321016155000684],[-79.6041642617762,41.32148615244976],[-79.60461325845034,41.27708014388582],[-79.62756426564562,41.27719114353313],[-79.62772926477071,41.26691514112473],[-79.63271326627732,41.26692714121845],[-79.63287826583614,41.25360713840086],[-79.65039727079896,41.25371713819119],[-79.64963126825366,41.217920130805666],[-79.66889527309463,41.199083126576596],[-79.66652227199431,41.19649912595616],[-79.67061727250189,41.19317412560253],[-79.66537127085792,41.18903212544514],[-79.67021627167387,41.1845521244017],[-79.68388027616982,41.18438712299532],[-79.6905662781636,41.181491122681315],[-79.69724528062528,41.18462212320787],[-79.7003362810235,41.18179812190814],[-79.70058428057582,41.17506712133034],[-79.69498727892389,41.17287312109327],[-79.68933527613534,41.16947912034348]]]},properties:{geoid:”42031″,name:”Clarion”,state_name:”Pennsylvania”,county_state_name:”Clarion County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.84,”40_35k_diff”:131.83,”60_35k_diff”:131.83,”27_65k_diff”:19.84,”40_65k_diff”:125.24,”60_65k_diff”:783.31,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:570.81,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.05,”27_65k_eptc”:460.42,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:480.26,”40_95k_eptc”:585.66,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.88,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:480.26,”40_65k_no_eptc”:585.66,”60_65k_no_eptc”:1243.73,”27_95k_no_eptc”:480.26,”40_95k_no_eptc”:585.66,”60_95k_no_eptc”:1243.73}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-78.36062182975648,40.733189094202096],[-78.36639383189816,40.73605109408621],[-78.3730198349116,40.74990009717618],[-78.37664283573866,40.751969097086494],[-78.373425835091,40.757561098487095],[-78.3652588334038,40.76455309983941],[-78.35913583160405,40.76790310038936],[-78.35225482897566,40.76858710116539],[-78.3501498287854,40.7761141027577],[-78.34258082685874,40.78190310439554],[-78.342581827671,40.790879105848454],[-78.34025182756649,40.791570106193305],[-78.33947082781995,40.79794110729513],[-78.33166382534587,40.8011301084516],[-78.32692882377256,40.80590710956572],[-78.32047282228332,40.808207110518026],[-78.3137538201987,40.80856611047514],[-78.31163481978953,40.81390011153664],[-78.30801081919343,40.8157281124495],[-78.30562781841513,40.82064611346508],[-78.29938581731429,40.82456811447266],[-78.29997281756037,40.83142411556765],[-78.3019858183367,40.83350311575155],[-78.29443981651804,40.837927116446394],[-78.29060281556268,40.842528118070675],[-78.29131881608356,40.846756119006926],[-78.2842398138621,40.851057119589086],[-78.27773181179175,40.851001120010096],[-78.2738298105148,40.848063119165964],[-78.26717180874694,40.85027212018709],[-78.25735180535034,40.85542412163382],[-78.24922280315899,40.85539112242353],[-78.24897780366365,40.86952712501007],[-78.23611179988619,40.873263126401866],[-78.23972780233798,40.876914126833654],[-78.24647780439723,40.87585212644801],[-78.24776380410091,40.87956512690255],[-78.24298980283749,40.88148712739186],[-78.23004079931516,40.88030712719475],[-78.22793979864312,40.886741128658436],[-78.22122479724577,40.88876912914252],[-78.22133579691912,40.89217712998118],[-78.2288387995872,40.90107913156541],[-78.22594479931146,40.907408133206296],[-78.21981579829216,40.91274913414659],[-78.20941679547848,40.91738013552938],[-78.20163979274498,40.915821135750086],[-78.19598779126267,40.920000136972774],[-78.19043778924328,40.91868013630621],[-78.17987778597123,40.923567137987455],[-78.17794378654932,40.92915713878678],[-78.17148378422623,40.93242613997584],[-78.17128178447886,40.93677514079508],[-78.16646378306051,40.93669414136027],[-78.16245678161197,40.94207714195426],[-78.15581277972994,40.94144514223568],[-78.15941478194235,40.950374143886776],[-78.16272678264814,40.95469114416963],[-78.1676577849111,40.95193914337735],[-78.16897978509462,40.95962514553665],[-78.16512778448178,40.96160014543977],[-78.15850978271791,40.96093714619572],[-78.15160678021913,40.957374145135724],[-78.1468557787838,40.95659414511887],[-78.14772677828415,40.95005614456521],[-78.14106177656902,40.94985214430284],[-78.13965077636118,40.95711014613599],[-78.13644977485933,40.96142114729332],[-78.1363537756708,40.96602614789332],[-78.13197177401759,40.96591414767473],[-78.12996677384501,40.961849147070396],[-78.1363787744863,40.95602914605952],[-78.13062377296579,40.951349145112225],[-78.13406577318766,40.9472251440616],[-78.12703677134408,40.945689144100925],[-78.1202717689206,40.9419381440227],[-78.11133676681196,40.9451321449446],[-78.10998076618169,40.94955514557577],[-78.10421676393248,40.94952614578963],[-78.09926576255701,40.95159714621295],[-78.0949027612194,40.950444146266314],[-78.08957075977321,40.95446614717887],[-78.08150875722927,40.955072148135706],[-78.07774275658814,40.95883214837656],[-78.0840517595006,40.96773915036291],[-78.08814976135773,40.970329150767384],[-78.09052476238585,40.98088915281977],[-78.08443076103734,40.9808391529671],[-78.08183776024526,40.98542215374888],[-78.08470476123739,40.99090015451343],[-78.07361075758214,40.99394515537484],[-78.0681177568717,40.997653156320844],[-78.06185275436155,40.997908156964996],[-78.06514075630687,41.003346157902904],[-78.05616575273264,41.004264158402535],[-78.05595875359441,41.00828115910062],[-78.06200475555039,41.01327915970903],[-78.06983375797628,41.01470215950643],[-78.0678917581717,41.01949216097218],[-78.07560176091773,41.02219316057717],[-78.07990576253218,41.02948816235476],[-78.07616576201417,41.03448716325498],[-78.06927175909229,41.03272916326948],[-78.06562275822559,41.03578816418296],[-78.05726075617851,41.03935916529075],[-78.06408275924113,41.045921166037104],[-78.05938775774723,41.05084216716407],[-78.06236575866208,41.053238167023004],[-78.06820576035712,41.04996716678468],[-78.07285176182859,41.051930166454675],[-78.07556276374258,41.05966516783401],[-78.0846207665965,41.057400167668206],[-78.09065376747267,41.059420167186055],[-78.08563976725755,41.06865816977541],[-78.09575477004176,41.07091116984539],[-78.0926737706756,41.07957017090247],[-78.09811377269453,41.08604717175381],[-78.10761677642566,41.10551817572859],[-78.11225277829128,41.11364817726734],[-78.10870477806381,41.11765317790334],[-78.10034777607083,41.12179117923023],[-78.0947597741157,41.119674178628436],[-78.09037277185357,41.11564117790185],[-78.08759777096284,41.117181178329524],[-78.08644977075971,41.123581179350104],[-78.08414077103954,41.12595318041597],[-78.07767476870151,41.12517518013573],[-78.07373476745106,41.12206318016734],[-78.06866176562743,41.12431618029312],[-78.0704347669897,41.12898918112113],[-78.0655917658476,41.13234918266751],[-78.05884676267502,41.13091718206315],[-78.05483876214684,41.134185182787874],[-78.05273576252893,41.14532518529438],[-78.04344275944577,41.146516186239666],[-78.03817375791068,41.15361118726554],[-78.06100976701974,41.17454719044932],[-78.09338378033888,41.21693919696318],[-78.18824381039407,41.226002194665746],[-78.23681982615311,41.23048319410352],[-78.32398485462899,41.235147190564604],[-78.44589289307027,41.241839186853895],[-78.53195092005032,41.24646418435875],[-78.57869993550045,41.24959018287462],[-78.64666895660407,41.25378618130476],[-78.64794995443046,41.217468174043],[-78.71025097311792,41.201867168791466],[-78.76637999048735,41.20276716623405],[-78.781192993038,41.174794160524534],[-78.80453499787805,41.132194151314394],[-78.8045549941375,41.09077014365945],[-78.8040439892539,41.01819912942067],[-78.80404998435297,40.95182211683906],[-78.80516998044637,40.905988108225486],[-78.80640897789499,40.861626099878954],[-78.80660097280092,40.78031108493815],[-78.80627696788675,40.72975007456231],[-78.80172896714336,40.724626073812],[-78.69194493265458,40.7243440783578],[-78.63558491424357,40.72307408075504],[-78.56902589383435,40.72565008393748],[-78.52983088200665,40.72592708535565],[-78.47201486374082,40.72550708814574],[-78.40290184213443,40.72524709117394],[-78.34867082451186,40.72345109278674],[-78.36062182975648,40.733189094202096]]]},properties:{geoid:”42033″,name:”Clearfield”,state_name:”Pennsylvania”,county_state_name:”Clearfield County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.83,”40_35k_diff”:131.83,”60_35k_diff”:131.83,”27_65k_diff”:99.43,”40_65k_diff”:222.29,”60_65k_diff”:989.41,”27_95k_diff”:0,”40_95k_diff”:9.790000000000077,”60_95k_diff”:776.91,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.41,”40_65k_eptc”:460.42,”60_65k_eptc”:460.41,”27_95k_eptc”:559.84,”40_95k_eptc”:672.92,”60_95k_eptc”:672.91,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.87,”27_65k_no_eptc”:559.84,”40_65k_no_eptc”:682.71,”60_65k_no_eptc”:1449.82,”27_95k_no_eptc”:559.84,”40_95k_no_eptc”:682.71,”60_95k_no_eptc”:1449.82}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-74.2032925046407,40.593050225545646],[-74.19959050398431,40.60039022795838],[-74.20483450599261,40.60607022828183],[-74.20242650512641,40.616778230890965],[-74.20392650639235,40.62437823227678],[-74.2024015059173,40.63160023330036],[-74.1914315035739,40.64203323586709],[-74.18564250137977,40.64605023736334],[-74.18165150120224,40.64653623711548],[-74.1614294943361,40.64415623718283],[-74.13670448743999,40.674452244119436],[-74.13577648783026,40.67556724425643],[-74.14898549234518,40.68224424540136],[-74.15386249457364,40.68592524634649],[-74.15786249495102,40.685960245751],[-74.16505149789485,40.690169246390894],[-74.16992849895331,40.68855724582431],[-74.20154850934813,40.68668024402935],[-74.20924951169552,40.69071724469837],[-74.21300951421227,40.700916246516236],[-74.22195051722285,40.707349247541394],[-74.25584652864714,40.71337724740976],[-74.28552653879517,40.722270248478154],[-74.29258054076988,40.72091124787862],[-74.29721354175868,40.71519724624839],[-74.30352454363133,40.71319624610456],[-74.30925454542917,40.71444724645101],[-74.31628254824221,40.71927224659526],[-74.32559755125904,40.71708324633185],[-74.34268355737836,40.72518924729304],[-74.34866455884585,40.73022924749864],[-74.35894056321804,40.73598324873502],[-74.3717395670528,40.73964824863419],[-74.37200656673832,40.73408324750315],[-74.37774856887981,40.73435624766595],[-74.3776505685411,40.730342246353956],[-74.38438857060156,40.724422245144844],[-74.39104657203949,40.72452624523783],[-74.39074157221245,40.718530243757705],[-74.39615857397726,40.71725024366309],[-74.40232457528501,40.71799224376817],[-74.40896957755955,40.709816241909394],[-74.42150958110746,40.70320123990397],[-74.4268155826904,40.70185323898389],[-74.43454958402745,40.693570237773386],[-74.44819958808068,40.68549123504487],[-74.45190458919278,40.68540523504419],[-74.45153558866772,40.679595233771785],[-74.45484858918921,40.674051233256684],[-74.46103659130726,40.67351223242889],[-74.45084758730562,40.654156229118556],[-74.44308558436371,40.657659230551054],[-74.43277458236567,40.66467123150512],[-74.42929358074134,40.66461823203853],[-74.41985757704778,40.65768323115216],[-74.40513157340209,40.66778223382017],[-74.40180157186245,40.66448923333982],[-74.40336157231842,40.65409623111949],[-74.4069875724962,40.65073423036836],[-74.4085625726736,40.644295228802754],[-74.41442157503477,40.6406602282759],[-74.41493557439942,40.63247822576574],[-74.41764757518759,40.627549224828684],[-74.4228165764474,40.62501122457517],[-74.42319857621501,40.621158223948186],[-74.42794757726692,40.61657622223414],[-74.43142457807575,40.615671222149274],[-74.43652657964941,40.610937221602136],[-74.44569258293463,40.60900922066803],[-74.45037258343311,40.60418121973225],[-74.45446458574371,40.603667219277916],[-74.46329258721104,40.599195217536355],[-74.45690558498798,40.59580821708324],[-74.30292253761078,40.6086912257206],[-74.30532753751875,40.600594223446514],[-74.29994953570335,40.59812822360806],[-74.29099153223036,40.59193322290863],[-74.25956052216348,40.59732122479093],[-74.25769052269196,40.60228422599155],[-74.25296952060683,40.60077622574633],[-74.24166751701013,40.599564225792726],[-74.2353795154607,40.60247522684815],[-74.22974651357094,40.598834225777495],[-74.21247250760375,40.60282922776658],[-74.21150550741156,40.598329226786845],[-74.2032925046407,40.593050225545646]]]},properties:{geoid:”34039″,name:”Union”,state_name:”New Jersey”,county_state_name:”Union County, New Jersey”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:84.32,”60_65k_diff”:696.41,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:483.91,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.05,”27_65k_eptc”:446.7,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:446.7,”40_95k_eptc”:544.74,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:446.7,”40_65k_no_eptc”:544.74,”60_65k_no_eptc”:1156.83,”27_95k_no_eptc”:446.7,”40_95k_no_eptc”:544.74,”60_95k_no_eptc”:1156.83}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-79.21531310952638,40.911354092495806],[-79.21520710502074,40.848648079983356],[-79.21490410065005,40.78851406890591],[-79.21521809915843,40.775950066716405],[-79.27693811436659,40.71106205185264],[-79.37783313688847,40.603967027044746],[-79.45017915470932,40.530157009435285],[-79.44964315429495,40.52680000884371],[-79.45654815642561,40.52324500773714],[-79.45974115606226,40.5167450066152],[-79.45455115372746,40.507022005209365],[-79.45530015353216,40.496624002967614],[-79.4524651522273,40.4894380016158],[-79.45401415300309,40.485515001027935],[-79.44754015042088,40.48081900042509],[-79.43846314809879,40.48674500213506],[-79.4306311453194,40.489054002472166],[-79.42357714170551,40.47333699959164],[-79.42131814070379,40.470605999423476],[-79.41569313990573,40.47057999996232],[-79.40663413680969,40.47430900070217],[-79.39546413260949,40.457139997791835],[-79.39110513052825,40.45441999767945],[-79.38175612728591,40.45270499811449],[-79.37419412533366,40.45370099823097],[-79.36959412465934,40.45661199936056],[-79.3663371233842,40.46597400135002],[-79.36707312440504,40.47509800240801],[-79.36592812408546,40.47748200346486],[-79.35859812278684,40.47792400322685],[-79.35803212171645,40.47088700197612],[-79.36227812163996,40.460068999616894],[-79.36052912117806,40.454102999204274],[-79.35385411854209,40.45170899896211],[-79.34592911713678,40.45483300001816],[-79.34541111722568,40.467220001782536],[-79.33844311507272,40.470006003029496],[-79.33173511227638,40.46189700198271],[-79.33027011142069,40.45385899983845],[-79.3254121103845,40.45270700007633],[-79.32278910939257,40.45604000126323],[-79.31610310803087,40.45926100213129],[-79.30035410316223,40.46097800322258],[-79.29763410177054,40.45580400221964],[-79.30168010244839,40.45136400088206],[-79.29990010199404,40.4449199993294],[-79.30175410164283,40.439298998662004],[-79.29943810112218,40.43452299807307],[-79.28941209737626,40.43668099869458],[-79.28285109613083,40.442777000411056],[-79.27260809314643,40.43909000016678],[-79.26935409098053,40.42852499784273],[-79.27354509151246,40.422932996728996],[-79.27285909148482,40.41841899617886],[-79.26328408825277,40.4167709955048],[-79.25411708575506,40.42229599694649],[-79.24757108488734,40.43208799950256],[-79.24017808164469,40.42999899905817],[-79.23320608010897,40.43074899952313],[-79.21478607385926,40.424465999539564],[-79.20651607012762,40.4150399978309],[-79.19923606787684,40.410787997755754],[-79.19120006594908,40.41522899841474],[-79.17371605975194,40.4106299989492],[-79.1643720572946,40.41023199857873],[-79.15579205458442,40.4117729997382],[-79.15205405300733,40.4087739991369],[-79.15400505320129,40.40170899735387],[-79.14789505058616,40.39760799677088],[-79.13500804704871,40.398311998169],[-79.12475204418307,40.39536899726114],[-79.11700304145873,40.3942509973683],[-79.11490904031105,40.389886996737076],[-79.12250604226719,40.38936199679839],[-79.12868004434682,40.38506399547422],[-79.12711904284573,40.375075993543106],[-79.12163704112788,40.370583993044505],[-79.10931203775642,40.37332599361365],[-79.10215603456905,40.36887599350939],[-79.09677203331074,40.37073299439597],[-79.096119033003,40.374042994758845],[-79.09053003163008,40.38025099659631],[-79.08831503133396,40.38656099773153],[-79.08296803022239,40.38958999844364],[-79.07448602758457,40.38582799806249],[-79.06988802545642,40.38042199694783],[-79.06455602397669,40.379009996678235],[-79.05848402259024,40.38087599782589],[-79.05711202178956,40.384300998055295],[-79.05188802111722,40.38929399989577],[-79.04243901767931,40.39138999986736],[-79.03983801687225,40.396281001283896],[-79.0363310166461,40.396004001124794],[-79.0277170145283,40.406144003641266],[-79.03426501631442,40.40976200445701],[-79.03301001659936,40.41678200589837],[-79.02784001488001,40.41958200614987],[-79.0166200119986,40.42028700657895],[-78.99664000482167,40.41326400612057],[-78.98887300291068,40.41198200613921],[-78.98232700063075,40.40578700592496],[-78.97381699652537,40.3954290037767],[-78.94609899120111,40.441758013644474],[-78.92192598691554,40.483520022642104],[-78.88594898069252,40.55407503800625],[-78.85968897651924,40.60705204955588],[-78.85067397514639,40.62634405338336],[-78.82668897143158,40.681758065114686],[-78.80886496898687,40.72107007278191],[-78.79964396582201,40.71727207274196],[-78.80172896714336,40.724626073812],[-78.80627696788675,40.72975007456231],[-78.80660097280092,40.78031108493815],[-78.80640897789499,40.861626099878954],[-78.80516998044637,40.905988108225486],[-78.86747400050072,40.90622710554256],[-78.94642402552712,40.90844710258313],[-78.99975804231453,40.90914610122693],[-79.0699320642312,40.90980109819462],[-79.12472708101028,40.910579095423174],[-79.21531310952638,40.911354092495806]]]},properties:{geoid:”42063″,name:”Indiana”,state_name:”Pennsylvania”,county_state_name:”Indiana County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:122.53,”40_65k_diff”:250.46,”60_65k_diff”:1049.23,”27_95k_diff”:0,”40_95k_diff”:37.96,”60_95k_diff”:836.73,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.05,”27_65k_eptc”:460.41,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:582.94,”40_95k_eptc”:672.92,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:582.94,”40_65k_no_eptc”:710.88,”60_65k_no_eptc”:1509.65,”27_95k_no_eptc”:582.94,”40_95k_no_eptc”:710.88,”60_95k_no_eptc”:1509.65}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-76.9149723475798,40.32849207415658],[-76.91727234909479,40.332723074200416],[-76.9261823519384,40.34098807583628],[-76.92852335361007,40.34799307714929],[-76.93267435452191,40.35532607808746],[-76.93754935719393,40.3574890781702],[-76.96115236402991,40.35804107795481],[-76.97062736684151,40.35631307693482],[-76.98199837040093,40.357328076707354],[-76.99802437599497,40.35668707628473],[-77.00819337868134,40.35845707633103],[-77.01918038347867,40.36479307638985],[-77.02165238384814,40.36837607732739],[-77.02306938452588,40.37640707888868],[-77.02684338677759,40.38054807963006],[-77.02914638733353,40.38662108097122],[-77.02864738797967,40.3912050816005],[-77.02147138627397,40.39792808275546],[-77.01312738396928,40.40235708390083],[-77.01173638335233,40.407420085635806],[-77.0158493858497,40.41565808643745],[-77.0162723859632,40.42518108866887],[-77.00323738162888,40.42680808905617],[-76.99791738045631,40.43367809120451],[-76.98943237801534,40.438171092561404],[-76.9804543762205,40.44714409423317],[-76.96949837337904,40.45274009619361],[-76.9611453701622,40.45579809704878],[-76.95281136906067,40.462475098438276],[-76.9493993682219,40.46904509972373],[-76.94946836908707,40.48453510286069],[-76.95308537037515,40.490629103392244],[-76.96909237641292,40.49757010482572],[-76.9783533798435,40.50715710621244],[-76.98510638193332,40.51635710786342],[-76.98566538275155,40.52500510916726],[-76.98153238272425,40.531931110479235],[-76.98054838188659,40.53834011177554],[-76.98199138343647,40.54342311308903],[-76.99186438787949,40.56128011619062],[-76.99239838828788,40.56788511761984],[-76.98816338713436,40.5745931190414],[-76.98367538565506,40.57826711969231],[-76.96527038138056,40.58706812188669],[-76.95875737940123,40.59286312300894],[-76.95310737857493,40.60451212606339],[-76.95355337937883,40.61477812813541],[-76.95083837954778,40.62705213019682],[-76.9491503790798,40.62817513019318],[-76.95607938104474,40.62794613012942],[-76.98765239004382,40.61619812698259],[-77.0001103935426,40.61092312484658],[-77.02330640031748,40.60426812268404],[-77.03297640317042,40.603454122875675],[-77.04195640573404,40.60423112265713],[-77.04727140820279,40.60253112164654],[-77.0699934145328,40.59847212026317],[-77.08729441974072,40.598060119038585],[-77.10331642451855,40.595913118421585],[-77.10679242529616,40.59279811716466],[-77.11892543000536,40.59265811714347],[-77.12806143208249,40.59083411614441],[-77.15913744200417,40.586575114370426],[-77.1634554436564,40.58691511412517],[-77.18293244862386,40.58214811214435],[-77.16756344293289,40.559517108540604],[-77.17378144441929,40.557509107949876],[-77.1829524475627,40.55670410788595],[-77.19846445232753,40.5522951057403],[-77.21645945695374,40.544425103634005],[-77.23169846174866,40.53849210250056],[-77.26816647226188,40.52609109854339],[-77.2806064757342,40.520115096848585],[-77.28959447877499,40.51846509557818],[-77.33811249177337,40.49534408947147],[-77.41343551332824,40.46059708028628],[-77.42902951731605,40.45447607793624],[-77.43653952019184,40.45056207671989],[-77.44589052270803,40.44716807616138],[-77.47142252957264,40.43492107294298],[-77.50064553794873,40.420344068364464],[-77.5090245408102,40.41515206770013],[-77.51708754203912,40.41161606668161],[-77.54014354862666,40.39922906288065],[-77.53226754543513,40.376014058930906],[-77.54061654705615,40.375568058110765],[-77.5656675552933,40.3673710558219],[-77.5827965592795,40.35704905349398],[-77.59943056360483,40.34815505050505],[-77.61366156770639,40.3376810485007],[-77.6361415738504,40.322382044360126],[-77.65487657898359,40.30684804039718],[-77.67176358289021,40.2898330364985],[-77.66419757991947,40.280487035436],[-77.66427757935737,40.2782350345708],[-77.65641857629602,40.27040103369397],[-77.67115758088666,40.25757703069231],[-77.66549657787078,40.2520570297418],[-77.65344957532253,40.257415030613544],[-77.64950457389344,40.257559031209254],[-77.64502557256498,40.25394003097892],[-77.64999257285805,40.247965029436806],[-77.6454045713883,40.23893602785322],[-77.6488805716105,40.23332702643298],[-77.64995357170969,40.22629102467102],[-77.64764457017421,40.22248502408327],[-77.64339656973598,40.22317302473192],[-77.6398955678107,40.21768602370747],[-77.61616956175519,40.23262402781053],[-77.6091735588517,40.23276102800948],[-77.60277255679551,40.227496026806705],[-77.60489055781069,40.22493002622222],[-77.60477055610303,40.206041023137125],[-77.61466755826257,40.19855702088096],[-77.60545055528891,40.185370019188916],[-77.59355155143913,40.192018020704175],[-77.58995655075746,40.196522021781604],[-77.58044154851115,40.20386402363791],[-77.57834354808078,40.206634023803595],[-77.55808754286039,40.21864602699602],[-77.53687053608476,40.21908002821808],[-77.5289625330851,40.223007029644194],[-77.52675253320862,40.22559502991641],[-77.51550453014421,40.230512031077474],[-77.5101115278797,40.23442403215758],[-77.49731752427576,40.24024203413281],[-77.47359851801096,40.254224037250374],[-77.45782751455741,40.26613304026262],[-77.42659750611647,40.286618045416496],[-77.41378050195905,40.29390004742209],[-77.39444749722165,40.30351404986697],[-77.37569549189458,40.31069905229271],[-77.36602048899572,40.31357705322017],[-77.35763748539206,40.31248405350054],[-77.35987548619212,40.30669205249854],[-77.36476448748547,40.30254905111449],[-77.38696949354238,40.29035904832294],[-77.40289549803113,40.28013604562931],[-77.40930649928767,40.2745620439207],[-77.4110464998079,40.26932304330172],[-77.41979750189802,40.26407804152201],[-77.42317950268756,40.257938040069504],[-77.42084750231393,40.25537603989065],[-77.41386149942471,40.25522303983139],[-77.40245949668117,40.256962040948736],[-77.38511649136673,40.26272004283205],[-77.36072048453421,40.274709046158776],[-77.35430148247245,40.279286047416655],[-77.3406494783709,40.28692304923486],[-77.32856347555925,40.29231905033048],[-77.32392647308134,40.28861304970358],[-77.33069847487232,40.28059604786855],[-77.33049347535214,40.275604047576735],[-77.31729046984046,40.26759804612952],[-77.31223746859462,40.26774804685073],[-77.29157846283489,40.27281004822479],[-77.27005945633663,40.278660049958674],[-77.24169344772527,40.282855052378004],[-77.23916544728948,40.28411005237907],[-77.23090444416016,40.28357905296561],[-77.20449843550442,40.287088054870914],[-77.18279742881937,40.28775105517615],[-77.15039941949816,40.291260057307255],[-77.13485141477915,40.29491205912723],[-77.12264641090957,40.296872059166894],[-77.10174640486528,40.29864906108243],[-77.09636740302945,40.300403061541836],[-77.07466239644874,40.30224406203107],[-77.06387639245986,40.30197506255507],[-77.05966139116335,40.30330106337466],[-77.04177138639874,40.30441006416469],[-77.02452138008121,40.303966065024014],[-77.00513037431072,40.30562506600991],[-76.97422136539738,40.31033806793827],[-76.94928435776241,40.31686907052365],[-76.9149723475798,40.32849207415658]]]},properties:{geoid:”42099″,name:”Perry”,state_name:”Pennsylvania”,county_state_name:”Perry County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.83,”60_35k_diff”:131.83,”27_65k_diff”:230.11,”40_65k_diff”:381.65,”60_65k_diff”:1327.83,”27_95k_diff”:17.61,”40_95k_diff”:169.15,”60_95k_diff”:1115.33,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.05,”27_65k_eptc”:460.41,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:672.91,”40_95k_eptc”:672.92,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:690.52,”40_65k_no_eptc”:842.07,”60_65k_no_eptc”:1788.25,”27_95k_no_eptc”:690.52,”40_95k_no_eptc”:842.07,”60_95k_no_eptc”:1788.25}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-79.69498727892389,41.17287312109327],[-79.71882228601292,41.172654119861676],[-79.82448431938549,41.1731301149914],[-79.86929633251893,41.172749112698355],[-79.90642734426451,41.172128111166884],[-79.95929336029933,41.17166510885666],[-79.99978237287708,41.17186910683948],[-80.04706738403006,41.1206480953041],[-80.09686439529027,41.069812083872456],[-80.09829739613338,41.07106208385771],[-80.16647541266701,41.00093606771058],[-80.15853339818746,40.85510404053717],[-80.15551339286351,40.79224302938789],[-80.15195038744453,40.73341401817142],[-80.15106538492087,40.713146014559456],[-80.1485003817312,40.67377700705386],[-80.12779437559725,40.6736120077141],[-80.10106136714174,40.67401700885313],[-80.07143735795084,40.674943010491106],[-80.07139635745709,40.6741820106137],[-80.02100934179832,40.674069013000185],[-79.98784533201541,40.673595013884636],[-79.95994232333577,40.672288015290924],[-79.91462930973557,40.673294017332765],[-79.87523729728055,40.672405018402344],[-79.85155929008795,40.672296019182454],[-79.82943628254102,40.6711500205172],[-79.81873227919145,40.67171602045886],[-79.78065426769724,40.67123602208621],[-79.7327472529399,40.6692480241209],[-79.70754924437438,40.66985902539147],[-79.692881240698,40.66961902576937],[-79.69293324021642,40.66975202619481],[-79.69235524321277,40.710868034004804],[-79.69328724532504,40.741435039290174],[-79.69280624881225,40.793413049135474],[-79.69212725110617,40.813424053192826],[-79.69169925494529,40.875080065014814],[-79.6899282611156,40.957049080476786],[-79.69019526697713,41.0467160971695],[-79.69027527205961,41.103260108005195],[-79.68878127372258,41.13343711378472],[-79.68933527613534,41.16947912034348],[-79.69498727892389,41.17287312109327]]]},properties:{geoid:”42019″,name:”Butler”,state_name:”Pennsylvania”,county_state_name:”Butler County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:26.92,”60_65k_diff”:574.51,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:362.01,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:399.63,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:399.63,”40_95k_eptc”:487.34,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.87,”27_65k_no_eptc”:399.63,”40_65k_no_eptc”:487.34,”60_65k_no_eptc”:1034.93,”27_95k_no_eptc”:399.63,”40_95k_no_eptc”:487.34,”60_95k_no_eptc”:1034.93}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-75.4813618376742,39.38756294134767],[-75.53112685524965,39.43020494801769],[-75.56053986659349,39.455652952106966],[-75.5635878688975,39.48305595749206],[-75.55909186818916,39.49581395974567],[-75.54648786441903,39.49624996049828],[-75.52786285838252,39.49814696128328],[-75.53005285968447,39.50482496250536],[-75.53002386051547,39.51042196402218],[-75.52667286003503,39.53022296817846],[-75.52780086036954,39.53537196865466],[-75.53196986223118,39.537172968886],[-75.53341386336747,39.542051970523204],[-75.51814585956733,39.55669197395864],[-75.51196185718844,39.5672979757999],[-75.51277185870136,39.57829797783138],[-75.51806686082196,39.58284797873376],[-75.52769486333752,39.58411997883624],[-75.53128086555719,39.58870497961562],[-75.54214786902021,39.59452698007045],[-75.55031987206647,39.60077398107282],[-75.55339987229007,39.60177398092613],[-75.55697587413687,39.60758398197511],[-75.55890987592245,39.61849098401618],[-75.55877487590048,39.629994986890146],[-75.55426787545092,39.635573987699885],[-75.54853587322518,39.63777798872445],[-75.54197987208845,39.645432990068066],[-75.53352586938804,39.64756499127619],[-75.52783086761774,39.65307199206333],[-75.52183986694848,39.66099599437606],[-75.51600986510411,39.66576599532928],[-75.51219186437685,39.671774996439346],[-75.50925386342328,39.684871999698714],[-75.50929286493987,39.69420300104813],[-75.5065378635126,39.697271002471645],[-75.49631386051693,39.700964003414825],[-75.48838585872033,39.71471600578178],[-75.48188485703243,39.713694006328254],[-75.47652085526788,39.716109007103434],[-75.47555885611315,39.733540010281374],[-75.46939785462148,39.74286901269091],[-75.46355185387763,39.75702201509467],[-75.46392285469757,39.760771015833235],[-75.45944185354223,39.76581901765757],[-75.4523408515033,39.76902101815213],[-75.45029485078636,39.77528701985075],[-75.43830184789611,39.78441002195263],[-75.4054908380238,39.79637602586484],[-75.41506384127008,39.80192702624302],[-75.42310584380418,39.806717026961586],[-75.44050885059772,39.81515002770103],[-75.45349185457304,39.820465028949954],[-75.46818885973654,39.82557902905007],[-75.48104086406371,39.829327029295946],[-75.49834686986841,39.83338802972945],[-75.52030787631298,39.83701302916815],[-75.53497888103709,39.838539029448185],[-75.55740488861024,39.83951502845034],[-75.5799278957566,39.83887002766236],[-75.59310089976104,39.8377310267107],[-75.59488189980355,39.837533026428815],[-75.61036590508304,39.835368025415335],[-75.62434890893473,39.83270302519231],[-75.64234591433524,39.82822502357378],[-75.66660192191412,39.81997102078859],[-75.6804699260872,39.8139470186002],[-75.70009093168886,39.80348601623808],[-75.71950393638274,39.79037301323469],[-75.73299793992243,39.77911501016377],[-75.74203094237079,39.77026400796413],[-75.75405794530192,39.75618600522821],[-75.76636494831922,39.737494000527256],[-75.77378794930112,39.722207997710704],[-75.78859795420743,39.72220699721962],[-75.78852294991229,39.64814098165294],[-75.77698893736077,39.5060409540078],[-75.76572092538457,39.36676592690574],[-75.7600759199095,39.296826912337124],[-75.71490290499007,39.29937391442228],[-75.68518989656324,39.29709691568285],[-75.68026289409772,39.292503915114],[-75.67556289279321,39.290660914274035],[-75.66727089049712,39.2904249146512],[-75.6604778877597,39.29167991492333],[-75.6511608851393,39.29160191568583],[-75.64845188494728,39.295442916576675],[-75.64084288228106,39.30146191802147],[-75.6325928799449,39.30128091863297],[-75.62576587736699,39.30415391882327],[-75.61963287665046,39.31006592078084],[-75.60659987190148,39.30809792046265],[-75.59496486843953,39.309934921324164],[-75.59133686730519,39.31164592133041],[-75.58434286503793,39.30872592144746],[-75.57443086167224,39.31361892254676],[-75.56871786070096,39.32353092511672],[-75.56900886083473,39.32875192604759],[-75.5648078601699,39.33194392678233],[-75.55620685764345,39.33533292806377],[-75.55735985899538,39.3415089291669],[-75.56052085963113,39.345074929407886],[-75.5573798594612,39.34910893031886],[-75.54521785550828,39.35077093142699],[-75.54326485443023,39.35324393197732],[-75.53585085285684,39.35062493195349],[-75.52845484986008,39.35831293317277],[-75.5214218479189,39.35861493344312],[-75.51689884719919,39.36099593407035],[-75.51597684702847,39.364370934864475],[-75.51177884619055,39.36603793521713],[-75.4813618376742,39.38756294134767]]]},properties:{geoid:”10003″,name:”New Castle”,state_name:”Delaware”,county_state_name:”New Castle County, Delaware”,”27_22k_diff”:66.19,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.84,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:106.11,”40_65k_diff”:230.44,”60_65k_diff”:1006.71,”27_95k_diff”:0,”40_95k_diff”:17.94,”60_95k_diff”:794.21,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.42,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:566.53,”40_95k_eptc”:672.92,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.19,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.88,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.87,”27_65k_no_eptc”:566.53,”40_65k_no_eptc”:690.86,”60_65k_no_eptc”:1467.13,”27_95k_no_eptc”:566.53,”40_95k_no_eptc”:690.86,”60_95k_no_eptc”:1467.13}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-78.09940567841932,39.722106908972364],[-78.069299670429,39.74830591497055],[-78.06450067022848,39.75770891668782],[-78.05310266664222,39.77030892028969],[-78.04640466524141,39.77930792159498],[-78.02850566094382,39.799907926521286],[-78.01909865915911,39.8071059286432],[-78.00270265475261,39.82660693317648],[-77.98383565082928,39.856505939255904],[-77.9751376489935,39.871795943264566],[-77.96474564863769,39.89963394911465],[-77.96269464755305,39.901733949742365],[-77.95654564644909,39.914831951669946],[-77.95438864687047,39.92321695386647],[-77.95619064723071,39.927031954385946],[-77.95317364627195,39.93164095545583],[-77.94727564442829,39.93494795616531],[-77.93779164315148,39.94895195931223],[-77.93655564327807,39.961131962032034],[-77.93384764313815,39.965422962538355],[-77.93241364246438,39.972400963955366],[-77.92659164104232,39.97919796635425],[-77.92486764140372,39.98433696725599],[-77.91979464088232,39.992659968785595],[-77.92095464121446,40.00045797056888],[-77.91433163942949,40.010310972136054],[-77.9056346376786,40.018733974824094],[-77.90478763746117,40.02278497515412],[-77.89357263441809,40.03334797753178],[-77.88332963260977,40.0485259812765],[-77.87665763155482,40.054668982739486],[-77.86449162771042,40.06157598423458],[-77.92556264980247,40.10398498984122],[-77.92590765006413,40.10191899008091],[-78.0295276830653,40.12274898949381],[-78.07724969910883,40.13304498942695],[-78.07953070012985,40.13389199007019],[-78.13486571928684,40.165138993908776],[-78.15886872365968,40.12190998481261],[-78.18856173116612,40.10172897940367],[-78.20689673656723,40.086272975224524],[-78.20473673519032,40.08535897584733],[-78.20379773511611,40.07880797420771],[-78.205082734714,40.07284797264593],[-78.20273473352813,40.0689059725567],[-78.19074172979171,40.06654397229076],[-78.18530472754207,40.06038597168295],[-78.18153572701385,40.058932971076594],[-78.18395472672103,40.05090696987966],[-78.18789872820761,40.04706196880532],[-78.19931273094471,40.04593596785447],[-78.20415973292702,40.0422109673204],[-78.20568073247978,40.034241965154166],[-78.20270773061416,40.02967296428434],[-78.20368872994338,40.01637896217637],[-78.20101272945858,40.01299596147791],[-78.20433272988579,40.010986961443145],[-78.219813733838,39.99329595704865],[-78.22549973488763,39.98381495523297],[-78.23790173736872,39.957206949256594],[-78.23960473715735,39.95020294810032],[-78.24330173824261,39.94630994644921],[-78.25000373967029,39.93600594490425],[-78.26750474307262,39.903508937100845],[-78.27050274296634,39.89330693582729],[-78.2769037444768,39.8807069324009],[-78.28130574454597,39.86720593020322],[-78.29060474567697,39.843506924721055],[-78.29900574741924,39.82550792129673],[-78.31613075106057,39.80185191607766],[-78.32224475270529,39.79470391378029],[-78.32885175403136,39.78129191110666],[-78.33558375557186,39.77413690975379],[-78.34682075700456,39.75799390573147],[-78.35010675787596,39.75589090502146],[-78.3632237619409,39.74160390154418],[-78.37469976363221,39.72769589844964],[-78.38060176555427,39.722606897428136],[-78.34443775451959,39.72247589863067],[-78.31441674490868,39.72286990058693],[-78.26922073113087,39.722506901991814],[-78.25000272472836,39.72270590247612],[-78.19920570975279,39.72240790481576],[-78.09940567841932,39.722106908972364]]]},properties:{geoid:”42057″,name:”Fulton”,state_name:”Pennsylvania”,county_state_name:”Fulton County, Pennsylvania”,”27_22k_diff”:66.19,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:357.86,”40_65k_diff”:537.44,”60_65k_diff”:1658.67,”27_95k_diff”:145.36,”40_95k_diff”:324.94,”60_95k_diff”:1446.17,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.05,”40_35k_eptc”:86.04,”60_35k_eptc”:86.05,”27_65k_eptc”:460.42,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:672.92,”40_95k_eptc”:672.92,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.19,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.88,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:818.28,”40_65k_no_eptc”:997.86,”60_65k_no_eptc”:2119.09,”27_95k_no_eptc”:818.28,”40_95k_no_eptc”:997.86,”60_95k_no_eptc”:2119.09}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-76.1455212183487,41.99885042295573],[-76.2446702502822,41.99841341904796],[-76.3041032685248,41.99832641666321],[-76.38498429476101,41.998492413572926],[-76.44289531289057,41.9987674113803],[-76.54136334515208,41.999963407691396],[-76.58877436047426,42.000291406263855],[-76.74967741109445,42.00169740002898],[-76.83399943840168,42.00199939681268],[-76.88876045585761,42.00188639405505],[-76.92706146812547,42.001583392652776],[-76.921691464285,41.967520386692996],[-76.91680845944805,41.9342563800028],[-76.90891245253471,41.875252369977446],[-76.90774345129306,41.86380236759786],[-76.90211844687775,41.82492236054189],[-76.89931744461023,41.809336357297624],[-76.8986094440092,41.79447335521799],[-76.88435843069173,41.673130332653024],[-76.88126642812813,41.648418327905645],[-76.87870142514262,41.62035232263616],[-76.87471642231779,41.59692731835535],[-76.81373340230542,41.590042319637504],[-76.79268839522427,41.58782932027869],[-76.60404833487226,41.57250032529948],[-76.50930530392114,41.5647173267682],[-76.41116027204518,41.55677332950957],[-76.38572026386613,41.55499133039685],[-76.35040925179179,41.55202633078213],[-76.27383522727668,41.546081332546265],[-76.22007521020504,41.54128633423914],[-76.20875021016779,41.59176534379714],[-76.19800021007026,41.647831355482865],[-76.16343719860026,41.6492633567604],[-76.11517418356637,41.65183335871219],[-76.11953718897172,41.710438369836226],[-76.12462019518676,41.766923380422135],[-76.12590119614677,41.77062238076665],[-76.1256131961511,41.78032238316419],[-76.13404820571446,41.873596400362196],[-76.13681520855663,41.906742406334565],[-76.1399662113675,41.937011411775124],[-76.1455212183487,41.99885042295573]]]},properties:{geoid:”42015″,name:”Bradford”,state_name:”Pennsylvania”,county_state_name:”Bradford County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.83,”60_35k_diff”:131.84,”27_65k_diff”:110.27,”40_65k_diff”:235.51,”60_65k_diff”:1017.48,”27_95k_diff”:0,”40_95k_diff”:23.01,”60_95k_diff”:804.98,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.41,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:570.68,”40_95k_eptc”:672.92,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:570.68,”40_65k_no_eptc”:695.93,”60_65k_no_eptc”:1477.9,”27_95k_no_eptc”:570.68,”40_95k_no_eptc”:695.93,”60_95k_no_eptc”:1477.9}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-78.11652375307669,40.739135105435736],[-78.13907875910867,40.724283101822756],[-78.15586976388249,40.71775309931048],[-78.15539176415503,40.71449709895862],[-78.16241376526068,40.711704097828274],[-78.17004476836767,40.71260409788151],[-78.18258777211493,40.70590909606137],[-78.19524577537,40.69730209381889],[-78.19986777645026,40.69898009410814],[-78.20487377835155,40.69588209317121],[-78.21714378050994,40.682884090626146],[-78.22197278151593,40.674547088322086],[-78.21369777906946,40.6654120869762],[-78.2061547760642,40.6551360856882],[-78.19835877249135,40.64809808425194],[-78.19608477103013,40.642505083131994],[-78.19722177166639,40.63935908245599],[-78.1902987688787,40.63717608294883],[-78.18917476908324,40.63280008184583],[-78.17872476481948,40.62691708131587],[-78.17342976278614,40.62827308143811],[-78.16973476191338,40.62103308076622],[-78.1663737602815,40.61795608024486],[-78.17167776144392,40.61226507907872],[-78.18421476461782,40.59530307481825],[-78.17929776212351,40.59273307428086],[-78.17828276164289,40.58379407314838],[-78.19708576614333,40.55845206706207],[-78.18914776314863,40.55125106660049],[-78.18559776099255,40.543711064853994],[-78.17830975803871,40.53765706376213],[-78.17682075825331,40.534479063698555],[-78.17174975573332,40.534423063576],[-78.16643575414403,40.53143106363055],[-78.16355575407415,40.53611406446079],[-78.1514817500624,40.540719065935654],[-78.14988674988395,40.546053067188375],[-78.1451427491439,40.549085067882125],[-78.14513774941722,40.55388206871292],[-78.14099174832353,40.5570350690591],[-78.13616474764683,40.569179071745594],[-78.12864074481962,40.56796107227033],[-78.13936674708093,40.55060306857971],[-78.13994974672539,40.54619506738677],[-78.14733074867297,40.53325906433405],[-78.14924274872743,40.52531506313158],[-78.15047874832776,40.510310060152705],[-78.15362874829806,40.496955057279116],[-78.15337574690199,40.488566056078284],[-78.14890074520218,40.4876370552449],[-78.13563574267862,40.498222058439744],[-78.13174374105715,40.49683005824799],[-78.12945073921823,40.4891730562962],[-78.13008373931964,40.481998055085405],[-78.1342357405865,40.47325005333749],[-78.1554497446609,40.43855104617624],[-78.15941274576795,40.43380104505754],[-78.17794974921915,40.40865103904449],[-78.18628475183638,40.39988503690199],[-78.19145675216372,40.39109003502777],[-78.20546275575978,40.37271303155829],[-78.21203775653967,40.35947402792429],[-78.21641075784646,40.353627027422775],[-78.22458075927376,40.34666002543997],[-78.23092676168208,40.339850023432724],[-78.23812676322518,40.33031902187366],[-78.25009376505353,40.312299017253125],[-78.25730776700848,40.29789101437051],[-78.25010576261343,40.2727630104397],[-78.23740375516492,40.22675900185029],[-78.23630475482217,40.22456700163093],[-78.20200074229432,40.20430799910644],[-78.14926172374514,40.17408499463339],[-78.13486571928684,40.165138993908776],[-78.07953070012985,40.13389199007019],[-78.07724969910883,40.13304498942695],[-78.0295276830653,40.12274898949381],[-77.92590765006413,40.10191899008091],[-77.92556264980247,40.10398498984122],[-77.86449162771042,40.06157598423458],[-77.86141162679841,40.062959984449954],[-77.85677462535905,40.06923898600588],[-77.82799561944809,40.116771996956395],[-77.81586861779618,40.132449999951525],[-77.81297561725545,40.139094001176765],[-77.80519861515371,40.152868004858306],[-77.79638861384844,40.16682200722225],[-77.76832760667294,40.204137015850286],[-77.73763459935006,40.23741302391265],[-77.72419959610504,40.25013202649674],[-77.71347859376144,40.25652002833581],[-77.70839159210857,40.261356029385546],[-77.70303259060022,40.263584030526815],[-77.72287260038242,40.31009303858331],[-77.72803560314902,40.3230170402864],[-77.75212261355418,40.378553050380475],[-77.76174261646611,40.3687380482683],[-77.8103956319097,40.368599046522775],[-77.81470063220071,40.36249704531306],[-77.8186386330786,40.360550044170594],[-77.82983963684111,40.3639030443259],[-77.8383456405973,40.36903804556221],[-77.84522364202611,40.36877404459401],[-77.85290864523755,40.36479804402079],[-77.85691664622341,40.365236043778935],[-77.86120564777092,40.36985004480858],[-77.86519764907295,40.37153804499146],[-77.87256065206438,40.3812040458871],[-77.8702916519685,40.39226904848433],[-77.87770365404897,40.39355804865823],[-77.88771965793329,40.391366047127974],[-77.88911865885476,40.398973049417194],[-77.91384666614724,40.398687047724465],[-77.91241866622447,40.40818405024377],[-77.90805266545776,40.414026051116565],[-77.89637166223348,40.417786052769195],[-77.88874866068146,40.42866805456112],[-77.8701846559134,40.44525205826264],[-77.84413964976763,40.473455064871104],[-77.83587664804912,40.48424006775693],[-77.82824764577049,40.491566069226224],[-77.81651564258924,40.50008207178505],[-77.84182965355728,40.550043080330354],[-77.83254765208204,40.562542083050296],[-77.82160264955603,40.5789390867924],[-77.80133164430214,40.59957709139475],[-77.77985563950527,40.61966309628395],[-77.77248263771047,40.62594009738668],[-77.75162263126295,40.632308099915484],[-77.73514462647765,40.64474910220825],[-77.72819562505425,40.64858110359965],[-77.72043662316126,40.65458310527255],[-77.72073962376942,40.65797610587452],[-77.71084862074129,40.66201110717509],[-77.69061661498004,40.67504411018312],[-77.68708261414284,40.67675811091547],[-77.68271061319967,40.68272511199345],[-77.68534861443713,40.68491211200554],[-77.70378961915952,40.679944110603294],[-77.70835862188252,40.69049611259584],[-77.70306862000356,40.692688113482],[-77.69924161947283,40.69807311421041],[-77.70117262026696,40.70499011527374],[-77.67661361376456,40.71646011881961],[-77.68133661652679,40.72976612072839],[-77.71055062461429,40.71457211670486],[-77.71867962783465,40.72738011902877],[-77.76855164283181,40.719474115569824],[-77.82490566159561,40.74354211798665],[-77.85922267214787,40.73082711393192],[-77.89428468248943,40.71621110982708],[-77.90464368536558,40.71074210828425],[-77.94425269584795,40.691565102996535],[-77.99334271235398,40.705215103926655],[-78.01074171792551,40.710371104513094],[-78.11621075307866,40.73938610570411],[-78.11652375307669,40.739135105435736]]]},properties:{geoid:”42061″,name:”Huntingdon”,state_name:”Pennsylvania”,county_state_name:”Huntingdon County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.83,”40_35k_diff”:131.83,”60_35k_diff”:131.83,”27_65k_diff”:99.43,”40_65k_diff”:222.29,”60_65k_diff”:989.41,”27_95k_diff”:0,”40_95k_diff”:9.790000000000077,”60_95k_diff”:776.91,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.41,”40_65k_eptc”:460.42,”60_65k_eptc”:460.41,”27_95k_eptc”:559.84,”40_95k_eptc”:672.92,”60_95k_eptc”:672.91,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.87,”27_65k_no_eptc”:559.84,”40_65k_no_eptc”:682.71,”60_65k_no_eptc”:1449.82,”27_95k_no_eptc”:559.84,”40_95k_no_eptc”:682.71,”60_95k_no_eptc”:1449.82}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-78.38060176555427,39.722606897428136],[-78.37469976363221,39.72769589844964],[-78.3632237619409,39.74160390154418],[-78.35010675787596,39.75589090502146],[-78.34682075700456,39.75799390573147],[-78.33558375557186,39.77413690975379],[-78.32885175403136,39.78129191110666],[-78.32224475270529,39.79470391378029],[-78.31613075106057,39.80185191607766],[-78.29900574741924,39.82550792129673],[-78.29060474567697,39.843506924721055],[-78.28130574454597,39.86720593020322],[-78.2769037444768,39.8807069324009],[-78.27050274296634,39.89330693582729],[-78.26750474307262,39.903508937100845],[-78.25000373967029,39.93600594490425],[-78.24330173824261,39.94630994644921],[-78.23960473715735,39.95020294810032],[-78.23790173736872,39.957206949256594],[-78.22549973488763,39.98381495523297],[-78.219813733838,39.99329595704865],[-78.20433272988579,40.010986961443145],[-78.20101272945858,40.01299596147791],[-78.20368872994338,40.01637896217637],[-78.20270773061416,40.02967296428434],[-78.20568073247978,40.034241965154166],[-78.20415973292702,40.0422109673204],[-78.19931273094471,40.04593596785447],[-78.18789872820761,40.04706196880532],[-78.18395472672103,40.05090696987966],[-78.18153572701385,40.058932971076594],[-78.18530472754207,40.06038597168295],[-78.19074172979171,40.06654397229076],[-78.20273473352813,40.0689059725567],[-78.205082734714,40.07284797264593],[-78.20379773511611,40.07880797420771],[-78.20473673519032,40.08535897584733],[-78.20689673656723,40.086272975224524],[-78.18856173116612,40.10172897940367],[-78.15886872365968,40.12190998481261],[-78.13486571928684,40.165138993908776],[-78.14926172374514,40.17408499463339],[-78.20200074229432,40.20430799910644],[-78.23630475482217,40.22456700163093],[-78.23740375516492,40.22675900185029],[-78.25010576261343,40.2727630104397],[-78.25730776700848,40.29789101437051],[-78.25985676729367,40.29458901406283],[-78.26765276833684,40.27792701013578],[-78.27406276930765,40.26671200770544],[-78.28400877222295,40.254538004804054],[-78.2887667729005,40.24211500279296],[-78.30671277899503,40.24814700318578],[-78.3239247841276,40.25731800410996],[-78.39310280812722,40.2842100064431],[-78.43429082206961,40.30230900836083],[-78.44246482246511,40.27619400303812],[-78.44279682204665,40.25961599963376],[-78.44789782239802,40.244402996218774],[-78.45727482539313,40.25066799702034],[-78.50570284321029,40.287316002850076],[-78.52969885141681,40.29287800250571],[-78.5730738658816,40.30886600389256],[-78.62038588139964,40.3270330055658],[-78.62567488344791,40.31932600381228],[-78.63538788477194,40.30950600110899],[-78.64270988578785,40.28307899575508],[-78.65174588794004,40.281531995440844],[-78.64381888416861,40.25914799117512],[-78.65830788788818,40.24324298753232],[-78.66141288822638,40.231111985560624],[-78.67695889187087,40.21121498099798],[-78.69867389465337,40.16145797025393],[-78.72115389846986,40.11186595948386],[-78.73984990160419,40.069578951083],[-78.75201890461105,40.07492495107886],[-78.76320890689055,40.057012947153254],[-78.76303990465644,40.01472893935994],[-78.76161990372174,40.0144989391608],[-78.75920189635322,39.91094891905726],[-78.75932789545871,39.90690091826365],[-78.75724388972587,39.82349190247021],[-78.76704389054147,39.795391896414074],[-78.77154389178642,39.7891918952561],[-78.79685389589977,39.74116088487316],[-78.80187389715375,39.734567883321596],[-78.80838989796224,39.72291888056413],[-78.72330187232029,39.72303688410442],[-78.70641886728971,39.72289188485283],[-78.62474284192133,39.72295388787479],[-78.57614382609047,39.72256688926502],[-78.54589581718265,39.72284989117211],[-78.53759981392172,39.722479891509195],[-78.49610980167225,39.72287789280259],[-78.44540378607262,39.722837895156246],[-78.4388437842189,39.72248689535775],[-78.4086557740806,39.72280089645804],[-78.38060176555427,39.722606897428136]]]},properties:{geoid:”42009″,name:”Bedford”,state_name:”Pennsylvania”,county_state_name:”Bedford County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.84,”40_35k_diff”:131.83,”60_35k_diff”:131.84,”27_65k_diff”:0,”40_65k_diff”:70.18,”60_65k_diff”:666.38,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:453.88,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:435.11,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:435.11,”40_95k_eptc”:530.6,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.88,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:435.11,”40_65k_no_eptc”:530.6,”60_65k_no_eptc”:1126.8,”27_95k_no_eptc”:435.11,”40_95k_no_eptc”:530.6,”60_95k_no_eptc”:1126.8}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-80.09829739613338,41.07106208385771],[-80.14730641514605,41.11392509011009],[-80.25794844995825,41.11723808537182],[-80.2579364498378,41.128173087720306],[-80.26890545320917,41.12784908693776],[-80.31203546703699,41.12760108537176],[-80.34123647567469,41.12691908363951],[-80.49573952332354,41.125065076574046],[-80.51904053130039,41.1251010751098],[-80.51919552898424,41.105253071994255],[-80.51881852463751,41.041363059985486],[-80.51901952179612,41.01335705482338],[-80.51901151564715,40.921580037197664],[-80.51904750960591,40.85134702412079],[-80.42254248025027,40.85227802832385],[-80.33144545183418,40.85291903287482],[-80.26371043126875,40.85403803569461],[-80.2531264277616,40.85396003614894],[-80.18309540648127,40.85466803981863],[-80.15853339818746,40.85510404053717],[-80.16647541266701,41.00093606771058],[-80.09829739613338,41.07106208385771]]]},properties:{geoid:”42073″,name:”Lawrence”,state_name:”Pennsylvania”,county_state_name:”Lawrence County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.83,”40_35k_diff”:131.83,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:31.55,”60_65k_diff”:584.35,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:371.85,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:403.43,”40_65k_eptc”:460.42,”60_65k_eptc”:460.41,”27_95k_eptc”:403.43,”40_95k_eptc”:491.97,”60_95k_eptc”:672.91,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.87,”27_65k_no_eptc”:403.43,”40_65k_no_eptc”:491.97,”60_65k_no_eptc”:1044.76,”27_95k_no_eptc”:403.43,”40_95k_no_eptc”:491.97,”60_95k_no_eptc”:1044.76}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-74.46493151095558,39.29823795840488],[-74.53908453483008,39.298233955826674],[-74.5429635366055,39.30165495625512],[-74.54751553817549,39.30206595679396],[-74.55861954156042,39.29857495513383],[-74.56876354405676,39.29927595497231],[-74.58369154902432,39.308866956737184],[-74.59176755192969,39.30935095622525],[-74.61800555921631,39.29352995260297],[-74.62460056107105,39.292441951745936],[-74.63278056434393,39.295132952256225],[-74.64340956729355,39.29549995220625],[-74.64917956889394,39.289917950614225],[-74.65817057158824,39.289663950491914],[-74.6593035723217,39.297525951792835],[-74.67560857832605,39.2968319509672],[-74.68018257884391,39.29434395083357],[-74.68656358060498,39.29416295058749],[-74.69039058214564,39.29103094959676],[-74.700182584719,39.29031194853374],[-74.70151058532878,39.293877949546356],[-74.7111275891868,39.29530494922272],[-74.71439958968344,39.29173594905902],[-74.71969659124439,39.29421494883278],[-74.72167259284647,39.298271949666635],[-74.7284395950643,39.29645894948974],[-74.73159059544214,39.29864794918983],[-74.73804359779102,39.298063949621636],[-74.74093059830166,39.295555948367905],[-74.75216660215493,39.2950129485008],[-74.75436960300391,39.299161948513884],[-74.76221960550028,39.29680494824301],[-74.77364260866644,39.300986948298544],[-74.7843756127949,39.307325949506186],[-74.79831361693317,39.30667494918253],[-74.80064561797857,39.308457948642825],[-74.80942862055109,39.306083948388654],[-74.82268962532565,39.30675694827535],[-74.8248846251353,39.305283947487595],[-74.83755663024945,39.31488594867019],[-74.85099863379894,39.31622894852969],[-74.86023563726665,39.31915494949369],[-74.86129563853414,39.32382295004194],[-74.86460963881238,39.32438095041539],[-74.86824463943002,39.318071948779696],[-74.87374364178332,39.312608947118264],[-74.88214764323477,39.30839794583511],[-74.89638564361765,39.23506193077418],[-74.91282464836513,39.22697292872178],[-74.92278665136025,39.22377192808981],[-74.92539265200787,39.21256792537596],[-74.92228465072232,39.20492592369571],[-74.9257286516041,39.20130292304979],[-74.92608765112666,39.19708392238118],[-74.91846064823692,39.19470992223265],[-74.92196464928783,39.19222392173932],[-74.92090864859752,39.18803492098029],[-74.91412464646163,39.18839592114929],[-74.9157706474631,39.184603919826976],[-74.91219364619586,39.17864591904525],[-74.91569064692558,39.17576291780569],[-74.99962167067649,39.135781907534245],[-75.12472170651874,39.07647889107959],[-75.1684637190217,39.056186884986495],[-75.14282870824489,39.01149487665068],[-75.13846270644503,39.002704875121516],[-75.13465470529476,38.99757987415594],[-75.12462870087596,38.97959787119546],[-75.06412167614695,38.87433785187593],[-75.01512465553921,38.788664836459425],[-74.99962265184668,38.80209183938487],[-74.91096962750875,38.87511985744358],[-74.90798762744079,38.87932385854854],[-74.89704762369387,38.88109085909218],[-74.88208261970333,38.884682860189706],[-74.8721596164805,38.88780186106902],[-74.8549226112699,38.88822186225164],[-74.84079960713552,38.890105862342054],[-74.82433060241218,38.89626986469193],[-74.81505359958942,38.90182686570716],[-74.80357259616248,38.91391886871406],[-74.80068059575598,38.92059087053861],[-74.79097759289965,38.92793087205078],[-74.77393958814335,38.94280187556274],[-74.75930758476635,38.94891587787943],[-74.74960958135617,38.954066878568696],[-74.73342457792307,38.96766588182148],[-74.72840357574213,38.97425688369641],[-74.72488457551883,38.9833098860351],[-74.72383157545345,38.98920188676218],[-74.71845657478941,38.997711889150544],[-74.72000957542083,39.00012088929364],[-74.71557257415947,39.00922389156416],[-74.70964657306438,39.01457689275474],[-74.68219456554662,39.04983190105397],[-74.67662256395549,39.052043901457616],[-74.66161655963668,39.0612919035136],[-74.65355955738903,39.06830190509275],[-74.64687555665431,39.07621990739511],[-74.64217055541405,39.08458190945775],[-74.63986955524726,39.094660911512406],[-74.64038555558986,39.10228191316044],[-74.64428055771361,39.11483191548158],[-74.62460355278994,39.14314092164325],[-74.61323655009093,39.15270092407565],[-74.60360354791817,39.16295292663947],[-74.5953475457358,39.1777599297636],[-74.58984254458066,39.18345493066451],[-74.58373654245175,39.187227932037246],[-74.57487754050341,39.19925893462087],[-74.56524253815876,39.210649937586425],[-74.55561053581425,39.21976293981832],[-74.54597753273231,39.22659794147145],[-74.5239595265863,39.24026794521061],[-74.51845552582834,39.24596294638996],[-74.50847252309083,39.26097894932235],[-74.49106751851508,39.274075952910835],[-74.48970051780205,39.27730895367351],[-74.47731551509568,39.288699956132156],[-74.46493151095558,39.29823795840488]]]},properties:{geoid:”34009″,name:”Cape May”,state_name:”New Jersey”,county_state_name:”Cape May County, New Jersey”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:84.32,”60_65k_diff”:696.41,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:483.91,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.05,”27_65k_eptc”:446.7,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:446.7,”40_95k_eptc”:544.74,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:446.7,”40_65k_no_eptc”:544.74,”60_65k_no_eptc”:1156.83,”27_95k_no_eptc”:446.7,”40_95k_no_eptc”:544.74,”60_95k_no_eptc”:1156.83}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-77.14411346978856,41.06884820776083],[-77.16428047640328,41.06871620705769],[-77.24969350984061,41.15091521928457],[-77.26223351476628,41.162417220393564],[-77.27202051801741,41.17254222223234],[-77.27245251844118,41.17545122245084],[-77.27741352029294,41.180547223178486],[-77.28830852437802,41.18299822323704],[-77.29306152569299,41.18648122418463],[-77.29365352670513,41.19107722511361],[-77.29058252503343,41.19510822556793],[-77.29901252819286,41.20097522666273],[-77.30636653105809,41.208085227767086],[-77.32089353673209,41.21894022898158],[-77.33430554142437,41.22048422884996],[-77.34976754541363,41.21992622824442],[-77.34962954607792,41.22888122962504],[-77.35804954913299,41.23060522944808],[-77.36273155148066,41.23358823066441],[-77.37035255313147,41.23308722975754],[-77.39082656064512,41.247794231745864],[-77.3990455643052,41.25306123278122],[-77.40440956539945,41.258178233566625],[-77.41066956833558,41.26622923484306],[-77.41612756987854,41.27006423498256],[-77.4249475731555,41.27311123560773],[-77.42940257607168,41.282148236751645],[-77.44516058109713,41.28777023706221],[-77.45005658343754,41.293270237707496],[-77.45642658585328,41.30464723955282],[-77.46824758944312,41.31043724023645],[-77.4718645913088,41.31428124082815],[-77.4750315933356,41.32669724343197],[-77.47453559303598,41.33402924499086],[-77.47598959471219,41.33830224552277],[-77.48556959778793,41.34528924641573],[-77.49919560248858,41.35358524705578],[-77.51614760857036,41.35587524718603],[-77.52653961150871,41.35853624699193],[-77.53744061611324,41.364811248172636],[-77.54001061722046,41.36810924896225],[-77.54190161862716,41.381304251091954],[-77.55045162190638,41.395834252928175],[-77.56443762700724,41.412691255911284],[-77.57093263009476,41.415246255910574],[-77.57574263144346,41.42161025754231],[-77.58054263411294,41.4355872598328],[-77.58467363639429,41.441309260256695],[-77.59728463979886,41.441064260125614],[-77.59813164284154,41.478584267040894],[-77.73366668585096,41.47759326135811],[-77.77232969764806,41.47752925953763],[-77.82829171508357,41.47699025719084],[-77.861294726608,41.476207255665685],[-77.95213975522569,41.475613251894465],[-77.98919676600318,41.47483024981132],[-77.98846475934405,41.388507234279516],[-77.98878875842213,41.367461230104055],[-78.01326676296522,41.33103022195826],[-78.09338378033888,41.21693919696318],[-78.06100976701974,41.17454719044932],[-78.03817375791068,41.15361118726554],[-78.0349717574879,41.15392818736777],[-78.02859675531214,41.15033318691524],[-78.01735075198123,41.15319518858855],[-78.01447875039852,41.15200418788571],[-78.01202374932667,41.14507918687449],[-78.00910774785063,41.14332418638517],[-78.00357174640801,41.144864187414704],[-78.00033174634943,41.150958188497526],[-78.00179874724282,41.158141189626974],[-77.99791074660536,41.16337719088707],[-77.99027474399576,41.16171219133532],[-77.98671374252176,41.16380719170706],[-77.98418974305874,41.170244193159675],[-77.97301473917783,41.17302919365706],[-77.970835738479,41.17832219518141],[-77.97359074036278,41.18910119698582],[-77.97308074196793,41.204196199625464],[-77.96565273911182,41.20959220073573],[-77.95944073873329,41.21750520318219],[-77.95561773716706,41.21743520327474],[-77.95060873540105,41.213799202349676],[-77.94083573165746,41.209444201828255],[-77.93565873028422,41.21174920238878],[-77.93561773050477,41.21489920353034],[-77.93901073170079,41.22271520431608],[-77.9362637310915,41.226006205574244],[-77.92363372698925,41.226435205916474],[-77.92016972640222,41.229247206987736],[-77.9137897257285,41.24057320898228],[-77.89826472161619,41.252673212411246],[-77.89766971523474,41.17692619759371],[-77.79001168225135,41.177150201723755],[-77.78956567900762,41.14213519585456],[-77.77799867601325,41.14662019675145],[-77.74667766293173,41.106269190052394],[-77.73698866059884,41.10791419153098],[-77.73023965788235,41.11137619173249],[-77.72478665590998,41.10740119197107],[-77.7177616540986,41.1049621911566],[-77.7139436521951,41.10598319163378],[-77.7122686520328,41.1103541923635],[-77.70622765055117,41.11388019321437],[-77.69549264683319,41.10760819302981],[-77.69039164557795,41.10625719248045],[-77.68375364405394,41.10931419365094],[-77.67272463925927,41.10520819309569],[-77.66709463868197,41.108289193927384],[-77.66081463563386,41.1067661938964],[-77.6589726346975,41.10096319307401],[-77.65006963179478,41.09756119274326],[-77.64766863140379,41.098088193175066],[-77.62176162314695,41.09119319220884],[-77.62095062183742,41.08909519211474],[-77.61203261881728,41.08581719238576],[-77.59526461376832,41.07771919160285],[-77.59200361155033,41.07163518979877],[-77.58382360928177,41.070105189943654],[-77.58143060857985,41.0671231900238],[-77.57356760546625,41.06869019071825],[-77.56761460376039,41.06538518972202],[-77.56173860180414,41.057650188498364],[-77.58019660640514,41.047278185666514],[-77.55909659795796,41.02182618160649],[-77.50859857781533,40.962946172884315],[-77.44027655692517,40.97445617732955],[-77.39390954256415,40.978293180183584],[-77.33992752679038,40.98717518424204],[-77.22888949399498,41.019656194629285],[-77.14416246804348,41.04434620276905],[-77.14411346978856,41.06884820776083]]]},properties:{geoid:”42035″,name:”Clinton”,state_name:”Pennsylvania”,county_state_name:”Clinton County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.83,”40_35k_diff”:131.83,”60_35k_diff”:131.83,”27_65k_diff”:52.73,”40_65k_diff”:165.35,”60_65k_diff”:868.49,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:655.99,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.42,”40_65k_eptc”:460.42,”60_65k_eptc”:460.41,”27_95k_eptc”:513.15,”40_95k_eptc”:625.77,”60_95k_eptc”:672.91,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.87,”27_65k_no_eptc”:513.15,”40_65k_no_eptc”:625.77,”60_65k_no_eptc”:1328.9,”27_95k_no_eptc”:513.15,”40_95k_no_eptc”:625.77,”60_95k_no_eptc”:1328.9}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-76.38033620909066,40.775453181514436],[-76.3071721872361,40.80181718902182],[-76.2846131852675,40.883596206176755],[-76.24966317618218,40.91580021329897],[-76.20782916556635,40.94974822149622],[-76.22077117264107,41.00009323111791],[-76.23119617963329,41.05017624016913],[-76.22848017912406,41.05364024063229],[-76.228977185554,41.138474256977915],[-76.24977219121303,41.135070255169516],[-76.2776411996569,41.1318122536554],[-76.2999852103953,41.17172726037657],[-76.31923821846736,41.20810026700551],[-76.31995921863381,41.21126326714852],[-76.31859021988912,41.23548027237433],[-76.31291522202682,41.287829282580745],[-76.31026322300154,41.31020628677205],[-76.3743702433024,41.308684283452706],[-76.40793625292692,41.30842628259323],[-76.4475992640472,41.27563727426822],[-76.47881327236514,41.25009126824722],[-76.49965427776195,41.2338642647722],[-76.52165428353335,41.2142682599492],[-76.59260930208491,41.15777324654787],[-76.64076931749435,41.155726244270156],[-76.63089431189177,41.12521623837692],[-76.62085130622717,41.08996523243319],[-76.6204603054159,41.08484823114674],[-76.61549730360372,41.07971623088164],[-76.61736530411548,41.07336122949769],[-76.61604130347395,41.06875622890199],[-76.61897330330692,41.06376722759166],[-76.56991728725457,41.05376922734691],[-76.56226528314158,41.034222224084616],[-76.56284928327521,41.02345522195543],[-76.56621028275057,41.00859521925969],[-76.5652352818639,40.99982021688857],[-76.52734426801716,40.97152021289504],[-76.51456326287244,40.95675921052018],[-76.51587026378853,40.95026321009967],[-76.51242326151181,40.946110208608836],[-76.52939726693712,40.94015120681971],[-76.52582626525947,40.93457520584329],[-76.52178226441558,40.93166120581914],[-76.52014026283967,40.92664220474039],[-76.52224226302981,40.92275120396785],[-76.52833126460129,40.91848020335158],[-76.52486426379129,40.915944203067745],[-76.52802626290298,40.88262119591356],[-76.50662725607954,40.88286719709118],[-76.5037892547041,40.87873419630809],[-76.50933225577474,40.87398519547381],[-76.50775425526719,40.864057193259946],[-76.50248325311222,40.86177719301688],[-76.49800825164083,40.854083191594796],[-76.49925325181347,40.85034419139276],[-76.50809525400881,40.84664519041294],[-76.50805625393922,40.84213918876617],[-76.5025702510161,40.831708187079876],[-76.50128725035073,40.82465818598612],[-76.49524724811046,40.82419118596754],[-76.48723824583722,40.826332187065724],[-76.4639082385368,40.82831118797511],[-76.4578822374579,40.830169188835725],[-76.42993122835608,40.83222619030517],[-76.42334922634299,40.833407190980004],[-76.41148922270462,40.833498191134396],[-76.39405121412679,40.80125518523889],[-76.39264721419298,40.79736718477954],[-76.38033620909066,40.775453181514436]]]},properties:{geoid:”42037″,name:”Columbia”,state_name:”Pennsylvania”,county_state_name:”Columbia County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.84,”27_65k_diff”:188.06,”40_65k_diff”:330.38,”60_65k_diff”:1218.95,”27_95k_diff”:0,”40_95k_diff”:117.88,”60_95k_diff”:1006.45,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.42,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:648.48,”40_95k_eptc”:672.92,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:648.48,”40_65k_no_eptc”:790.8,”60_65k_no_eptc”:1679.37,”27_95k_no_eptc”:648.48,”40_95k_no_eptc”:790.8,”60_95k_no_eptc”:1679.37}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-75.6967839577076,40.241871102616024],[-75.62489494055846,40.32978112305517],[-75.60028993402975,40.360173129461955],[-75.58783893106536,40.375062133343455],[-75.54271092043132,40.43061514547811],[-75.52969591821261,40.447003149286964],[-75.57950493539643,40.4780651534092],[-75.6685719668022,40.534953161649014],[-75.73803999230869,40.57911316737137],[-75.77892300697553,40.60447017080586],[-75.82560602363503,40.633871174510865],[-75.8495150325553,40.649948176986456],[-75.89147504709355,40.67727818058984],[-75.99321407717015,40.63972016967554],[-76.01222807952988,40.57772115692278],[-76.02120308177126,40.5737631559862],[-76.02651108396051,40.57860315647881],[-76.03153708506902,40.577004156306174],[-76.03669408741952,40.579336155919464],[-76.0395110880554,40.58310215728084],[-76.04725309019311,40.58268415631099],[-76.05094409163183,40.57517615506656],[-76.05423009206,40.5740941545254],[-76.05802609333352,40.579637155199016],[-76.06534109621522,40.57968615512027],[-76.07944210012764,40.56610615187823],[-76.10586710765882,40.56220615015159],[-76.13474711576856,40.553490147367675],[-76.13760611734503,40.551137147230584],[-76.15509812223128,40.5452371451566],[-76.16013912307051,40.54045814405255],[-76.16360112403406,40.53999714362712],[-76.17162612645879,40.53495514237057],[-76.18564013130977,40.53556314216286],[-76.19663613395102,40.531273140427004],[-76.21940914155554,40.528707139052614],[-76.23112514455912,40.524224138400115],[-76.23432314590202,40.52208213797702],[-76.25601015205994,40.51707513599124],[-76.27215415769045,40.51759413516942],[-76.28211116099835,40.5161451346613],[-76.30232816619679,40.51466613355382],[-76.31458117100752,40.515918133651475],[-76.32254617356006,40.51416813233386],[-76.33043717578532,40.51591813266015],[-76.33911117894579,40.51535913270621],[-76.35240218291088,40.51116513069273],[-76.36922418785846,40.50960513033907],[-76.3781591901259,40.50602012884466],[-76.38435019226418,40.50574712879574],[-76.40587619900293,40.49873712642401],[-76.41860220278872,40.495623125489296],[-76.44018320867728,40.49596012434046],[-76.35225617775289,40.441467117560705],[-76.32843916905017,40.42682811504948],[-76.24967514153367,40.37722910859278],[-76.23191813527953,40.36630010771689],[-76.20553012607792,40.360669107662574],[-76.15788510867286,40.32095710082173],[-76.15121710576648,40.31597910027737],[-76.14951110526172,40.31446210009639],[-76.06986507667553,40.26390009369221],[-76.04976407040908,40.25080009112711],[-76.00726805486937,40.223831087708426],[-75.98885304791781,40.21164208619209],[-75.95476903616287,40.190150083461425],[-75.8751640078349,40.13807907580123],[-75.87337700684066,40.13711507552625],[-75.8546130021137,40.14926907931486],[-75.84651799951325,40.153806080524966],[-75.82098199284783,40.16972408396817],[-75.74317997133569,40.21672909626344],[-75.72986496743619,40.224497098742056],[-75.6967839577076,40.241871102616024]]]},properties:{geoid:”42011″,name:”Berks”,state_name:”Pennsylvania”,county_state_name:”Berks County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.83,”40_35k_diff”:131.83,”60_35k_diff”:131.84,”27_65k_diff”:26.17,”40_65k_diff”:132.95,”60_65k_diff”:799.68,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:587.18,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.41,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:486.58,”40_95k_eptc”:593.37,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:486.58,”40_65k_no_eptc”:593.37,”60_65k_no_eptc”:1260.1,”27_95k_no_eptc”:486.58,”40_95k_no_eptc”:593.37,”60_95k_no_eptc”:1260.1}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-79.99978239854833,41.490057166333074],[-80.0325894088924,41.48890016448023],[-80.1255994370094,41.48628616023926],[-80.12537243619815,41.480404159065074],[-80.1567694462861,41.48089015779467],[-80.16947545063807,41.48153915729134],[-80.22439446784884,41.482499154676724],[-80.25718647735908,41.48342615336025],[-80.27559848362603,41.483490152976565],[-80.35072550687867,41.48472014959502],[-80.37885451642319,41.48583814893351],[-80.43115053229079,41.486966146146095],[-80.43209253328938,41.49209714766114],[-80.44489953701452,41.4922771470014],[-80.44500453637795,41.48712614588713],[-80.5192195603435,41.489119143035026],[-80.5189955526338,41.40435112761112],[-80.51911854994201,41.36087711890523],[-80.51910254226463,41.267220101919605],[-80.51895553614854,41.18854608730046],[-80.51922353427146,41.16094408161992],[-80.51904053130039,41.1251010751098],[-80.49573952332354,41.125065076574046],[-80.34123647567469,41.12691908363951],[-80.31203546703699,41.12760108537176],[-80.26890545320917,41.12784908693776],[-80.2579364498378,41.128173087720306],[-80.25794844995825,41.11723808537182],[-80.14730641514605,41.11392509011009],[-80.09829739613338,41.07106208385771],[-80.09686439529027,41.069812083872456],[-80.04706738403006,41.1206480953041],[-79.99978237287708,41.17186910683948],[-79.99920737529692,41.19710011194699],[-79.99978237645965,41.211837114302895],[-79.999780387018,41.34144813875591],[-79.99978239854833,41.490057166333074]]]},properties:{geoid:”42085″,name:”Mercer”,state_name:”Pennsylvania”,county_state_name:”Mercer County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.83,”40_35k_diff”:131.83,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:31.55,”60_65k_diff”:584.35,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:371.85,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:403.43,”40_65k_eptc”:460.42,”60_65k_eptc”:460.41,”27_95k_eptc”:403.43,”40_95k_eptc”:491.97,”60_95k_eptc”:672.91,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.87,”27_65k_no_eptc”:403.43,”40_65k_no_eptc”:491.97,”60_65k_no_eptc”:1044.76,”27_95k_no_eptc”:403.43,”40_95k_no_eptc”:491.97,”60_95k_no_eptc”:1044.76}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-74.46329258721104,40.599195217536355],[-74.47385959111789,40.59701621697514],[-74.48321959380227,40.5894412157503],[-74.49050059525594,40.58653421482725],[-74.50479459969456,40.586300213743755],[-74.51514760316778,40.58011821215553],[-74.52580560585064,40.56854920932885],[-74.52449360536859,40.561730208215806],[-74.52668660593052,40.55948220780804],[-74.52077360327705,40.55653620744896],[-74.5177926024325,40.55285820700314],[-74.5161446012846,40.545823205803764],[-74.51185459915877,40.53988820500149],[-74.49486359349068,40.528744203439345],[-74.48511658932976,40.51532520101447],[-74.48190358879121,40.512009200109446],[-74.46694858332496,40.50890620026073],[-74.46695358251117,40.502879198695936],[-74.45918058077837,40.496627197672986],[-74.4598645800126,40.49105419728154],[-74.46821058254174,40.486853195655584],[-74.47850058547242,40.483926195172224],[-74.48493858794997,40.47959919368629],[-74.49564159061063,40.468710191080945],[-74.50781559369666,40.460993189674035],[-74.52033959729114,40.451286186850496],[-74.52664859839821,40.44477518528026],[-74.5362496010755,40.43830818386931],[-74.55454760602055,40.430168181731254],[-74.57616561352799,40.42231217944389],[-74.5858656155255,40.41709317777247],[-74.58581561454,40.40228017490524],[-74.58771061470948,40.3944261736247],[-74.59184461583997,40.39203517266347],[-74.59530661632009,40.3863951714693],[-74.60256861852264,40.3807281697137],[-74.6129796221733,40.3757681688747],[-74.62024162405832,40.37375716810516],[-74.62521762541195,40.36312916573454],[-74.62582862445404,40.35640416478318],[-74.63059762504047,40.339613161084635],[-74.62327562242803,40.334433160497134],[-74.62438262309018,40.329328158879484],[-74.62265262177075,40.32532215860921],[-74.61404261958734,40.32459815891694],[-74.6033236150457,40.32141015843454],[-74.60025961368504,40.315469157477466],[-74.59505161304139,40.31585915757581],[-74.58558860989045,40.31325015754974],[-74.58407060907251,40.308193156723064],[-74.57952260701995,40.30382115593071],[-74.56087760046438,40.29601815451986],[-74.55669959825482,40.291664154073395],[-74.54215959391915,40.29168915501512],[-74.53658359206374,40.289494154536136],[-74.52939459052133,40.29425515559322],[-74.52157658722764,40.290042154745336],[-74.51976258731437,40.287070154159395],[-74.51485658544321,40.287146154567665],[-74.50881158268841,40.281891153571536],[-74.50162758058933,40.27951615365521],[-74.49761857980387,40.28054215360073],[-74.48192857401183,40.2738301532803],[-74.48496357336015,40.25333314887041],[-74.46430256648924,40.25225314950386],[-74.46077756620947,40.25136614970524],[-74.39343954603507,40.279556157266235],[-74.39423254693732,40.28839815915692],[-74.37754654301254,40.30544016351898],[-74.31945052682144,40.35083317422997],[-74.25954751010073,40.39734218573611],[-74.24789550697571,40.406613187731146],[-74.24779850881744,40.43120519230227],[-74.23640850617619,40.44345319545843],[-74.23083150402667,40.44572919641955],[-74.22708450333957,40.44452519596365],[-74.2227385014073,40.45106019773331],[-74.22819750591599,40.477629202336495],[-74.25303751413848,40.48666820298165],[-74.25884451691005,40.49888320555706],[-74.25813051618616,40.508725207640424],[-74.25409651592102,40.51566920939012],[-74.24602151348074,40.520966210606666],[-74.25028551665056,40.54230821448235],[-74.24748551596205,40.549385215664536],[-74.23141651139963,40.55919021866523],[-74.2180045073244,40.557066218650434],[-74.21457650550856,40.56054121943776],[-74.21014550511421,40.57373222211544],[-74.20724350539611,40.58792322448013],[-74.2032925046407,40.593050225545646],[-74.21150550741156,40.598329226786845],[-74.21247250760375,40.60282922776658],[-74.22974651357094,40.598834225777495],[-74.2353795154607,40.60247522684815],[-74.24166751701013,40.599564225792726],[-74.25296952060683,40.60077622574633],[-74.25769052269196,40.60228422599155],[-74.25956052216348,40.59732122479093],[-74.29099153223036,40.59193322290863],[-74.29994953570335,40.59812822360806],[-74.30532753751875,40.600594223446514],[-74.30292253761078,40.6086912257206],[-74.45690558498798,40.59580821708324],[-74.46329258721104,40.599195217536355]]]},properties:{geoid:”34023″,name:”Middlesex”,state_name:”New Jersey”,county_state_name:”Middlesex County, New Jersey”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:84.32,”60_65k_diff”:696.41,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:483.91,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.05,”27_65k_eptc”:446.7,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:446.7,”40_95k_eptc”:544.74,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:446.7,”40_65k_no_eptc”:544.74,”60_65k_no_eptc”:1156.83,”27_95k_no_eptc”:446.7,”40_95k_no_eptc”:544.74,”60_95k_no_eptc”:1156.83}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-76.44018320867728,40.49596012434046],[-76.41860220278872,40.495623125489296],[-76.40587619900293,40.49873712642401],[-76.38435019226418,40.50574712879574],[-76.3781591901259,40.50602012884466],[-76.36922418785846,40.50960513033907],[-76.35240218291088,40.51116513069273],[-76.33911117894579,40.51535913270621],[-76.33043717578532,40.51591813266015],[-76.32254617356006,40.51416813233386],[-76.31458117100752,40.515918133651475],[-76.30232816619679,40.51466613355382],[-76.28211116099835,40.5161451346613],[-76.27215415769045,40.51759413516942],[-76.25601015205994,40.51707513599124],[-76.23432314590202,40.52208213797702],[-76.23112514455912,40.524224138400115],[-76.21940914155554,40.528707139052614],[-76.19663613395102,40.531273140427004],[-76.18564013130977,40.53556314216286],[-76.17162612645879,40.53495514237057],[-76.16360112403406,40.53999714362712],[-76.16013912307051,40.54045814405255],[-76.15509812223128,40.5452371451566],[-76.13760611734503,40.551137147230584],[-76.13474711576856,40.553490147367675],[-76.10586710765882,40.56220615015159],[-76.07944210012764,40.56610615187823],[-76.06534109621522,40.57968615512027],[-76.05802609333352,40.579637155199016],[-76.05423009206,40.5740941545254],[-76.05094409163183,40.57517615506656],[-76.04725309019311,40.58268415631099],[-76.0395110880554,40.58310215728084],[-76.03669408741952,40.579336155919464],[-76.03153708506902,40.577004156306174],[-76.02651108396051,40.57860315647881],[-76.02120308177126,40.5737631559862],[-76.01222807952988,40.57772115692278],[-75.99321407717015,40.63972016967554],[-75.89147504709355,40.67727818058984],[-75.85481103609285,40.69320018501357],[-75.84466503310092,40.69300918580603],[-75.80779102244514,40.70750019021248],[-75.79652001949559,40.71704219178452],[-75.77968401483109,40.72503019425823],[-75.77769201420824,40.72954219564952],[-75.76594901077985,40.730934196207265],[-75.75780900892455,40.735422197089406],[-75.78156701689963,40.75010119935488],[-75.82210703209708,40.77612920269758],[-75.82891003455461,40.780118202811394],[-75.87084104925418,40.806956206892075],[-75.88603905467338,40.81627520830219],[-75.90836206318228,40.8355832110872],[-75.92737707053477,40.85255821377387],[-75.95534508006574,40.87648621684498],[-75.9976380967849,40.913267222141855],[-76.02800810569146,40.90232121959711],[-76.10970813322771,40.923653220056394],[-76.20782916556635,40.94974822149622],[-76.24966317618218,40.91580021329897],[-76.2846131852675,40.883596206176755],[-76.3071721872361,40.80181718902182],[-76.38033620909066,40.775453181514436],[-76.39660421334415,40.76983817938741],[-76.50520124557583,40.73016116756145],[-76.5444932565472,40.71546116363626],[-76.572397264254,40.705400160679545],[-76.60007027312274,40.69707215797859],[-76.63755928404827,40.68287115351087],[-76.66213929091577,40.6740211504438],[-76.69517530037835,40.662955147294404],[-76.70074030205478,40.662822147005656],[-76.70162630200974,40.65809014635093],[-76.66882529015679,40.63760714298005],[-76.64143528138806,40.6209301411894],[-76.58448226107602,40.58511813672627],[-76.53541624302886,40.555165132401825],[-76.49968623026912,40.532610129397874],[-76.44018320867728,40.49596012434046]]]},properties:{geoid:”42107″,name:”Schuylkill”,state_name:”Pennsylvania”,county_state_name:”Schuylkill County, Pennsylvania”,”27_22k_diff”:66.19,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.84,”40_35k_diff”:131.83,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:83.74,”60_65k_diff”:695.18,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:482.68,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:446.23,”40_65k_eptc”:460.42,”60_65k_eptc”:460.41,”27_95k_eptc”:446.23,”40_95k_eptc”:544.16,”60_95k_eptc”:672.91,”27_22k_no_eptc”:66.19,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.88,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.87,”27_65k_no_eptc”:446.23,”40_65k_no_eptc”:544.16,”60_65k_no_eptc”:1155.59,”27_95k_no_eptc”:446.23,”40_95k_no_eptc”:544.16,”60_95k_no_eptc”:1155.59}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-75.72279888061315,38.829858819474985],[-75.71303386961554,38.70650679501247],[-75.70550986211934,38.610804775800986],[-75.69367184952551,38.46008774500148],[-75.60187282108372,38.45676874714749],[-75.50939979203928,38.454291750634084],[-75.39371375567467,38.45213175420898],[-75.37391874903028,38.452265754960926],[-75.23211670555676,38.45122975913579],[-75.13954667583975,38.45118176270574],[-75.04874064707366,38.45127276550052],[-74.99962663194634,38.45113976732779],[-74.98628362821913,38.451639768272614],[-74.98618562890726,38.46630877102728],[-74.98512962856572,38.4738587724899],[-74.98420162928736,38.497101776857974],[-74.98517263157996,38.528178783277006],[-74.98884363454883,38.56095379002756],[-74.98967063605556,38.57737479349324],[-74.9923046380102,38.595851797287224],[-74.9935206392559,38.612508801041855],[-74.99726964160394,38.625118803237655],[-75.00196964260181,38.631690804539765],[-75.00192164437975,38.64973680796972],[-75.00274664485069,38.66624281175713],[-75.002137645648,38.67591781360844],[-75.00302664654552,38.68597181516008],[-75.00899565020808,38.711980820609554],[-75.00986264989383,38.719915822264376],[-75.01421365308045,38.74504382724698],[-75.01326965318496,38.75615482953743],[-75.01339065469712,38.77235483307987],[-75.01736765621699,38.786646835657734],[-75.01512465553921,38.788664836459425],[-75.06412167614695,38.87433785187593],[-75.12462870087596,38.97959787119546],[-75.13465470529476,38.99757987415594],[-75.13846270644503,39.002704875121516],[-75.31207975876005,38.94587285755729],[-75.31353575836603,38.950437858840445],[-75.321267761981,38.95346285883837],[-75.3246367622067,38.94971785763554],[-75.33244576461773,38.95071485819224],[-75.33679876645495,38.94654285675197],[-75.34351776868573,38.947446857338115],[-75.34217576845253,38.951442858140226],[-75.34406276866355,38.95527685883006],[-75.35277577124413,38.94793285687166],[-75.36102677388863,38.957540858166794],[-75.36620977618006,38.953942857187755],[-75.36788777658701,38.95958785834385],[-75.37213277775575,38.96144385866856],[-75.38134078085913,38.96129285877735],[-75.38252678096306,38.95591385744306],[-75.39361678398329,38.952853856027495],[-75.40104178572834,38.94703885497979],[-75.39850478543559,38.94080185323795],[-75.40287478632263,38.937457852995266],[-75.3986147848385,38.933524852336426],[-75.40095178479463,38.92948885091475],[-75.39911078397975,38.92691785109655],[-75.40839578686308,38.92008684865333],[-75.40881978691732,38.916831848568634],[-75.41670178969044,38.918025848195164],[-75.4246937915065,38.91342584744845],[-75.42979479291361,38.91358984743335],[-75.43470979425246,38.91089984641244],[-75.44418879805923,38.91307584630112],[-75.45684380176752,38.909719845362176],[-75.46534480406915,38.911272845551046],[-75.47722380803515,38.90584884411471],[-75.4858348106516,38.903560842603056],[-75.48815781111084,38.898990841806835],[-75.48802781076661,38.89279184082606],[-75.49438481190877,38.887889839706105],[-75.49688981266267,38.88300883796701],[-75.50816981545758,38.878958836849826],[-75.50974681668359,38.87500483668676],[-75.5204408188665,38.85574983245253],[-75.53623582357514,38.84989782986332],[-75.53958182352586,38.843641829034226],[-75.54872782653419,38.841084828421046],[-75.55501482835044,38.835656826830615],[-75.58488583752033,38.834560825373295],[-75.68317586752445,38.83132382112899],[-75.72279888061315,38.829858819474985]]]},properties:{geoid:”10005″,name:”Sussex”,state_name:”Delaware”,county_state_name:”Sussex County, Delaware”,”27_22k_diff”:66.19,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.84,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:106.11,”40_65k_diff”:230.44,”60_65k_diff”:1006.71,”27_95k_diff”:0,”40_95k_diff”:17.94,”60_95k_diff”:794.21,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.42,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:566.53,”40_95k_eptc”:672.92,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.19,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.88,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.87,”27_65k_no_eptc”:566.53,”40_65k_no_eptc”:690.86,”60_65k_no_eptc”:1467.13,”27_95k_no_eptc”:566.53,”40_95k_no_eptc”:690.86,”60_95k_no_eptc”:1467.13}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-76.22007521020504,41.54128633423914],[-76.27383522727668,41.546081332546265],[-76.35040925179179,41.55202633078213],[-76.38572026386613,41.55499133039685],[-76.41116027204518,41.55677332950957],[-76.50930530392114,41.5647173267682],[-76.60404833487226,41.57250032529948],[-76.79268839522427,41.58782932027869],[-76.81373340230542,41.590042319637504],[-76.80461739760078,41.564541315569656],[-76.79755439404285,41.54299731144566],[-76.78279938644361,41.502631304875095],[-76.76785637842165,41.45820929692207],[-76.74949936886024,41.40558028748115],[-76.7451703675353,41.40236228678522],[-76.70730835378552,41.378790284433244],[-76.66129933678985,41.34957328076333],[-76.59253431193862,41.304340274462724],[-76.54782329761997,41.29573027480946],[-76.54849029678165,41.29314327430875],[-76.52027828816362,41.28823327396674],[-76.49969128120773,41.28548727457606],[-76.4475992640472,41.27563727426822],[-76.40793625292692,41.30842628259323],[-76.3743702433024,41.308684283452706],[-76.31026322300154,41.31020628677205],[-76.28280121799624,41.37725230034644],[-76.27678621776558,41.39157630359638],[-76.22813321055723,41.511145327804925],[-76.22386821027341,41.524552330742516],[-76.22007521020504,41.54128633423914]]]},properties:{geoid:”42113″,name:”Sullivan”,state_name:”Pennsylvania”,county_state_name:”Sullivan County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.83,”60_35k_diff”:131.84,”27_65k_diff”:110.27,”40_65k_diff”:235.51,”60_65k_diff”:1017.48,”27_95k_diff”:0,”40_95k_diff”:23.01,”60_95k_diff”:804.98,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.41,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:570.68,”40_95k_eptc”:672.92,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:570.68,”40_65k_no_eptc”:695.93,”60_65k_no_eptc”:1477.9,”27_95k_no_eptc”:570.68,”40_95k_no_eptc”:695.93,”60_95k_no_eptc”:1477.9}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-76.70162630200974,40.65809014635093],[-76.70074030205478,40.662822147005656],[-76.69517530037835,40.662955147294404],[-76.66213929091577,40.6740211504438],[-76.63755928404827,40.68287115351087],[-76.60007027312274,40.69707215797859],[-76.572397264254,40.705400160679545],[-76.5444932565472,40.71546116363626],[-76.50520124557583,40.73016116756145],[-76.39660421334415,40.76983817938741],[-76.38033620909066,40.775453181514436],[-76.39264721419298,40.79736718477954],[-76.39405121412679,40.80125518523889],[-76.41148922270462,40.833498191134396],[-76.42334922634299,40.833407190980004],[-76.42993122835608,40.83222619030517],[-76.4578822374579,40.830169188835725],[-76.4639082385368,40.82831118797511],[-76.48723824583722,40.826332187065724],[-76.49524724811046,40.82419118596754],[-76.50128725035073,40.82465818598612],[-76.5025702510161,40.831708187079876],[-76.50805625393922,40.84213918876617],[-76.50809525400881,40.84664519041294],[-76.49925325181347,40.85034419139276],[-76.49800825164083,40.854083191594796],[-76.50248325311222,40.86177719301688],[-76.50775425526719,40.864057193259946],[-76.50933225577474,40.87398519547381],[-76.5037892547041,40.87873419630809],[-76.50662725607954,40.88286719709118],[-76.52802626290298,40.88262119591356],[-76.55079127029427,40.88258519504377],[-76.55738027177676,40.88890219647061],[-76.56029627366902,40.898869198368075],[-76.56479727626616,40.90424119853547],[-76.5681132775164,40.91546220063138],[-76.56557427725276,40.92115420231889],[-76.56167227591044,40.92478620263513],[-76.55857227508714,40.9305042043759],[-76.55697927600922,40.93861720581737],[-76.58956728633741,40.94013520527931],[-76.60143828948856,40.942194204421455],[-76.62508229844035,40.96031720717415],[-76.635061301679,40.96438620817972],[-76.64533130567476,40.964432206983105],[-76.6524533077572,40.961651206597146],[-76.66135031078932,40.96800420736483],[-76.67486431452967,40.965510206238505],[-76.68212131659344,40.964970205864056],[-76.68714731847244,40.962761204943014],[-76.7348283327131,40.95445620222636],[-76.74302033582052,40.95449220185578],[-76.76737834263108,40.9497921999399],[-76.77570334593206,40.94947919930284],[-76.79261235128133,40.946655198410674],[-76.79005035058283,40.9516331991478],[-76.79050235070164,40.95671619988561],[-76.78544934939978,40.958915200543615],[-76.78654535035918,40.96517120234591],[-76.78490934948861,40.96693420256131],[-76.77371434813338,41.00256020969351],[-76.77578834930138,41.00812621018136],[-76.77377034970539,41.014364211553485],[-76.77059934833633,41.018735212483875],[-76.76196534585985,41.02594021437969],[-76.76450734747891,41.02961921481473],[-76.75967934683202,41.03871421745618],[-76.75650534692858,41.05051121960631],[-76.74650734412506,41.0655412231915],[-76.7348933421463,41.09214122863737],[-76.73419834351765,41.103809230371404],[-76.73534434393208,41.11010623170163],[-76.73351634394801,41.1276952356151],[-76.73580634565188,41.13784123710801],[-76.73169134612426,41.153247240428804],[-76.73127734645713,41.163088242108095],[-76.73267434730377,41.17204824365073],[-76.79080936636252,41.17574024179244],[-76.8259653767622,41.16667923904783],[-76.82817037757793,41.16578823874086],[-76.85691838637185,41.16364923707814],[-76.8702633905371,41.160063235730384],[-76.88415739446948,41.157354234984346],[-76.88814739564812,41.153815234087496],[-76.8961163969011,41.139078230926486],[-76.89792139669956,41.13298822941407],[-76.89588439586669,41.11998622726915],[-76.88968739154126,41.10132122418059],[-76.88438538982129,41.09376122310708],[-76.87271238541193,41.08271022122695],[-76.86520438261685,41.080235220972106],[-76.85833738000946,41.073086219838736],[-76.85698737986799,41.06602521867443],[-76.85757837821086,41.05553821690606],[-76.85619437841603,41.050553215154466],[-76.85776237743225,41.04407221452864],[-76.86129537831782,41.03806821301012],[-76.86125137798481,41.02849721144122],[-76.8647243783578,41.020360209413134],[-76.86743237815945,41.00775720656113],[-76.86758637812376,40.99847620474532],[-76.87011537868129,40.99194220350801],[-76.87558937907447,40.9845902024704],[-76.88187738053867,40.97310919939926],[-76.88225138027211,40.96877119853387],[-76.87739937838916,40.96015319714789],[-76.87622337802891,40.95109719541816],[-76.86979337451783,40.94212919390423],[-76.85992737052514,40.923986191127106],[-76.85147136694474,40.91285418973946],[-76.8226813563192,40.889707186154865],[-76.80649935060839,40.88601118591815],[-76.80024434817499,40.88200218499756],[-76.79871634774426,40.87837418437519],[-76.80070634851397,40.87260318335964],[-76.81025334956811,40.8545731798576],[-76.81281434980428,40.84711417841852],[-76.81802835189433,40.84330117723425],[-76.82968735493546,40.83103717409476],[-76.84062835708737,40.821332171767125],[-76.84981735975815,40.80893816900033],[-76.84906835882175,40.80550116857012],[-76.85216535987203,40.800847167819434],[-76.8560963603354,40.79121916539816],[-76.85925435985067,40.777051162845744],[-76.85628335836286,40.754795158365496],[-76.85752335767532,40.74962015736064],[-76.85540935604647,40.735051154587005],[-76.85649435566683,40.72263815266689],[-76.86118635593319,40.71160615056564],[-76.86525935662442,40.7046141483077],[-76.87432435928652,40.6929131458696],[-76.87985236101403,40.68720014449526],[-76.88709036315949,40.68259714381775],[-76.8962533653373,40.67868214283424],[-76.9038513672514,40.674104141365206],[-76.91495236997831,40.66467013871434],[-76.9201103711701,40.65587813711906],[-76.92762737258052,40.64571513487032],[-76.93988537592816,40.638150133375355],[-76.9491503790798,40.62817513019318],[-76.93696437326714,40.612849128282434],[-76.92549837017538,40.608899127984145],[-76.90334436270884,40.61190012925881],[-76.89887136138961,40.61046012901371],[-76.89004135828907,40.61033912938864],[-76.89025635877779,40.61628713071878],[-76.88682435827764,40.617716131061336],[-76.87271935385373,40.61632113132385],[-76.86953035323971,40.61839113217414],[-76.86948535293409,40.62348913279815],[-76.86425635213506,40.627593133988],[-76.85460134820646,40.62572813376081],[-76.84010634422437,40.625447134496255],[-76.83316434163825,40.627610134842165],[-76.82740734036804,40.63395413606591],[-76.81320433560245,40.63331713675045],[-76.8101513356167,40.634854137257335],[-76.80990433538666,40.64192413867473],[-76.80249433312115,40.64728814008554],[-76.7938533302861,40.640522139411416],[-76.78585532847747,40.641740139575354],[-76.7782833260665,40.645994140779706],[-76.75623431864581,40.64809614178823],[-76.74589631637652,40.654472143704844],[-76.73276231210131,40.65474114461708],[-76.72173130826788,40.653491144517204],[-76.71827530775207,40.65839714531215],[-76.71316930592054,40.65955914576016],[-76.70392630245547,40.65537814551448],[-76.70162630200974,40.65809014635093]]]},properties:{geoid:”42097″,name:”Northumberland”,state_name:”Pennsylvania”,county_state_name:”Northumberland County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.84,”27_65k_diff”:188.06,”40_65k_diff”:330.38,”60_65k_diff”:1218.95,”27_95k_diff”:0,”40_95k_diff”:117.88,”60_95k_diff”:1006.45,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.42,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:648.48,”40_95k_eptc”:672.92,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:648.48,”40_65k_no_eptc”:790.8,”60_65k_no_eptc”:1679.37,”27_95k_no_eptc”:648.48,”40_95k_no_eptc”:790.8,”60_95k_no_eptc”:1679.37}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-78.62038588139964,40.3270330055658],[-78.61809788110396,40.332107006903875],[-78.60223887848849,40.353637011301686],[-78.56146886590392,40.369678016236584],[-78.56095686688863,40.37503901743736],[-78.55289186812541,40.434791028572064],[-78.55772387005997,40.44157102974864],[-78.54846586857343,40.46186203453363],[-78.5440278680025,40.465958035305626],[-78.54045086709283,40.47639503741718],[-78.54431386881694,40.48279903872275],[-78.54471786920516,40.48669003889372],[-78.5414578685922,40.49707804099628],[-78.53982186896961,40.506301043138954],[-78.53038686702506,40.519152046033255],[-78.52266586515024,40.52326604712343],[-78.51821386426535,40.528810048194174],[-78.5118538628762,40.53144704939762],[-78.49756385878383,40.53917105168343],[-78.48612685508171,40.54084605167945],[-78.47905385331329,40.547315053329],[-78.45385284753203,40.5812570607064],[-78.44934684740537,40.59030606313603],[-78.44121084544587,40.5972470645868],[-78.44359084635249,40.60977406717303],[-78.44774784870808,40.62433906965805],[-78.44163884799188,40.63011907141843],[-78.44016984738485,40.63876907289557],[-78.4421588477873,40.64120007286923],[-78.43699984690515,40.64676007400486],[-78.42418784327221,40.64755507488838],[-78.41712684128233,40.64535807463319],[-78.40863183852075,40.64435707516488],[-78.34867082451186,40.72345109278674],[-78.40290184213443,40.72524709117394],[-78.47201486374082,40.72550708814574],[-78.52983088200665,40.72592708535565],[-78.56902589383435,40.72565008393748],[-78.63558491424357,40.72307408075504],[-78.69194493265458,40.7243440783578],[-78.80172896714336,40.724626073812],[-78.79964396582201,40.71727207274196],[-78.80886496898687,40.72107007278191],[-78.82668897143158,40.681758065114686],[-78.85067397514639,40.62634405338336],[-78.85968897651924,40.60705204955588],[-78.88594898069252,40.55407503800625],[-78.92192598691554,40.483520022642104],[-78.94609899120111,40.441758013644474],[-78.97381699652537,40.3954290037767],[-78.97523299724493,40.391935003406935],[-78.99817400177862,40.35617699537366],[-79.00608100395384,40.351210994178416],[-79.0102820036892,40.340235991984414],[-79.01537100565217,40.33919499134425],[-79.02002200668471,40.3356129905794],[-79.0254140081813,40.32601298831566],[-79.02971500942891,40.322976987801404],[-79.03166800860517,40.31765398672091],[-79.03729801044948,40.31341098545467],[-79.03756101023815,40.3069689844828],[-79.04505001242205,40.29965498217918],[-79.0460760120278,40.29657998213159],[-79.05605601496902,40.284868979579656],[-79.01585600160679,40.28542198059685],[-78.98176999112553,40.28544698263378],[-78.92711197417415,40.284740984606465],[-78.92479697322801,40.278495983242045],[-78.90205696592854,40.27479898378893],[-78.89623296394663,40.271595983611014],[-78.89440596335389,40.268496982463695],[-78.89716396312426,40.26373998149168],[-78.8925709617927,40.25780398069062],[-78.89087096108973,40.24975197959929],[-78.88467195851366,40.24458297829583],[-78.87984695655359,40.24723497962252],[-78.86866495392573,40.248890980398556],[-78.86494395184478,40.24470897923614],[-78.8600659503992,40.242906979505214],[-78.85317194848534,40.245730980158434],[-78.84804394688898,40.244908980538085],[-78.79340192938913,40.244194982236564],[-78.65830788788818,40.24324298753232],[-78.64381888416861,40.25914799117512],[-78.65174588794004,40.281531995440844],[-78.64270988578785,40.28307899575508],[-78.63538788477194,40.30950600110899],[-78.62567488344791,40.31932600381228],[-78.62038588139964,40.3270330055658]]]},properties:{geoid:”42021″,name:”Cambria”,state_name:”Pennsylvania”,county_state_name:”Cambria County, Pennsylvania”,”27_22k_diff”:66.19,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.84,”40_35k_diff”:131.84,”60_35k_diff”:131.84,”27_65k_diff”:72.39,”40_65k_diff”:189.32,”60_65k_diff”:919.39,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:706.89,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.42,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:532.81,”40_95k_eptc”:649.74,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.19,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.88,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:532.81,”40_65k_no_eptc”:649.74,”60_65k_no_eptc”:1379.81,”27_95k_no_eptc”:532.81,”40_95k_no_eptc”:649.74,”60_95k_no_eptc”:1379.81}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-75.50560896099414,41.23254730249383],[-75.50103695923991,41.236355303814854],[-75.49605895846172,41.24295630494504],[-75.48506095481743,41.242656304904436],[-75.48447895446124,41.24598230560803],[-75.4771239531072,41.24643030631951],[-75.47213195065932,41.24348330607199],[-75.46749994936674,41.24798730737139],[-75.4610869480694,41.24727630752537],[-75.4566869461302,41.25394630835841],[-75.44523594350929,41.25454130900015],[-75.44142294249704,41.260061310692016],[-75.44333894541562,41.29930331808209],[-75.44700295115975,41.36317733008492],[-75.44881295369622,41.40353233786683],[-75.45121295821163,41.44699934531825],[-75.45226895971464,41.47602735125495],[-75.45501296363192,41.51683635901951],[-75.45729296590626,41.546363364721415],[-75.45932896964635,41.58769137262985],[-75.46241297497549,41.641595382526575],[-75.50201198706773,41.6414503804131],[-75.65218903573849,41.64220437549063],[-75.71988905655843,41.64227137243547],[-75.71877605636554,41.636121371438286],[-75.72169905701998,41.63458637080089],[-75.7286820588079,41.63551037085701],[-75.77429206945506,41.57405635803612],[-75.76929906732823,41.56847435716094],[-75.78750507181545,41.54353935104098],[-75.80323207506703,41.52423534739867],[-75.77162806396235,41.505801344911994],[-75.83451407879005,41.42697332714255],[-75.83122507779213,41.41781432568665],[-75.8326330762135,41.39994232207193],[-75.82900107541926,41.39320632124073],[-75.81957707090676,41.38752632005466],[-75.80655206682017,41.38519132049916],[-75.79768806391024,41.38154331976724],[-75.79511806332282,41.37712731955304],[-75.76782805390746,41.36536231836461],[-75.74211604410696,41.34835231625126],[-75.68860802664369,41.33945431633162],[-75.68784302433029,41.317844311783865],[-75.69496102662772,41.31758531137591],[-75.69412202617936,41.30411830935113],[-75.69082602489559,41.304343309127276],[-75.68966302294805,41.28779330600367],[-75.67934601982368,41.287968306727535],[-75.67930601860425,41.264309301990856],[-75.65227500911016,41.25739130167986],[-75.65081400750572,41.22836729616607],[-75.64923500328311,41.18718128868667],[-75.64375300158248,41.18223628736472],[-75.64339400102224,41.17618028670948],[-75.63949900006148,41.17622228661457],[-75.63665299825492,41.17136728589345],[-75.63184499647642,41.16967728622814],[-75.62405599405338,41.16975828567355],[-75.61655999225242,41.172686286885344],[-75.61171899063872,41.16419528570538],[-75.60721798917173,41.16420228527307],[-75.60073798635908,41.16150528520922],[-75.59726698568855,41.1632122857356],[-75.59632998625506,41.171774287763434],[-75.58781398332859,41.17267428830049],[-75.58272598176494,41.17675328872011],[-75.57665497988646,41.17786528918583],[-75.57637298050626,41.186559290986644],[-75.57021297908811,41.19113829263629],[-75.57090497902834,41.19536929285059],[-75.56282097686547,41.20522729505485],[-75.55603797553961,41.207061296157356],[-75.55401897495379,41.21168829723709],[-75.54914597327462,41.21740829801617],[-75.53984797111873,41.22546929975977],[-75.53007396824685,41.22659630060556],[-75.52558596677227,41.22302530033269],[-75.51649296319853,41.21938829984886],[-75.50560896099414,41.23254730249383]]]},properties:{geoid:”42069″,name:”Lackawanna”,state_name:”Pennsylvania”,county_state_name:”Lackawanna County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.83,”40_35k_diff”:131.83,”60_35k_diff”:131.84,”27_65k_diff”:87.26,”40_65k_diff”:207.45,”60_65k_diff”:957.89,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:745.39,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.41,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:547.67,”40_95k_eptc”:667.87,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:547.67,”40_65k_no_eptc”:667.87,”60_65k_no_eptc”:1418.31,”27_95k_no_eptc”:547.67,”40_95k_no_eptc”:667.87,”60_95k_no_eptc”:1418.31}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-75.83451407879005,41.42697332714255],[-75.77162806396235,41.505801344911994],[-75.80323207506703,41.52423534739867],[-75.78750507181545,41.54353935104098],[-75.76929906732823,41.56847435716094],[-75.77429206945506,41.57405635803612],[-75.7286820588079,41.63551037085701],[-75.72169905701998,41.63458637080089],[-75.71877605636554,41.636121371438286],[-75.71988905655843,41.64227137243547],[-75.76792607296244,41.64341737102821],[-75.79222207951375,41.64205836976743],[-75.79733808184567,41.64262336949335],[-75.83189009254183,41.6431503680604],[-75.86872610508956,41.644364367565544],[-75.87901110845353,41.643470366907664],[-75.97273113852145,41.644325363190724],[-75.98630614225289,41.64480936312621],[-76.01430615078603,41.64427736162385],[-76.08776117434924,41.644732359030186],[-76.11422618345833,41.64339335801251],[-76.11517418356637,41.65183335871219],[-76.16343719860026,41.6492633567604],[-76.19800021007026,41.647831355482865],[-76.20875021016779,41.59176534379714],[-76.22007521020504,41.54128633423914],[-76.22386821027341,41.524552330742516],[-76.22813321055723,41.511145327804925],[-76.27678621776558,41.39157630359638],[-76.28280121799624,41.37725230034644],[-76.15888317932804,41.3799153061574],[-76.05247514488201,41.382714310758246],[-76.00507213009493,41.38455931309379],[-75.98327212345266,41.391071314785975],[-75.96884111945245,41.394040316225514],[-75.92914610732264,41.40348131876394],[-75.9014070987122,41.409571321319056],[-75.83928908053936,41.42464132622879],[-75.83451407879005,41.42697332714255]]]},properties:{geoid:”42131″,name:”Wyoming”,state_name:”Pennsylvania”,county_state_name:”Wyoming County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.83,”40_35k_diff”:131.83,”60_35k_diff”:131.84,”27_65k_diff”:87.26,”40_65k_diff”:207.45,”60_65k_diff”:957.89,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:745.39,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.41,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:547.67,”40_95k_eptc”:667.87,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:547.67,”40_65k_no_eptc”:667.87,”60_65k_no_eptc”:1418.31,”27_95k_no_eptc”:547.67,”40_95k_no_eptc”:667.87,”60_95k_no_eptc”:1418.31}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-74.1614294943361,40.64415623718283],[-74.14311148861802,40.641998237751245],[-74.13292248498342,40.643692237939746],[-74.12601948316374,40.64215923833303],[-74.10984947758494,40.64807224050505],[-74.09344347253494,40.648073240188666],[-74.08698747045922,40.65151424172364],[-74.05575046018984,40.651484242309394],[-74.02639145436132,40.70011125312305],[-74.02363845504735,40.71807725685151],[-74.01403045387019,40.75755926482289],[-73.98474044743897,40.79767027399576],[-73.99331145036126,40.80129427393276],[-73.99316244988552,40.80576727531177],[-74.01235345720568,40.81598527634865],[-74.01129445636487,40.82048327736237],[-74.0178204591164,40.82334927783566],[-74.020415459496,40.81865227645284],[-74.03165346256444,40.81326427528074],[-74.03654046371511,40.80785627390748],[-74.0585504709564,40.806285272961404],[-74.0638384727666,40.80416027191772],[-74.06903347420536,40.798357270968324],[-74.07785647698009,40.79429126998716],[-74.07985147735964,40.78973426843448],[-74.08914447945943,40.77960426651512],[-74.09009947932442,40.776891265612925],[-74.0879804780222,40.76444826396033],[-74.09583748089385,40.76286826286144],[-74.0986984818018,40.767749263601324],[-74.0984374815692,40.77253226475192],[-74.10533848478549,40.77716726573075],[-74.11396048751706,40.77631626492335],[-74.11640648770812,40.77328126396205],[-74.12719149031524,40.77135026314362],[-74.13077249257661,40.77784826466762],[-74.14753049846883,40.78649926612258],[-74.14898849859632,40.77800926448031],[-74.15579949949817,40.77082326290091],[-74.15768950022104,40.766108261139834],[-74.162075501915,40.76148726047739],[-74.16451450141533,40.75639625918568],[-74.16598850174887,40.74520725741019],[-74.16209449973866,40.736117255544464],[-74.15568849777907,40.733509255361604],[-74.14718949469946,40.7344092560545],[-74.14268949384575,40.739309256869205],[-74.13749349280108,40.74140625703545],[-74.12278748712284,40.742109257739415],[-74.11699448576331,40.73713325737274],[-74.1213884861359,40.72100925429412],[-74.12028848479173,40.715909253227636],[-74.11278848154636,40.70311025029891],[-74.13670448743999,40.674452244119436],[-74.1614294943361,40.64415623718283]]]},properties:{geoid:”34017″,name:”Hudson”,state_name:”New Jersey”,county_state_name:”Hudson County, New Jersey”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:84.32,”60_65k_diff”:696.41,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:483.91,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.05,”27_65k_eptc”:446.7,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:446.7,”40_95k_eptc”:544.74,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:446.7,”40_65k_no_eptc”:544.74,”60_65k_no_eptc”:1156.83,”27_95k_no_eptc”:446.7,”40_95k_no_eptc”:544.74,”60_95k_no_eptc”:1156.83}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-75.47419492314522,40.81475422275559],[-75.44245191310688,40.81837522496968],[-75.4204919070842,40.8234592265384],[-75.41676090633787,40.82611022766176],[-75.38326789617236,40.83104522938131],[-75.34175388313587,40.84532523424737],[-75.32093287687469,40.855665236994014],[-75.30059587100052,40.85957123814031],[-75.28404086635061,40.86604823999217],[-75.27353186293368,40.87315824177394],[-75.26722586156586,40.8824812437561],[-75.23250385244768,40.899767248429306],[-75.24113185540114,40.90944624981751],[-75.22182285017612,40.91958925296117],[-75.2181918492665,40.9278832542831],[-75.19553784318018,40.93634525670534],[-75.18753284050696,40.93713925712137],[-75.17807483687362,40.940328258302294],[-75.17683783695009,40.94553125946161],[-75.16946483563434,40.94802326030047],[-75.15293682968124,40.94931926085197],[-75.14513182715606,40.95159226223099],[-75.1292338227182,40.95893826391864],[-75.1202338206216,40.968710266306424],[-75.12260482195131,40.97016026617142],[-75.13136182371711,40.969284266240216],[-75.13470282574909,40.97204626665588],[-75.13552282579911,40.976873267582434],[-75.1325238259745,40.98124326802266],[-75.13057682588925,40.99110127037043],[-75.12342482378877,40.996137271732486],[-75.11059681952965,41.00218227337742],[-75.10911481947527,41.00411027308198],[-75.09352481437521,41.00945027525745],[-75.084496812114,41.01592827616387],[-75.07053380757272,41.01862827726548],[-75.04755880088854,41.02969728061591],[-75.0401077992365,41.03274328152878],[-75.03505979795551,41.03684428206985],[-75.02684879496495,41.03973928366525],[-75.02739179599833,41.0441142841539],[-75.01713079357857,41.05663128667839],[-75.0134707924994,41.06594928865975],[-75.00656579048916,41.06779028911636],[-75.00078178977809,41.073218291038124],[-74.9948487870941,41.07656429117817],[-74.98259178366823,41.07918029244987],[-74.97098878101372,41.0853012943927],[-74.967409779313,41.09012529493623],[-74.96690777928738,41.09441829601194],[-74.96943578034174,41.09608229599501],[-74.97689078305659,41.093188295318555],[-74.98131578450409,41.08986829509079],[-74.98826478643308,41.08823029448086],[-74.99171978728133,41.09229229512348],[-75.00031478961411,41.08949329393185],[-75.00317879104723,41.091781294024564],[-75.01260379375141,41.083809292260746],[-75.01854879526348,41.084896292385054],[-75.0250027979941,41.08352529145997],[-75.03259479966785,41.08527529167501],[-75.03921780269076,41.08880529275467],[-75.07681281797053,41.14113030079367],[-75.10599482717312,41.144209300845674],[-75.15650884454317,41.150349300182725],[-75.14788084311895,41.18222430605277],[-75.1297228424135,41.25210932030635],[-75.24208787747756,41.245898314872605],[-75.35918591495425,41.239214309331466],[-75.37462891996248,41.23779130831702],[-75.45905994632388,41.23421230483277],[-75.50560896099414,41.23254730249383],[-75.51649296319853,41.21938829984886],[-75.52558596677227,41.22302530033269],[-75.53007396824685,41.22659630060556],[-75.53984797111873,41.22546929975977],[-75.54914597327462,41.21740829801617],[-75.55401897495379,41.21168829723709],[-75.55603797553961,41.207061296157356],[-75.56282097686547,41.20522729505485],[-75.57090497902834,41.19536929285059],[-75.57021297908811,41.19113829263629],[-75.57637298050626,41.186559290986644],[-75.57665497988646,41.17786528918583],[-75.58272598176494,41.17675328872011],[-75.58781398332859,41.17267428830049],[-75.59632998625506,41.171774287763434],[-75.59726698568855,41.1632122857356],[-75.60073798635908,41.16150528520922],[-75.60450198777228,41.15611828427447],[-75.6030909866706,41.15215728335735],[-75.60931398849021,41.15006028328017],[-75.61557899042838,41.15071328304942],[-75.61417498922205,41.145176281646954],[-75.62838699403997,41.136854279551265],[-75.62806999276668,41.12829527832712],[-75.63283199421141,41.12795327764738],[-75.63416399463159,41.123254276870775],[-75.64026699700602,41.12683127711843],[-75.64838599991205,41.125503277093856],[-75.64941399940439,41.1223122757284],[-75.6457469974766,41.11814227562345],[-75.64397099759316,41.11278127429677],[-75.63758899567219,41.11340627469995],[-75.63297999344124,41.108542273717084],[-75.62824399211938,41.10690927368858],[-75.62613199136018,41.11060527475116],[-75.62003898891767,41.108979274171325],[-75.61594998738674,41.104767273956526],[-75.61269598574593,41.094245271716275],[-75.60489598348023,41.09415127234795],[-75.60606798324572,41.08563227079985],[-75.60081898137327,41.084489270420924],[-75.59602197914961,41.08068526966728],[-75.582966975418,41.07264326869702],[-75.5805129741315,41.06777226854893],[-75.57648597286114,41.06758126825707],[-75.57488897204756,41.062699267651695],[-75.57118797070319,41.05931226682702],[-75.56957596964406,41.04997126545473],[-75.56194896720088,41.049531265581464],[-75.50849894643657,40.99818525767002],[-75.49599194162418,40.98718925582477],[-75.54624695627125,40.96461124925009],[-75.57459196453078,40.95133124623588],[-75.5607289593929,40.934257242644996],[-75.52641494507999,40.88984423621281],[-75.49358293195809,40.84645022815633],[-75.48257892742166,40.829939226220425],[-75.47419492314522,40.81475422275559]]]},properties:{geoid:”42089″,name:”Monroe”,state_name:”Pennsylvania”,county_state_name:”Monroe County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.84,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:36.06,”60_65k_diff”:593.92,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:381.42,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:407.13,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:407.13,”40_95k_eptc”:496.48,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.88,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.87,”27_65k_no_eptc”:407.13,”40_65k_no_eptc”:496.48,”60_65k_no_eptc”:1054.34,”27_95k_no_eptc”:407.13,”40_95k_no_eptc”:496.48,”60_95k_no_eptc”:1054.34}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-77.98919676600318,41.47483024981132],[-78.05044478512805,41.47547024742285],[-78.08047379699903,41.50327025171817],[-78.10291980560496,41.52450825467008],[-78.12133481349211,41.541322257172496],[-78.14174382082307,41.56066625951145],[-78.18785683915024,41.6036992663076],[-78.20364284484296,41.617607267608605],[-78.31494687936173,41.617462263289546],[-78.42084891328138,41.61729225886754],[-78.42050091156848,41.60188225592037],[-78.41841090783224,41.5571632474274],[-78.41843390706117,41.54396224467334],[-78.42016390695669,41.54405524545284],[-78.4201589044987,41.499032236551976],[-78.4211569028996,41.47385323176947],[-78.41956890224493,41.473732231719254],[-78.42003089713813,41.40505421854076],[-78.29366885764182,41.404672224453364],[-78.25396184461174,41.40472922614803],[-78.25433384306072,41.37510922061789],[-78.2543848387236,41.32359221064248],[-78.23467783263028,41.323421211127794],[-78.23460483066961,41.29880420659386],[-78.23577682804549,41.25016219779322],[-78.23681982615311,41.23048319410352],[-78.18824381039407,41.226002194665746],[-78.09338378033888,41.21693919696318],[-78.01326676296522,41.33103022195826],[-77.98878875842213,41.367461230104055],[-77.98846475934405,41.388507234279516],[-77.98919676600318,41.47483024981132]]]},properties:{geoid:”42023″,name:”Cameron”,state_name:”Pennsylvania”,county_state_name:”Cameron County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.84,”27_65k_diff”:220.37,”40_65k_diff”:369.77,”60_65k_diff”:1302.6,”27_95k_diff”:7.87,”40_95k_diff”:157.27,”60_95k_diff”:1090.1,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.41,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:672.91,”40_95k_eptc”:672.92,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:680.78,”40_65k_no_eptc”:830.19,”60_65k_no_eptc”:1763.02,”27_95k_no_eptc”:680.78,”40_95k_no_eptc”:830.19,”60_95k_no_eptc”:1763.02}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-76.99932033488686,39.720113951386594],[-76.9909053322142,39.719806951541145],[-76.93652131498652,39.72071395334708],[-76.89104830096765,39.720397955390744],[-76.8574772896532,39.72040895616583],[-76.70448224253076,39.7211189622543],[-76.6445972240392,39.72110796473085],[-76.60142921049838,39.72130696660586],[-76.59546420847356,39.720456966202576],[-76.5838782042562,39.72130996664629],[-76.51479118251657,39.721134969823204],[-76.48336517266661,39.72132697113053],[-76.41484315120908,39.72118297327817],[-76.3845851419934,39.721310974963686],[-76.23980709677257,39.72134298019924],[-76.2386920964639,39.72510098076914],[-76.24058409676744,39.73032098130485],[-76.24557509917183,39.737181983077676],[-76.24958610103906,39.73998798321407],[-76.25656610365262,39.75004798535495],[-76.26057910471546,39.75204298571329],[-76.26747710765376,39.759365986366454],[-76.27160010949866,39.76581398760618],[-76.27611511066279,39.77562798944096],[-76.29018411661636,39.785018990746856],[-76.31107612410295,39.8036379936924],[-76.31570412628575,39.81004499497688],[-76.3283551297366,39.81479599479346],[-76.33825713391616,39.82206999586576],[-76.34240313484713,39.82887399750607],[-76.35054513843878,39.83776399924371],[-76.35076113903693,39.84709800097023],[-76.36167614266724,39.857062001978036],[-76.3696431454091,39.86040700310215],[-76.37665914805086,39.865650003665344],[-76.380694150212,39.8736830045193],[-76.38171115121126,39.87906800577658],[-76.37964415088032,39.88820900740188],[-76.38377915194297,39.893625008577715],[-76.38578815423175,39.90617501094299],[-76.39167615557949,39.91282701215326],[-76.40567216058636,39.91596301231397],[-76.42215816624795,39.925840013222896],[-76.4304031697123,39.928915013977544],[-76.44897117506329,39.934346014301816],[-76.45975217970766,39.94125801522412],[-76.467579182251,39.94305701560825],[-76.47358218435305,39.94736001573092],[-76.47920918661231,39.95482101700314],[-76.48739118924969,39.9621430187101],[-76.49535419295003,39.97613602036241],[-76.49845619491794,39.99673802470769],[-76.5006131956169,40.00063202571396],[-76.50958819953439,40.00943102647174],[-76.5136402004953,40.01563102782035],[-76.52032920351424,40.02003002857458],[-76.52787020605581,40.027998030074556],[-76.53217020850198,40.038240031479994],[-76.5315542088517,40.04616503333376],[-76.53452621006944,40.05135603441562],[-76.54145721210712,40.05104503353432],[-76.55389721630074,40.04673303211755],[-76.57121922064641,40.04567703179134],[-76.58848422645728,40.0493210314328],[-76.59759022944908,40.05187503150779],[-76.61336823527071,40.054485031576334],[-76.62060023700697,40.05473703112901],[-76.6436202448794,40.05962703201242],[-76.65372424789807,40.05982103169194],[-76.66382725176288,40.06323503168069],[-76.67550625540453,40.073604032928586],[-76.68043025782265,40.08320003489499],[-76.68753126113413,40.0923110360288],[-76.69718926481309,40.102500037836],[-76.71093426963078,40.1138510393754],[-76.72162227347948,40.120078040625785],[-76.73265427715316,40.122740040219476],[-76.7435392813275,40.13085804214603],[-76.74557028204892,40.13930604311691],[-76.74579228264591,40.145801044192794],[-76.74826128375427,40.1557690461917],[-76.74911428493915,40.167121048716055],[-76.75319728649042,40.176051050167295],[-76.76303628985261,40.17896305080871],[-76.77401629427925,40.184099051328225],[-76.7876702986242,40.191558051771054],[-76.80058730276451,40.200119053175456],[-76.82164031014557,40.20135105244922],[-76.82886131270374,40.20502805270404],[-76.83478731503212,40.21797005525046],[-76.8394703169858,40.221623056105244],[-76.85902532342105,40.2263360555814],[-76.8617533240989,40.22329705562806],[-76.86089532331982,40.21942205420727],[-76.86701732514429,40.21601005379039],[-76.872746326463,40.215633053676314],[-76.87750032827067,40.217842053839185],[-76.88562733072003,40.214001052220155],[-76.89180333253697,40.21590305302336],[-76.89696333566877,40.2246740546165],[-76.9033233371249,40.22111205340639],[-76.89867833543953,40.214640052592685],[-76.90257733608978,40.212984051825835],[-76.91053933800566,40.2055490497849],[-76.91491833975974,40.20594804979778],[-76.91785534054202,40.21038605057932],[-76.92221634208398,40.208348049788555],[-76.9294833431062,40.19686104764277],[-76.9186143404828,40.19831904852651],[-76.91330533794861,40.193195047123304],[-76.90855733623825,40.19073704669236],[-76.91345333776471,40.18768504635855],[-76.91672233832412,40.18324504491457],[-76.9202763406007,40.18648204594949],[-76.92655034241425,40.18848804594378],[-76.92830534205812,40.18381004487448],[-76.92329634010858,40.17709504416048],[-76.9076523345844,40.169380042556504],[-76.90728333462425,40.16549204236259],[-76.92910934144895,40.16128204060814],[-76.93928534490408,40.164272040733465],[-76.94991934781493,40.16579204089171],[-76.96687835335035,40.16271203904599],[-76.97802635701895,40.164785039659215],[-76.98067735742634,40.16056403883004],[-76.97366435449011,40.15929503881382],[-76.97122835368218,40.15703003786216],[-76.97477035515263,40.15323403688601],[-76.97901135581367,40.152037036501135],[-76.98681435929338,40.15513503758037],[-76.99236836109756,40.15517503658733],[-77.00365436371848,40.153110035996136],[-77.0113453659509,40.148457035157996],[-77.01967736910764,40.148317034622714],[-77.02275136985408,40.14582203417488],[-77.02886337150336,40.14774003371527],[-77.05521737848785,40.12906902908971],[-77.13742740030403,40.06995301460877],[-77.1279183975036,40.06869701491253],[-77.12344639559458,40.066201014845234],[-77.10630939063365,40.059767013979865],[-77.10431838909203,40.057965013572755],[-77.09263038492996,40.05392801365524],[-77.08081438079809,40.04323001198435],[-77.07856538002626,40.03787601096683],[-77.07235637736383,40.03401701008911],[-77.06848737582618,40.02888000958344],[-77.05618337149319,40.02344600852355],[-77.04069236730403,40.02132800916406],[-77.03321336495505,40.01873200863215],[-77.0262403624896,40.01838600896512],[-77.01865035984494,40.013955008176794],[-77.01054935623439,40.00048900594462],[-76.99267434846347,39.97320500142198],[-76.9861073464329,39.96438999995041],[-76.96961733927196,39.93990499561544],[-76.97258733969296,39.93419499458095],[-76.9710623398338,39.9309629938065],[-76.97235433897715,39.92614899313678],[-76.96715933729563,39.92211299186651],[-76.96698533696606,39.916190990655174],[-76.97284133844839,39.91386899011796],[-76.97288333867516,39.91108898941145],[-76.98385134194983,39.902064988025565],[-76.98205734021668,39.897403986536105],[-76.98399434113279,39.89473898625389],[-76.97771633851234,39.885805984735654],[-76.9783593387744,39.88215898342427],[-76.97253833627983,39.872921982077585],[-76.96362233339624,39.8740249828874],[-76.96224033244802,39.86484298065306],[-76.95493432926331,39.85685798007115],[-76.96484233189707,39.85077997858403],[-76.97408533532865,39.849667977649666],[-76.97854533671271,39.847734976673046],[-76.98304533696516,39.84136097531205],[-76.99066533977654,39.83435597355847],[-77.00031434188568,39.83122697315669],[-76.99965234057116,39.81964197060366],[-76.99932033488686,39.720113951386594]]]},properties:{geoid:”42133″,name:”York”,state_name:”Pennsylvania”,county_state_name:”York County, Pennsylvania”,”27_22k_diff”:66.19,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.84,”40_35k_diff”:131.84,”60_35k_diff”:131.84,”27_65k_diff”:237.88,”40_65k_diff”:391.13,”60_65k_diff”:1347.96,”27_95k_diff”:25.38,”40_95k_diff”:178.63,”60_95k_diff”:1135.46,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.42,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:672.92,”40_95k_eptc”:672.92,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.19,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.88,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:698.3,”40_65k_no_eptc”:851.55,”60_65k_no_eptc”:1808.38,”27_95k_no_eptc”:698.3,”40_95k_no_eptc”:851.55,”60_95k_no_eptc”:1808.38}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-78.71025097311792,41.201867168791466],[-78.64794995443046,41.217468174043],[-78.64666895660407,41.25378618130476],[-78.57869993550045,41.24959018287462],[-78.53195092005032,41.24646418435875],[-78.44589289307027,41.241839186853895],[-78.32398485462899,41.235147190564604],[-78.23681982615311,41.23048319410352],[-78.23577682804549,41.25016219779322],[-78.23460483066961,41.29880420659386],[-78.23467783263028,41.323421211127794],[-78.2543848387236,41.32359221064248],[-78.25433384306072,41.37510922061789],[-78.25396184461174,41.40472922614803],[-78.29366885764182,41.404672224453364],[-78.42003089713813,41.40505421854076],[-78.41956890224493,41.473732231719254],[-78.4211569028996,41.47385323176947],[-78.4201589044987,41.499032236551976],[-78.42016390695669,41.54405524545284],[-78.41843390706117,41.54396224467334],[-78.41841090783224,41.5571632474274],[-78.42050091156848,41.60188225592037],[-78.48291193089456,41.602338252993306],[-78.48381793430207,41.63148925843768],[-78.67601899417578,41.62498124928695],[-78.74462301593944,41.62518024682105],[-78.81524003811533,41.624257243046785],[-78.81497403735332,41.622681242584356],[-78.95614108170575,41.62334223674294],[-78.95742107926122,41.579230228574126],[-78.9579720766536,41.54608722210068],[-78.95913107364252,41.50012321380402],[-78.95896006853444,41.437069202253845],[-78.97666007378795,41.43697120093783],[-78.97666107492586,41.45176920372955],[-79.06352310305736,41.45321520026171],[-79.06515710074572,41.423202195026406],[-79.09359111023376,41.42329419374372],[-79.0947321069197,41.375121184450315],[-79.09509910453046,41.34066617808423],[-79.09160910311122,41.34096117872043],[-79.08112910110286,41.35269918056809],[-79.07670909898594,41.35425718169105],[-79.06624209615103,41.35038918116007],[-79.05221809183755,41.35113018209302],[-79.03996408821595,41.35668418386103],[-79.02778908458339,41.35721318396196],[-79.02033208179826,41.35050218302616],[-79.01635707986401,41.35100718353058],[-79.01405608003626,41.357642184388276],[-79.0038200763276,41.3590251856226],[-78.99269107355127,41.368624187575065],[-78.98155107051939,41.36776118799514],[-78.97448106865815,41.37548418992503],[-78.96981006741947,41.37590419007209],[-78.96654706584556,41.37094018958921],[-78.95944906340542,41.37115218953436],[-78.95916006279981,41.362169188277235],[-78.874757033943,41.32496918458002],[-78.81196701213878,41.29687218244804],[-78.74977699095443,41.269528179796445],[-78.73528298574165,41.2629231787482],[-78.73910398541629,41.25377617671173],[-78.73821698371718,41.23068017279338],[-78.71006197495215,41.23025117385549],[-78.71025097311792,41.201867168791466]]]},properties:{geoid:”42047″,name:”Elk”,state_name:”Pennsylvania”,county_state_name:”Elk County, Pennsylvania”,”27_22k_diff”:66.19,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.84,”40_35k_diff”:131.84,”60_35k_diff”:131.84,”27_65k_diff”:180.83,”40_65k_diff”:321.56,”60_65k_diff”:1200.22,”27_95k_diff”:0,”40_95k_diff”:109.06,”60_95k_diff”:987.72,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.42,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:641.25,”40_95k_eptc”:672.92,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.19,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.88,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:641.25,”40_65k_no_eptc”:781.98,”60_65k_no_eptc”:1660.64,”27_95k_no_eptc”:641.25,”40_95k_no_eptc”:781.98,”60_95k_no_eptc”:1660.64}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-74.55310658464879,40.079138112480855],[-74.52732457756301,40.09028411569992],[-74.46563456018981,40.13119712559035],[-74.4067115444824,40.172410135742794],[-74.26145649742674,40.16704113942541],[-74.25820849571615,40.16011813901614],[-74.26020649665621,40.15671213744617],[-74.25984249601413,40.149174136266744],[-74.25322849366782,40.147476136095165],[-74.25010149184604,40.144186135548175],[-74.24668549127415,40.13641913467811],[-74.24183448898114,40.13096713370128],[-74.2422084887361,40.12406413232445],[-74.24458348919167,40.118148130544235],[-74.23960548734662,40.1123911297909],[-74.2306354839468,40.1095691291913],[-74.20916147706713,40.110622130561545],[-74.20388947529665,40.112558131179064],[-74.19196047167762,40.111082131014484],[-74.17933546834253,40.1109711315366],[-74.17412146570284,40.10835213090684],[-74.15876146083968,40.105997131048916],[-74.15440545981605,40.09972713039913],[-74.15031645747145,40.0988851299434],[-74.10780544667678,40.13692613882058],[-74.10334644511276,40.13442013843278],[-74.10333544484098,40.13126913786761],[-74.09904044352587,40.12778913743613],[-74.09406244090142,40.11501313534026],[-74.09422344104658,40.10751713360448],[-74.08385143667631,40.0958511315726],[-74.07237443217763,40.08938913091888],[-74.07025243150562,40.089414131104576],[-74.0614914292183,40.09603613266464],[-74.05679442760382,40.097871133323615],[-74.05578442849924,40.10106813428668],[-74.04412242431913,40.10534113550313],[-74.03864442212284,40.104464135404704],[-74.02788141876022,40.09922313457983],[-74.00718041251822,40.097723134784786],[-73.96541539917973,40.097650136383805],[-73.96626639977686,40.10860513802747],[-73.96051439852359,40.1251221420655],[-73.94688139615262,40.15438914841614],[-73.93253139394479,40.19229815639373],[-73.90686438966559,40.25011916845519],[-73.89820938728701,40.2743611736369],[-73.89079238817644,40.310698181215926],[-73.88708338844961,40.3450171883953],[-73.88674739071291,40.37511719402733],[-73.88674739297078,40.42423520338492],[-73.88506139419832,40.452784209877294],[-73.88674839662654,40.47590021411427],[-73.88964639812036,40.48651921596042],[-73.90214140165078,40.492129217078855],[-73.97787542828557,40.519103219556925],[-74.15882248347943,40.4880312068833],[-74.2253325044568,40.47658620257219],[-74.22819750591599,40.477629202336495],[-74.2227385014073,40.45106019773331],[-74.22708450333957,40.44452519596365],[-74.23083150402667,40.44572919641955],[-74.23640850617619,40.44345319545843],[-74.24779850881744,40.43120519230227],[-74.24789550697571,40.406613187731146],[-74.25954751010073,40.39734218573611],[-74.31945052682144,40.35083317422997],[-74.37754654301254,40.30544016351898],[-74.39423254693732,40.28839815915692],[-74.39343954603507,40.279556157266235],[-74.46077756620947,40.25136614970524],[-74.46430256648924,40.25225314950386],[-74.48496357336015,40.25333314887041],[-74.48566057320403,40.248828148209064],[-74.48147757182058,40.242898147547876],[-74.54326958980442,40.21670013949693],[-74.54860159124449,40.2076931373882],[-74.5574115929312,40.199424135736244],[-74.56259259398442,40.189951133952704],[-74.57124259747604,40.18530113297325],[-74.5742935983779,40.187050132681094],[-74.58606160208139,40.184064131431775],[-74.5936766040533,40.17942913027156],[-74.5970936051282,40.18615013212174],[-74.59963660637793,40.18679913163061],[-74.614577610273,40.18239113050463],[-74.60929560827101,40.172019128515004],[-74.60402960640529,40.165428127324326],[-74.5878365995023,40.13826212303293],[-74.57950859650835,40.123550120190274],[-74.55310658464879,40.079138112480855]]]},properties:{geoid:”34025″,name:”Monmouth”,state_name:”New Jersey”,county_state_name:”Monmouth County, New Jersey”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:84.32,”60_65k_diff”:696.41,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:483.91,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.05,”27_65k_eptc”:446.7,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:446.7,”40_95k_eptc”:544.74,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:446.7,”40_65k_no_eptc”:544.74,”60_65k_no_eptc”:1156.83,”27_95k_no_eptc”:446.7,”40_95k_no_eptc”:544.74,”60_95k_no_eptc”:1156.83}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-75.47419492314522,40.81475422275559],[-75.48257892742166,40.829939226220425],[-75.49358293195809,40.84645022815633],[-75.52641494507999,40.88984423621281],[-75.5607289593929,40.934257242644996],[-75.57459196453078,40.95133124623588],[-75.54624695627125,40.96461124925009],[-75.49599194162418,40.98718925582477],[-75.50849894643657,40.99818525767002],[-75.56194896720088,41.049531265581464],[-75.56957596964406,41.04997126545473],[-75.57118797070319,41.05931226682702],[-75.57488897204756,41.062699267651695],[-75.57648597286114,41.06758126825707],[-75.5805129741315,41.06777226854893],[-75.582966975418,41.07264326869702],[-75.59602197914961,41.08068526966728],[-75.60081898137327,41.084489270420924],[-75.60606798324572,41.08563227079985],[-75.60489598348023,41.09415127234795],[-75.61269598574593,41.094245271716275],[-75.61594998738674,41.104767273956526],[-75.62003898891767,41.108979274171325],[-75.62613199136018,41.11060527475116],[-75.62824399211938,41.10690927368858],[-75.63297999344124,41.108542273717084],[-75.63758899567219,41.11340627469995],[-75.64397099759316,41.11278127429677],[-75.6457469974766,41.11814227562345],[-75.64941399940439,41.1223122757284],[-75.65454800101179,41.11657327443397],[-75.65821600191015,41.118559274646394],[-75.65642600226462,41.122939275832806],[-75.66150400353779,41.12923327668037],[-75.66749700629481,41.13398827731758],[-75.67861101008448,41.133031277239354],[-75.6842890107826,41.13042427631572],[-75.6913130133215,41.1314952761113],[-75.70059501653894,41.127331274919044],[-75.70281601698916,41.12262727420474],[-75.70967001866578,41.121994273890444],[-75.70789701730764,41.11630627224864],[-75.71648702084985,41.118209272457094],[-75.72365602240458,41.109442271132494],[-75.72883602374353,41.10800027047174],[-75.73250102506634,41.10297626885526],[-75.74083702688628,41.102232268296625],[-75.74737102930341,41.10393726836191],[-75.75436503129751,41.102313268169794],[-75.7528450312599,41.09723826681381],[-75.75502503131452,41.09407126693676],[-75.7614720327062,41.091581265597895],[-75.7675520349764,41.091663265513056],[-75.76566803452504,41.084398264218365],[-75.77197603541579,41.07690026297156],[-75.7700450338728,41.068419260821514],[-75.77153803413337,41.06109725945122],[-75.77044003278034,41.050560257340344],[-75.76554203103774,41.043976256829865],[-75.761227029611,41.04106325586419],[-75.75756102827013,41.03154725440231],[-75.74274702375853,41.03140525457928],[-75.73915102127594,41.02803925449413],[-75.73846802038115,41.016828252087706],[-75.7321850180767,41.00813225103125],[-75.76467402792062,40.99671824770941],[-75.80170403866612,40.98292524339953],[-75.81957704397104,40.98207724234582],[-75.84962705324428,40.97161323953712],[-75.84802605265959,40.96636523801128],[-75.86886005820516,40.959357236599594],[-75.89264606508156,40.950564233313024],[-75.9976380967849,40.913267222141855],[-75.95534508006574,40.87648621684498],[-75.92737707053477,40.85255821377387],[-75.90836206318228,40.8355832110872],[-75.88603905467338,40.81627520830219],[-75.87084104925418,40.806956206892075],[-75.82891003455461,40.780118202811394],[-75.82210703209708,40.77612920269758],[-75.78156701689963,40.75010119935488],[-75.75780900892455,40.735422197089406],[-75.74486500504854,40.740317198482565],[-75.73931100355661,40.7441631998016],[-75.7286020005005,40.75392320144811],[-75.70241999269837,40.76224820406957],[-75.6946229907684,40.77019420654971],[-75.67277298446993,40.775731207976875],[-75.60898696512045,40.78739521249067],[-75.6026099626999,40.788051213023515],[-75.59545496107634,40.79331021407364],[-75.57748995545315,40.79942221653372],[-75.56509295186183,40.801113216840854],[-75.55753394919063,40.80119621749638],[-75.55136094708338,40.804560218085385],[-75.54155094402422,40.80682321951487],[-75.52844594001286,40.80673321979385],[-75.51904693711276,40.80882122014777],[-75.50801993408191,40.809109220545494],[-75.48527392661572,40.812533222550655],[-75.47419492314522,40.81475422275559]]]},properties:{geoid:”42025″,name:”Carbon”,state_name:”Pennsylvania”,county_state_name:”Carbon County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.84,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:36.06,”60_65k_diff”:593.92,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:381.42,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:407.13,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:407.13,”40_95k_eptc”:496.48,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.88,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.87,”27_65k_no_eptc”:407.13,”40_65k_no_eptc”:496.48,”60_65k_no_eptc”:1054.34,”27_95k_no_eptc”:407.13,”40_95k_no_eptc”:496.48,”60_95k_no_eptc”:1054.34}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-78.34867082451186,40.72345109278674],[-78.40863183852075,40.64435707516488],[-78.41712684128233,40.64535807463319],[-78.42418784327221,40.64755507488838],[-78.43699984690515,40.64676007400486],[-78.4421588477873,40.64120007286923],[-78.44016984738485,40.63876907289557],[-78.44163884799188,40.63011907141843],[-78.44774784870808,40.62433906965805],[-78.44359084635249,40.60977406717303],[-78.44121084544587,40.5972470645868],[-78.44934684740537,40.59030606313603],[-78.45385284753203,40.5812570607064],[-78.47905385331329,40.547315053329],[-78.48612685508171,40.54084605167945],[-78.49756385878383,40.53917105168343],[-78.5118538628762,40.53144704939762],[-78.51821386426535,40.528810048194174],[-78.52266586515024,40.52326604712343],[-78.53038686702506,40.519152046033255],[-78.53982186896961,40.506301043138954],[-78.5414578685922,40.49707804099628],[-78.54471786920516,40.48669003889372],[-78.54431386881694,40.48279903872275],[-78.54045086709283,40.47639503741718],[-78.5440278680025,40.465958035305626],[-78.54846586857343,40.46186203453363],[-78.55772387005997,40.44157102974864],[-78.55289186812541,40.434791028572064],[-78.56095686688863,40.37503901743736],[-78.56146886590392,40.369678016236584],[-78.60223887848849,40.353637011301686],[-78.61809788110396,40.332107006903875],[-78.62038588139964,40.3270330055658],[-78.5730738658816,40.30886600389256],[-78.52969885141681,40.29287800250571],[-78.50570284321029,40.287316002850076],[-78.45727482539313,40.25066799702034],[-78.44789782239802,40.244402996218774],[-78.44279682204665,40.25961599963376],[-78.44246482246511,40.27619400303812],[-78.43429082206961,40.30230900836083],[-78.39310280812722,40.2842100064431],[-78.3239247841276,40.25731800410996],[-78.30671277899503,40.24814700318578],[-78.2887667729005,40.24211500279296],[-78.28400877222295,40.254538004804054],[-78.27406276930765,40.26671200770544],[-78.26765276833684,40.27792701013578],[-78.25985676729367,40.29458901406283],[-78.25730776700848,40.29789101437051],[-78.25009376505353,40.312299017253125],[-78.23812676322518,40.33031902187366],[-78.23092676168208,40.339850023432724],[-78.22458075927376,40.34666002543997],[-78.21641075784646,40.353627027422775],[-78.21203775653967,40.35947402792429],[-78.20546275575978,40.37271303155829],[-78.19145675216372,40.39109003502777],[-78.18628475183638,40.39988503690199],[-78.17794974921915,40.40865103904449],[-78.15941274576795,40.43380104505754],[-78.1554497446609,40.43855104617624],[-78.1342357405865,40.47325005333749],[-78.13008373931964,40.481998055085405],[-78.12945073921823,40.4891730562962],[-78.13174374105715,40.49683005824799],[-78.13563574267862,40.498222058439744],[-78.14890074520218,40.4876370552449],[-78.15337574690199,40.488566056078284],[-78.15362874829806,40.496955057279116],[-78.15047874832776,40.510310060152705],[-78.14924274872743,40.52531506313158],[-78.14733074867297,40.53325906433405],[-78.13994974672539,40.54619506738677],[-78.13936674708093,40.55060306857971],[-78.12864074481962,40.56796107227033],[-78.13616474764683,40.569179071745594],[-78.14099174832353,40.5570350690591],[-78.14513774941722,40.55388206871292],[-78.1451427491439,40.549085067882125],[-78.14988674988395,40.546053067188375],[-78.1514817500624,40.540719065935654],[-78.16355575407415,40.53611406446079],[-78.16643575414403,40.53143106363055],[-78.17174975573332,40.534423063576],[-78.17682075825331,40.534479063698555],[-78.17830975803871,40.53765706376213],[-78.18559776099255,40.543711064853994],[-78.18914776314863,40.55125106660049],[-78.19708576614333,40.55845206706207],[-78.17828276164289,40.58379407314838],[-78.17929776212351,40.59273307428086],[-78.18421476461782,40.59530307481825],[-78.17167776144392,40.61226507907872],[-78.1663737602815,40.61795608024486],[-78.16973476191338,40.62103308076622],[-78.17342976278614,40.62827308143811],[-78.17872476481948,40.62691708131587],[-78.18917476908324,40.63280008184583],[-78.1902987688787,40.63717608294883],[-78.19722177166639,40.63935908245599],[-78.19608477103013,40.642505083131994],[-78.19835877249135,40.64809808425194],[-78.2061547760642,40.6551360856882],[-78.21369777906946,40.6654120869762],[-78.22197278151593,40.674547088322086],[-78.21714378050994,40.682884090626146],[-78.20487377835155,40.69588209317121],[-78.19986777645026,40.69898009410814],[-78.19524577537,40.69730209381889],[-78.18258777211493,40.70590909606137],[-78.17004476836767,40.71260409788151],[-78.16241376526068,40.711704097828274],[-78.15539176415503,40.71449709895862],[-78.15586976388249,40.71775309931048],[-78.13907875910867,40.724283101822756],[-78.11652375307669,40.739135105435736],[-78.13183675797652,40.74302510495372],[-78.22173778581005,40.73938310124835],[-78.3400108224259,40.73354309473099],[-78.36062182975648,40.733189094202096],[-78.34867082451186,40.72345109278674]]]},properties:{geoid:”42013″,name:”Blair”,state_name:”Pennsylvania”,county_state_name:”Blair County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.84,”40_35k_diff”:131.83,”60_35k_diff”:131.84,”27_65k_diff”:0,”40_65k_diff”:70.18,”60_65k_diff”:666.38,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:453.88,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:435.11,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:435.11,”40_95k_eptc”:530.6,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.88,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:435.11,”40_65k_no_eptc”:530.6,”60_65k_no_eptc”:1126.8,”27_95k_no_eptc”:435.11,”40_95k_no_eptc”:530.6,”60_95k_no_eptc”:1126.8}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-79.39246207930748,39.72158585626474],[-79.31345905498803,39.7219868597818],[-79.22465602754257,39.721987862894196],[-79.12475299589197,39.72248986725859],[-79.08449898395264,39.72249086926323],[-79.04555097210438,39.722890870486594],[-78.99072295453817,39.72256887321269],[-78.85781791364644,39.72298787858473],[-78.80838989796224,39.72291888056413],[-78.80187389715375,39.734567883321596],[-78.79685389589977,39.74116088487316],[-78.77154389178642,39.7891918952561],[-78.76704389054147,39.795391896414074],[-78.75724388972587,39.82349190247021],[-78.75932789545871,39.90690091826365],[-78.75920189635322,39.91094891905726],[-78.76161990372174,40.0144989391608],[-78.76303990465644,40.01472893935994],[-78.76320890689055,40.057012947153254],[-78.75201890461105,40.07492495107886],[-78.73984990160419,40.069578951083],[-78.72115389846986,40.11186595948386],[-78.69867389465337,40.16145797025393],[-78.67695889187087,40.21121498099798],[-78.66141288822638,40.231111985560624],[-78.65830788788818,40.24324298753232],[-78.79340192938913,40.244194982236564],[-78.84804394688898,40.244908980538085],[-78.85317194848534,40.245730980158434],[-78.8600659503992,40.242906979505214],[-78.86494395184478,40.24470897923614],[-78.86866495392573,40.248890980398556],[-78.87984695655359,40.24723497962252],[-78.88467195851366,40.24458297829583],[-78.89087096108973,40.24975197959929],[-78.8925709617927,40.25780398069062],[-78.89716396312426,40.26373998149168],[-78.89440596335389,40.268496982463695],[-78.89623296394663,40.271595983611014],[-78.90205696592854,40.27479898378893],[-78.92479697322801,40.278495983242045],[-78.92711197417415,40.284740984606465],[-78.98176999112553,40.28544698263378],[-79.01585600160679,40.28542198059685],[-79.05605601496902,40.284868979579656],[-79.05664901402571,40.27861197839796],[-79.05938101497169,40.27577497725574],[-79.0679660168893,40.272478975942114],[-79.07352601854836,40.2667349754211],[-79.07664101879442,40.26031497399261],[-79.07957302021015,40.25793597302348],[-79.07925301892732,40.25117997154783],[-79.08247502068677,40.25008197155718],[-79.08617702029608,40.242672969922545],[-79.09491002323986,40.23649296868985],[-79.09594902262415,40.232617967116326],[-79.1001560246745,40.23115696723739],[-79.09867302399974,40.2261049664828],[-79.10300602384419,40.21823896468036],[-79.10793202507979,40.21303396345451],[-79.11428902724458,40.210265962367124],[-79.1162420273491,40.20376096142705],[-79.12194502850203,40.20314596055313],[-79.12570303009086,40.20070896031573],[-79.12381702937293,40.1939569584478],[-79.12965602980768,40.180931956170326],[-79.13439603153715,40.178729955075156],[-79.1433090337709,40.17989695508848],[-79.14106803336891,40.17306595413473],[-79.14070503260247,40.16331495218372],[-79.1497710344117,40.16038095101161],[-79.16092803779308,40.16114895089949],[-79.16275703831431,40.15406994976132],[-79.16212603728376,40.143317947230464],[-79.16582803846866,40.13869894650727],[-79.16762903767298,40.12879094408593],[-79.1719590393804,40.12635894375651],[-79.1742520396898,40.12061194244523],[-79.18099004077877,40.11572194174085],[-79.18522504179565,40.10985594033871],[-79.19216404407159,40.11027493987761],[-79.19687504667618,40.11595894046721],[-79.20519204883396,40.11656794071424],[-79.21077705042329,40.11891094101867],[-79.22086705320284,40.11274493937008],[-79.22262305287452,40.10417893790447],[-79.22667505392408,40.098257936140335],[-79.23662305742862,40.096548935595145],[-79.24301605859759,40.09227793441467],[-79.24640106016732,40.09371793466473],[-79.2561400624533,40.08834793325154],[-79.25867406309901,40.0802809317182],[-79.26439006479806,40.07867593057402],[-79.26774206516698,40.07427593020002],[-79.26716906500154,40.066017928155894],[-79.27135406505023,40.06424592773145],[-79.27876906752779,40.05554492541835],[-79.2781040672722,40.05048692473651],[-79.28431306797569,40.04825392397342],[-79.288581069585,40.041782922604355],[-79.29388707101101,40.04045392222007],[-79.29631907080211,40.03652192107962],[-79.3227890776591,40.003503913995395],[-79.33846908115393,39.9820219088788],[-79.3425880817683,39.982063908738425],[-79.34254108122461,39.97631090732568],[-79.35600808484716,39.95817190336642],[-79.3728870876466,39.93652989848831],[-79.37830608985512,39.936658898881085],[-79.37826108903936,39.93314289768538],[-79.38328509074937,39.92756789691918],[-79.38396009053513,39.9245018956375],[-79.39156509241452,39.91951189466576],[-79.3876270912946,39.91570389382406],[-79.39872109325314,39.90063589044688],[-79.41756109575286,39.85378388069058],[-79.40978509356115,39.84930588059328],[-79.3936610885191,39.843483879560324],[-79.38959208637696,39.83964387911965],[-79.38195908336648,39.83686887905596],[-79.3830530835697,39.83003487809566],[-79.38123608283031,39.826883877120245],[-79.37160407989684,39.82708387798636],[-79.36569807810359,39.82055387619753],[-79.36396007621067,39.80678487372099],[-79.36885207788872,39.80146587246365],[-79.36826007647173,39.7958848713639],[-79.36256007411096,39.78848487026316],[-79.35436007187484,39.78848487104336],[-79.35236007106755,39.784484869971095],[-79.35676007229527,39.78148486894222],[-79.37016007721381,39.785784869392046],[-79.3800610804747,39.790084870300944],[-79.38206108051497,39.783484868298565],[-79.38456108135463,39.78228486832248],[-79.39296108326423,39.784284868404455],[-79.3953610847812,39.78248486814664],[-79.39166108308216,39.77798486683315],[-79.38026107920099,39.773184866465634],[-79.37866107812599,39.76888486591183],[-79.38626108028407,39.76188486399204],[-79.39836108302302,39.7584848635625],[-79.39986108382226,39.7555848629296],[-79.393661081543,39.745684860830615],[-79.39406108164529,39.74328485996729],[-79.40436208462411,39.742984860087496],[-79.40886208596902,39.74108485895934],[-79.40996208575645,39.73498585781714],[-79.39266208025083,39.73268585863965],[-79.38946207840173,39.7270858571551],[-79.39246207930748,39.72158585626474]]]},properties:{geoid:”42111″,name:”Somerset”,state_name:”Pennsylvania”,county_state_name:”Somerset County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.84,”40_35k_diff”:131.83,”60_35k_diff”:131.84,”27_65k_diff”:0,”40_65k_diff”:70.18,”60_65k_diff”:666.38,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:453.88,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:435.11,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:435.11,”40_95k_eptc”:530.6,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.88,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:435.11,”40_65k_no_eptc”:530.6,”60_65k_no_eptc”:1126.8,”27_95k_no_eptc”:435.11,”40_95k_no_eptc”:530.6,”60_95k_no_eptc”:1126.8}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-74.46329258721104,40.599195217536355],[-74.45446458574371,40.603667219277916],[-74.45037258343311,40.60418121973225],[-74.44569258293463,40.60900922066803],[-74.43652657964941,40.610937221602136],[-74.43142457807575,40.615671222149274],[-74.42794757726692,40.61657622223414],[-74.42319857621501,40.621158223948186],[-74.4228165764474,40.62501122457517],[-74.41764757518759,40.627549224828684],[-74.41493557439942,40.63247822576574],[-74.41442157503477,40.6406602282759],[-74.4085625726736,40.644295228802754],[-74.4069875724962,40.65073423036836],[-74.40336157231842,40.65409623111949],[-74.40180157186245,40.66448923333982],[-74.40513157340209,40.66778223382017],[-74.41985757704778,40.65768323115216],[-74.42929358074134,40.66461823203853],[-74.43277458236567,40.66467123150512],[-74.44308558436371,40.657659230551054],[-74.45084758730562,40.654156229118556],[-74.46103659130726,40.67351223242889],[-74.47025459449036,40.66794023075136],[-74.48243659807537,40.6660372301888],[-74.48579759837425,40.66236822962071],[-74.4989346024209,40.661390228587265],[-74.50370160466942,40.65963822875094],[-74.50770260553153,40.652591226406955],[-74.51308960716372,40.64957122633674],[-74.52323060989471,40.64916522571007],[-74.5298556130833,40.66757522927131],[-74.52568761176606,40.6705772294457],[-74.52871461407071,40.67984523100143],[-74.52788061418282,40.68435223272437],[-74.52447861324889,40.68915023377396],[-74.51434761027502,40.694373234897625],[-74.51468361049226,40.70191723621677],[-74.51789761197517,40.70558123665563],[-74.52683361464075,40.71081723766246],[-74.52411961451564,40.71565123881593],[-74.5275206156779,40.716672239043234],[-74.53150661725381,40.72127523907397],[-74.52976761717048,40.72651324071807],[-74.53089461770857,40.72986224095669],[-74.54334062119653,40.73422324143567],[-74.54767762288512,40.73699524153267],[-74.54871262402042,40.74612724360043],[-74.55268162599599,40.7495202443318],[-74.55192762548167,40.75465924510146],[-74.55601962769774,40.758296245952316],[-74.72566767856841,40.719540232540545],[-74.72215367734796,40.71601323188041],[-74.72014167693796,40.706485229794104],[-74.7168876754346,40.704861229318404],[-74.71662867449986,40.69869522831437],[-74.7207326758628,40.69683822741376],[-74.72115767558896,40.69158422642268],[-74.72393967692054,40.68784522596548],[-74.71774567364683,40.683996225435365],[-74.72160767532286,40.67877922433831],[-74.72270267458964,40.67009822271951],[-74.73059567710861,40.66574522171679],[-74.72755367536811,40.658622220326855],[-74.71956967280735,40.65414521967777],[-74.72363567390788,40.64776821856984],[-74.7229526733929,40.63894021652095],[-74.72765967427723,40.636241215546136],[-74.72654567427173,40.63241821497707],[-74.71327866921601,40.63062421501885],[-74.71154666802964,40.625046213951535],[-74.7027046654971,40.62112521368044],[-74.71147766798609,40.611540211477376],[-74.7133016688128,40.61210521177697],[-74.72175367030871,40.600710208778736],[-74.7185836691315,40.5996642086056],[-74.72493867016476,40.58876320671274],[-74.7131516665838,40.58391120581298],[-74.72459866911538,40.56619220181551],[-74.730703671464,40.56359220095992],[-74.74266067436167,40.5539061987039],[-74.77598068151237,40.50361418786222],[-74.78139468326484,40.505009187735986],[-74.78721768548773,40.512001188978005],[-74.79784268920197,40.5155651894202],[-74.78042768214777,40.4841711842898],[-74.74814866781051,40.42416417347584],[-74.7349936616968,40.39905716858833],[-74.72206265604497,40.37521316475652],[-74.71816465549215,40.376787165527524],[-74.70080865045682,40.38065116619413],[-74.67450664209176,40.38429116847247],[-74.6539296358565,40.39105617001987],[-74.62252062569804,40.384304170300005],[-74.61759762336425,40.37727716911724],[-74.62024162405832,40.37375716810516],[-74.6129796221733,40.3757681688747],[-74.60256861852264,40.3807281697137],[-74.59530661632009,40.3863951714693],[-74.59184461583997,40.39203517266347],[-74.58771061470948,40.3944261736247],[-74.58581561454,40.40228017490524],[-74.5858656155255,40.41709317777247],[-74.57616561352799,40.42231217944389],[-74.55454760602055,40.430168181731254],[-74.5362496010755,40.43830818386931],[-74.52664859839821,40.44477518528026],[-74.52033959729114,40.451286186850496],[-74.50781559369666,40.460993189674035],[-74.49564159061063,40.468710191080945],[-74.48493858794997,40.47959919368629],[-74.47850058547242,40.483926195172224],[-74.46821058254174,40.486853195655584],[-74.4598645800126,40.49105419728154],[-74.45918058077837,40.496627197672986],[-74.46695358251117,40.502879198695936],[-74.46694858332496,40.50890620026073],[-74.48190358879121,40.512009200109446],[-74.48511658932976,40.51532520101447],[-74.49486359349068,40.528744203439345],[-74.51185459915877,40.53988820500149],[-74.5161446012846,40.545823205803764],[-74.5177926024325,40.55285820700314],[-74.52077360327705,40.55653620744896],[-74.52668660593052,40.55948220780804],[-74.52449360536859,40.561730208215806],[-74.52580560585064,40.56854920932885],[-74.51514760316778,40.58011821215553],[-74.50479459969456,40.586300213743755],[-74.49050059525594,40.58653421482725],[-74.48321959380227,40.5894412157503],[-74.47385959111789,40.59701621697514],[-74.46329258721104,40.599195217536355]]]},properties:{geoid:”34035″,name:”Somerset”,state_name:”New Jersey”,county_state_name:”Somerset County, New Jersey”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:84.32,”60_65k_diff”:696.41,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:483.91,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.05,”27_65k_eptc”:446.7,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:446.7,”40_95k_eptc”:544.74,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:446.7,”40_65k_no_eptc”:544.74,”60_65k_no_eptc”:1156.83,”27_95k_no_eptc”:446.7,”40_95k_no_eptc”:544.74,”60_95k_no_eptc”:1156.83}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-80.51935758882121,41.84957120958579],[-80.40817855455268,41.849472214241665],[-80.25059950495802,41.8494692210112],[-80.21109549339411,41.849048223462546],[-80.14649947216486,41.84904722594303],[-80.08764945429351,41.84985822926348],[-80.05397744442428,41.84986423031273],[-80.01109743001079,41.85020423244263],[-79.93633040671116,41.85039923597705],[-79.91592040115371,41.85068623697364],[-79.84414237868616,41.85085224005417],[-79.79855636398055,41.85111624196949],[-79.7620333526571,41.850918243463006],[-79.71084333602607,41.851462245736734],[-79.68035632719963,41.851532247255136],[-79.61207430600395,41.850336250515845],[-79.61197630760783,41.87506425491538],[-79.6114763074364,41.882964255958406],[-79.61065131666014,41.989545275512405],[-79.61084031702369,41.99876527778528],[-79.64984632964027,41.998912276025344],[-79.76195736469009,41.9988492710537],[-79.76185337555133,42.130513294919275],[-79.76173537708888,42.15529629974027],[-79.76193138224747,42.21917131127854],[-79.7618583858538,42.267554319611335],[-79.76257239504616,42.37506633918796],[-79.76232940107309,42.44534835236732],[-79.76259340595097,42.500066361882254],[-79.76242140690748,42.51608036474301],[-79.80512041848169,42.500051359946156],[-79.87478243817512,42.47303235211725],[-79.90009444544344,42.46340634964147],[-79.9997864744849,42.4249313381149],[-80.01854447917178,42.41797333523396],[-80.08022549728443,42.39417032886879],[-80.12479450962302,42.387196325408404],[-80.24980254744465,42.368424316240926],[-80.33122057261171,42.355879310003736],[-80.37480658497864,42.3497443066677],[-80.41548459809732,42.34319630379338],[-80.45997961147084,42.336473300136134],[-80.5198546290299,42.32714029642659],[-80.5198016218647,42.250066282068275],[-80.51946661824725,42.20405627366237],[-80.51964361496329,42.16040426566147],[-80.5197386075162,42.07455825010952],[-80.51932959920526,41.97247623202305],[-80.5192225945376,41.91928322219437],[-80.51935758882121,41.84957120958579]]]},properties:{geoid:”42049″,name:”Erie”,state_name:”Pennsylvania”,county_state_name:”Erie County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:26.92,”60_65k_diff”:574.51,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:362.01,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:399.63,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:399.63,”40_95k_eptc”:487.34,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.87,”27_65k_no_eptc”:399.63,”40_65k_no_eptc”:487.34,”60_65k_no_eptc”:1034.93,”27_95k_no_eptc”:399.63,”40_95k_no_eptc”:487.34,”60_95k_no_eptc”:1034.93}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-74.55310658464879,40.079138112480855],[-74.52869157466299,40.03745710435611],[-74.50637356446258,39.991233095911745],[-74.47151255034181,39.92493008414693],[-74.43422453428096,39.85516507145637],[-74.42941653124554,39.84541106955408],[-74.38970951486999,39.77329105705914],[-74.39036550689188,39.62980502852291],[-74.3904005044205,39.59604502085508],[-74.39230250518763,39.59456802050158],[-74.39760150667088,39.58152401825005],[-74.39767050578374,39.577794017416906],[-74.40082050665721,39.57225001642267],[-74.40516050847594,39.569601015739565],[-74.4103965094646,39.57102901578878],[-74.41883451262028,39.56859101471522],[-74.4143995101198,39.5609850137836],[-74.41739451131605,39.55726301275352],[-74.41584251034392,39.549458011287655],[-74.4104905081706,39.54786001132493],[-74.40168450551948,39.537930009423874],[-74.3807974956754,39.49854500228882],[-74.36096948995907,39.50203500303751],[-74.35501748799545,39.50537200410165],[-74.33858948313289,39.506863005287045],[-74.3263834796068,39.506340005073824],[-74.32195847755627,39.50515200494814],[-74.312613475217,39.50012500511119],[-74.2964624682573,39.47530000017337],[-74.23206344751436,39.475206002273495],[-74.21274344293751,39.50012500838835],[-74.21118144300003,39.50012500827279],[-74.18319043517623,39.53300201582552],[-74.12458142194352,39.615147034212285],[-74.096532414972,39.64995704259323],[-74.08331741116994,39.66957004678064],[-74.07068940929703,39.69126105105782],[-74.06219640724505,39.70704305494874],[-74.04949040428833,39.7237930587807],[-74.03815940153716,39.75012806474431],[-74.0330804014125,39.770027068787996],[-74.02766140204142,39.80651207605072],[-74.02478640280182,39.82959408040488],[-74.02233740325678,39.85576908571738],[-74.01990040373606,39.87512709001503],[-73.99957840255352,39.976806110700984],[-73.98918140109795,40.013332118707666],[-73.98603040131754,40.02113412044687],[-73.97329239977465,40.07515013136195],[-73.96614639827887,40.090585135207604],[-73.96541539917973,40.097650136383805],[-74.00718041251822,40.097723134784786],[-74.02788141876022,40.09922313457983],[-74.03864442212284,40.104464135404704],[-74.04412242431913,40.10534113550313],[-74.05578442849924,40.10106813428668],[-74.05679442760382,40.097871133323615],[-74.0614914292183,40.09603613266464],[-74.07025243150562,40.089414131104576],[-74.07237443217763,40.08938913091888],[-74.08385143667631,40.0958511315726],[-74.09422344104658,40.10751713360448],[-74.09406244090142,40.11501313534026],[-74.09904044352587,40.12778913743613],[-74.10333544484098,40.13126913786761],[-74.10334644511276,40.13442013843278],[-74.10780544667678,40.13692613882058],[-74.15031645747145,40.0988851299434],[-74.15440545981605,40.09972713039913],[-74.15876146083968,40.105997131048916],[-74.17412146570284,40.10835213090684],[-74.17933546834253,40.1109711315366],[-74.19196047167762,40.111082131014484],[-74.20388947529665,40.112558131179064],[-74.20916147706713,40.110622130561545],[-74.2306354839468,40.1095691291913],[-74.23960548734662,40.1123911297909],[-74.24458348919167,40.118148130544235],[-74.2422084887361,40.12406413232445],[-74.24183448898114,40.13096713370128],[-74.24668549127415,40.13641913467811],[-74.25010149184604,40.144186135548175],[-74.25322849366782,40.147476136095165],[-74.25984249601413,40.149174136266744],[-74.26020649665621,40.15671213744617],[-74.25820849571615,40.16011813901614],[-74.26145649742674,40.16704113942541],[-74.4067115444824,40.172410135742794],[-74.46563456018981,40.13119712559035],[-74.52732457756301,40.09028411569992],[-74.55310658464879,40.079138112480855]]]},properties:{geoid:”34029″,name:”Ocean”,state_name:”New Jersey”,county_state_name:”Ocean County, New Jersey”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:84.32,”60_65k_diff”:696.41,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:483.91,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.05,”27_65k_eptc”:446.7,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:446.7,”40_95k_eptc”:544.74,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:446.7,”40_65k_no_eptc”:544.74,”60_65k_no_eptc”:1156.83,”27_95k_no_eptc”:446.7,”40_95k_no_eptc”:544.74,”60_95k_no_eptc”:1156.83}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-79.39246207930748,39.72158585626474],[-79.38946207840173,39.7270858571551],[-79.39266208025083,39.73268585863965],[-79.40996208575645,39.73498585781714],[-79.40886208596902,39.74108485895934],[-79.40436208462411,39.742984860087496],[-79.39406108164529,39.74328485996729],[-79.393661081543,39.745684860830615],[-79.39986108382226,39.7555848629296],[-79.39836108302302,39.7584848635625],[-79.38626108028407,39.76188486399204],[-79.37866107812599,39.76888486591183],[-79.38026107920099,39.773184866465634],[-79.39166108308216,39.77798486683315],[-79.3953610847812,39.78248486814664],[-79.39296108326423,39.784284868404455],[-79.38456108135463,39.78228486832248],[-79.38206108051497,39.783484868298565],[-79.3800610804747,39.790084870300944],[-79.37016007721381,39.785784869392046],[-79.35676007229527,39.78148486894222],[-79.35236007106755,39.784484869971095],[-79.35436007187484,39.78848487104336],[-79.36256007411096,39.78848487026316],[-79.36826007647173,39.7958848713639],[-79.36885207788872,39.80146587246365],[-79.36396007621067,39.80678487372099],[-79.36569807810359,39.82055387619753],[-79.37160407989684,39.82708387798636],[-79.38123608283031,39.826883877120245],[-79.3830530835697,39.83003487809566],[-79.38195908336648,39.83686887905596],[-79.38959208637696,39.83964387911965],[-79.3936610885191,39.843483879560324],[-79.40978509356115,39.84930588059328],[-79.41756109575286,39.85378388069058],[-79.39872109325314,39.90063589044688],[-79.3876270912946,39.91570389382406],[-79.39156509241452,39.91951189466576],[-79.38396009053513,39.9245018956375],[-79.38328509074937,39.92756789691918],[-79.37826108903936,39.93314289768538],[-79.37830608985512,39.936658898881085],[-79.3728870876466,39.93652989848831],[-79.35600808484716,39.95817190336642],[-79.34254108122461,39.97631090732568],[-79.3425880817683,39.982063908738425],[-79.33846908115393,39.9820219088788],[-79.3227890776591,40.003503913995395],[-79.29631907080211,40.03652192107962],[-79.29388707101101,40.04045392222007],[-79.30979407650007,40.04355792252656],[-79.31609307857516,40.043847921564875],[-79.32368308055966,40.04078792135635],[-79.33864308487766,40.04215792051712],[-79.34268308660361,40.044177921255034],[-79.34445308717974,40.05089792171611],[-79.35124409066741,40.06787692516915],[-79.35563009240325,40.07436692656493],[-79.36746609676854,40.080205926862284],[-79.37252309827056,40.08137792676673],[-79.39371510512557,40.090904928109985],[-79.40131310823445,40.102237929613125],[-79.41539311302476,40.10460792928371],[-79.42347711624369,40.11116393006859],[-79.43756312082326,40.11586793072718],[-79.44213312249694,40.11957793145865],[-79.4477231251544,40.12677793251597],[-79.44748112523219,40.133240933484515],[-79.46122813013828,40.14135693479744],[-79.46152513054584,40.1441059351543],[-79.48313913679824,40.14405093444976],[-79.48852313818433,40.14122793394874],[-79.49667614078182,40.14176793311351],[-79.50519114343935,40.14057593263982],[-79.51786714622048,40.13138593036589],[-79.52698014901914,40.123244928143286],[-79.53086815084008,40.128215928910436],[-79.53399415206619,40.12862492912989],[-79.54107415269266,40.12082192694943],[-79.54128715221165,40.11275292546392],[-79.548522155129,40.110329924624835],[-79.55315315681067,40.11258592549834],[-79.5591201575252,40.111164924365326],[-79.56097115782171,40.106615923580925],[-79.57892316345689,40.10523392253738],[-79.58538016509608,40.10213292210016],[-79.5845791646043,40.0978419215618],[-79.59202916644973,40.09346791985665],[-79.5930241663159,40.08206291777488],[-79.60044516937286,40.08431591766788],[-79.60367717031981,40.09084691878872],[-79.61309917317016,40.0934459188834],[-79.62585617773748,40.09194091823547],[-79.62700117767884,40.08843191727463],[-79.63570018051425,40.08591291675647],[-79.63899718073574,40.08286691576629],[-79.64812518383626,40.087650916485806],[-79.65408618628521,40.08930191607557],[-79.6542881867326,40.0936409170649],[-79.65725718720635,40.09660291799354],[-79.6638691893271,40.096739917182724],[-79.66860519143302,40.09885491781738],[-79.66619019042454,40.10266391881818],[-79.67175419305273,40.106254918825634],[-79.68379719592409,40.10862791862553],[-79.68463719747047,40.11312191988476],[-79.69165819929488,40.113097919318214],[-79.70540220253187,40.107645917587],[-79.71127020489126,40.108665917712315],[-79.72180820847878,40.11529491828639],[-79.71850220735102,40.1169289189523],[-79.72336221018922,40.1223459199981],[-79.72760321095039,40.120615919460484],[-79.73485421301876,40.121053919308366],[-79.74117721565287,40.12627891982038],[-79.74605921687834,40.12846492053191],[-79.78220322800543,40.128427918784176],[-79.8038202345187,40.128768917955085],[-79.81004323752282,40.132487918187564],[-79.8165972395909,40.132798918319445],[-79.81611623903643,40.12838291687774],[-79.83941224578012,40.128258916267576],[-79.85360625036208,40.12753891505686],[-79.8690132545554,40.12801791499756],[-79.87529925723166,40.129537915032245],[-79.87786725799504,40.12696691393126],[-79.86005925159309,40.11884791379447],[-79.85253924929364,40.116111913011025],[-79.84913124828374,40.112623913048054],[-79.84338624557182,40.09969691079568],[-79.83927424273114,40.09248090901519],[-79.84261824355957,40.08379290739508],[-79.84937024569135,40.07955290596181],[-79.86245924893684,40.075664905087955],[-79.87156325174632,40.075456904259475],[-79.87974025424373,40.07870490461078],[-79.89439625929072,40.080272904550206],[-79.8995482606175,40.078448904117494],[-79.90153326128058,40.073600903107135],[-79.89615625893872,40.07048090234184],[-79.88511625548477,40.068560902513056],[-79.87894025346634,40.06304090169241],[-79.88110025348597,40.05780890113873],[-79.89161225594476,40.04942489863767],[-79.89046025580107,40.04536089797441],[-79.87868325146773,40.03822589692225],[-79.87621925054127,40.03376189687175],[-79.87999525151766,40.028289895118036],[-79.8899572543248,40.02246989397173],[-79.904326257932,40.022540892822796],[-79.91432326150776,40.021044892559985],[-79.92484726390845,40.01613189077043],[-79.92978926549868,40.011752889499896],[-79.93452626601346,39.99963388734829],[-79.94673526955285,39.99425788585087],[-79.95462327194544,39.99528188568038],[-79.95902327321177,40.000033886462106],[-79.9632012752982,40.00797488806528],[-79.97141027847151,40.013817888658764],[-79.98517028261257,40.0131088877038],[-79.9935692851997,40.00913688665363],[-79.99572928518226,40.00510488598127],[-79.99430528460212,39.99721688409872],[-79.99089728275648,39.986561882093085],[-79.99801728452181,39.98332988111519],[-80.00585828673277,39.98020988016414],[-80.00913828783145,39.97715387951456],[-80.01073828808586,39.9711538788762],[-80.00934728604254,39.958801876511714],[-79.99881928250949,39.95089787532447],[-79.99371428084116,39.949393874827464],[-79.97424127482776,39.955121876981956],[-79.96513727253998,39.95515387777972],[-79.95724926979697,39.95328187706338],[-79.94766426687883,39.94734687672413],[-79.94272026470819,39.94297887635991],[-79.9350562610185,39.93360287450329],[-79.92560025757369,39.92480287318289],[-79.92332825688246,39.91774687194799],[-79.92960125812098,39.90774686984449],[-79.92843325728248,39.90229086890017],[-79.91528125147357,39.88030786546687],[-79.91685025133094,39.87661186416449],[-79.92767825520511,39.87198386295578],[-79.93067925530599,39.868083862310826],[-79.92478025320611,39.858790860774064],[-79.92465325296637,39.85506385971221],[-79.93798025613295,39.84668385740793],[-79.9364802558998,39.841683856640365],[-79.92437925155336,39.8381838565219],[-79.92171925000478,39.831331855175804],[-79.92118024917646,39.815684852776435],[-79.92017124862501,39.81228585206009],[-79.91018024418143,39.79958484976826],[-79.90858024354105,39.793484848396915],[-79.9139812448323,39.78798484767768],[-79.92929424866358,39.78628584631799],[-79.93441425058286,39.781284844773474],[-79.93298224935882,39.771484842919136],[-79.93468324884887,39.764684842405245],[-79.9300832469168,39.75708584045004],[-79.92248324475104,39.753484840665756],[-79.91438224249089,39.75218484016307],[-79.90718223949258,39.74748584013832],[-79.90368223795308,39.74348583886292],[-79.90350923820215,39.73926683834142],[-79.9061772380032,39.7334018374001],[-79.91628324083872,39.720784834208565],[-79.87478222800067,39.72068583577637],[-79.74972818899204,39.72078484165749],[-79.69167417127537,39.72098484326155],[-79.66737316364386,39.720784844773874],[-79.58386913784214,39.72128484817357],[-79.54846812742912,39.72078584962353],[-79.47666510525514,39.72108585222835],[-79.41546308615573,39.72158585569896],[-79.39246207930748,39.72158585626474]]]},properties:{geoid:”42051″,name:”Fayette”,state_name:”Pennsylvania”,county_state_name:”Fayette County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.84,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:59.62,”60_65k_diff”:643.96,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:431.46,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:426.45,”40_65k_eptc”:460.42,”60_65k_eptc”:460.41,”27_95k_eptc”:426.45,”40_95k_eptc”:520.04,”60_95k_eptc”:672.91,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.88,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.87,”27_65k_no_eptc”:426.45,”40_65k_no_eptc”:520.04,”60_65k_no_eptc”:1104.37,”27_95k_no_eptc”:426.45,”40_95k_no_eptc”:520.04,”60_95k_no_eptc”:1104.37}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-77.67176358289021,40.2898330364985],[-77.65487657898359,40.30684804039718],[-77.6361415738504,40.322382044360126],[-77.61366156770639,40.3376810485007],[-77.59943056360483,40.34815505050505],[-77.5827965592795,40.35704905349398],[-77.5656675552933,40.3673710558219],[-77.54061654705615,40.375568058110765],[-77.53226754543513,40.376014058930906],[-77.54014354862666,40.39922906288065],[-77.51708754203912,40.41161606668161],[-77.5090245408102,40.41515206770013],[-77.50064553794873,40.420344068364464],[-77.47142252957264,40.43492107294298],[-77.44589052270803,40.44716807616138],[-77.43653952019184,40.45056207671989],[-77.42902951731605,40.45447607793624],[-77.41343551332824,40.46059708028628],[-77.33811249177337,40.49534408947147],[-77.28959447877499,40.51846509557818],[-77.2806064757342,40.520115096848585],[-77.26816647226188,40.52609109854339],[-77.23169846174866,40.53849210250056],[-77.21645945695374,40.544425103634005],[-77.19846445232753,40.5522951057403],[-77.1829524475627,40.55670410788595],[-77.17378144441929,40.557509107949876],[-77.16756344293289,40.559517108540604],[-77.18293244862386,40.58214811214435],[-77.1634554436564,40.58691511412517],[-77.15913744200417,40.586575114370426],[-77.12806143208249,40.59083411614441],[-77.11892543000536,40.59265811714347],[-77.10679242529616,40.59279811716466],[-77.10331642451855,40.595913118421585],[-77.08729441974072,40.598060119038585],[-77.0699934145328,40.59847212026317],[-77.04727140820279,40.60253112164654],[-77.04195640573404,40.60423112265713],[-77.03297640317042,40.603454122875675],[-77.02330640031748,40.60426812268404],[-77.0001103935426,40.61092312484658],[-76.98765239004382,40.61619812698259],[-76.95607938104474,40.62794613012942],[-76.9491503790798,40.62817513019318],[-76.93988537592816,40.638150133375355],[-76.9406583769769,40.646183134553795],[-76.9452233791158,40.65034113532396],[-76.96181638414971,40.64568213341827],[-76.96546338477303,40.64722013395909],[-76.96860238560117,40.64123113218729],[-76.97644238829824,40.643077132675785],[-76.97658338859574,40.64538213305072],[-76.98804639182005,40.64359913212339],[-76.99755139398188,40.63588613057034],[-77.00313339615921,40.63872513040861],[-77.00605639805518,40.64262313159293],[-77.00404739649554,40.64558013149567],[-77.0079013985805,40.65194113265318],[-77.00842039977319,40.65992013482245],[-77.01379440117437,40.662172134647285],[-77.01915240261172,40.65950813410491],[-77.02251640440937,40.66089413375927],[-77.02575540496463,40.65607113266371],[-77.02950340624483,40.65557013317452],[-77.03441140759656,40.659936133373364],[-77.03242140704583,40.66468013458357],[-77.03544440805982,40.66852413539191],[-77.03555140961416,40.676926136755135],[-77.03934141071441,40.679966136817534],[-77.04577141270036,40.675645135891685],[-77.05328341456253,40.67519913543562],[-77.06580341914415,40.678285135886334],[-77.06808541984108,40.679848135599784],[-77.09360942723572,40.676129134179405],[-77.09732942919749,40.678373134656105],[-77.09745242864616,40.68209013505291],[-77.10152243117815,40.68898713647085],[-77.1095994336048,40.69158613651165],[-77.1250554384698,40.68580613481427],[-77.13984644280598,40.683592133772514],[-77.14909144546566,40.680546132557566],[-77.1505184452931,40.67708213195915],[-77.17132545249125,40.67906613172311],[-77.24101247417678,40.68766713103992],[-77.28794348934467,40.693603130207315],[-77.32305550016926,40.68309012648467],[-77.34430750675853,40.67550712372016],[-77.35596850935481,40.671989122737145],[-77.3636495114366,40.668730122171105],[-77.38379851769069,40.66175912014018],[-77.40718752478284,40.65232511764637],[-77.41873952808731,40.646510115586985],[-77.4257285295593,40.64411411468895],[-77.45203753768124,40.63282011179737],[-77.48915954800624,40.61523210634189],[-77.49776255036117,40.609492105212006],[-77.49750854805308,40.5817480998904],[-77.51273755168565,40.57307109781845],[-77.51563255288909,40.56957709722333],[-77.53245855763616,40.55948409386596],[-77.55961556442844,40.54502609051172],[-77.57404856961388,40.537802088826496],[-77.58862357348951,40.529272086208515],[-77.61251157976373,40.51419508204764],[-77.61246157743913,40.49092707815517],[-77.62596058125338,40.4829640754762],[-77.64599958671194,40.46838907172854],[-77.69021559802894,40.43250306383305],[-77.71074760372396,40.417601059587355],[-77.72346760671326,40.407297057578475],[-77.73820361104474,40.393318053578405],[-77.75212261355418,40.378553050380475],[-77.72803560314902,40.3230170402864],[-77.72287260038242,40.31009303858331],[-77.70303259060022,40.263584030526815],[-77.69895659000045,40.26578303116388],[-77.68516558627832,40.27631203344521],[-77.67586258394333,40.284707035256375],[-77.67176358289021,40.2898330364985]]]},properties:{geoid:”42067″,name:”Juniata”,state_name:”Pennsylvania”,county_state_name:”Juniata County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:273.99999999999994,”40_65k_diff”:435.17,”60_65k_diff”:1441.49,”27_95k_diff”:61.5,”40_95k_diff”:222.67,”60_95k_diff”:1228.99,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.41,”40_65k_eptc”:460.42,”60_65k_eptc”:460.41,”27_95k_eptc”:672.91,”40_95k_eptc”:672.92,”60_95k_eptc”:672.91,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.87,”27_65k_no_eptc”:734.41,”40_65k_no_eptc”:895.59,”60_65k_no_eptc”:1901.9,”27_95k_no_eptc”:734.41,”40_95k_no_eptc”:895.59,”60_95k_no_eptc”:1901.9}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-77.36418252459318,40.846945156150674],[-77.37471052717227,40.84530315545199],[-77.40730353759903,40.83528215201964],[-77.43903554672366,40.82381814862581],[-77.5110985666112,40.793962140652575],[-77.55253957851517,40.77759913551319],[-77.571940584346,40.76934113325809],[-77.59335759082552,40.761255130312435],[-77.62472160017668,40.75226912750416],[-77.65257660827459,40.74492912475487],[-77.66199061025557,40.73775012381599],[-77.68133661652679,40.72976612072839],[-77.67661361376456,40.71646011881961],[-77.70117262026696,40.70499011527374],[-77.69924161947283,40.69807311421041],[-77.70306862000356,40.692688113482],[-77.70835862188252,40.69049611259584],[-77.70378961915952,40.679944110603294],[-77.68534861443713,40.68491211200554],[-77.68271061319967,40.68272511199345],[-77.68708261414284,40.67675811091547],[-77.69061661498004,40.67504411018312],[-77.71084862074129,40.66201110717509],[-77.72073962376942,40.65797610587452],[-77.72043662316126,40.65458310527255],[-77.72819562505425,40.64858110359965],[-77.73514462647765,40.64474910220825],[-77.75162263126295,40.632308099915484],[-77.77248263771047,40.62594009738668],[-77.77985563950527,40.61966309628395],[-77.80133164430214,40.59957709139475],[-77.82160264955603,40.5789390867924],[-77.83254765208204,40.562542083050296],[-77.84182965355728,40.550043080330354],[-77.81651564258924,40.50008207178505],[-77.82824764577049,40.491566069226224],[-77.83587664804912,40.48424006775693],[-77.84413964976763,40.473455064871104],[-77.8701846559134,40.44525205826264],[-77.88874866068146,40.42866805456112],[-77.89637166223348,40.417786052769195],[-77.90805266545776,40.414026051116565],[-77.91241866622447,40.40818405024377],[-77.91384666614724,40.398687047724465],[-77.88911865885476,40.398973049417194],[-77.88771965793329,40.391366047127974],[-77.87770365404897,40.39355804865823],[-77.8702916519685,40.39226904848433],[-77.87256065206438,40.3812040458871],[-77.86519764907295,40.37153804499146],[-77.86120564777092,40.36985004480858],[-77.85691664622341,40.365236043778935],[-77.85290864523755,40.36479804402079],[-77.84522364202611,40.36877404459401],[-77.8383456405973,40.36903804556221],[-77.82983963684111,40.3639030443259],[-77.8186386330786,40.360550044170594],[-77.81470063220071,40.36249704531306],[-77.8103956319097,40.368599046522775],[-77.76174261646611,40.3687380482683],[-77.75212261355418,40.378553050380475],[-77.73820361104474,40.393318053578405],[-77.72346760671326,40.407297057578475],[-77.71074760372396,40.417601059587355],[-77.69021559802894,40.43250306383305],[-77.64599958671194,40.46838907172854],[-77.62596058125338,40.4829640754762],[-77.61246157743913,40.49092707815517],[-77.61251157976373,40.51419508204764],[-77.58862357348951,40.529272086208515],[-77.57404856961388,40.537802088826496],[-77.55961556442844,40.54502609051172],[-77.53245855763616,40.55948409386596],[-77.51563255288909,40.56957709722333],[-77.51273755168565,40.57307109781845],[-77.49750854805308,40.5817480998904],[-77.49776255036117,40.609492105212006],[-77.48915954800624,40.61523210634189],[-77.45203753768124,40.63282011179737],[-77.4257285295593,40.64411411468895],[-77.41873952808731,40.646510115586985],[-77.40718752478284,40.65232511764637],[-77.38379851769069,40.66175912014018],[-77.3636495114366,40.668730122171105],[-77.35596850935481,40.671989122737145],[-77.34430750675853,40.67550712372016],[-77.32305550016926,40.68309012648467],[-77.28794348934467,40.693603130207315],[-77.35409951060336,40.70167512903524],[-77.3553295149466,40.759422140162386],[-77.35663051877414,40.80734214893679],[-77.35711552238749,40.84449215633549],[-77.36418252459318,40.846945156150674]]]},properties:{geoid:”42087″,name:”Mifflin”,state_name:”Pennsylvania”,county_state_name:”Mifflin County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.84,”27_65k_diff”:188.06,”40_65k_diff”:330.38,”60_65k_diff”:1218.95,”27_95k_diff”:0,”40_95k_diff”:117.88,”60_95k_diff”:1006.45,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.42,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:648.48,”40_95k_eptc”:672.92,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:648.48,”40_65k_no_eptc”:790.8,”60_65k_no_eptc”:1679.37,”27_95k_no_eptc”:648.48,”40_95k_no_eptc”:790.8,”60_95k_no_eptc”:1679.37}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-75.06185571524799,39.568753991917795],[-75.0662877163405,39.56048299075506],[-75.06666271638964,39.556233989903454],[-75.06987271781922,39.55312698892462],[-75.0744587183984,39.54457198739878],[-75.0710487164748,39.53995498614558],[-75.072642716717,39.53608298570493],[-75.07106471698533,39.53245298483842],[-75.07339871706655,39.5267249830734],[-75.0729187160629,39.52189798260942],[-75.07560571737599,39.51894398192614],[-75.07801671745723,39.511991979976905],[-75.07664371702327,39.50783297971828],[-75.07970071712356,39.501441978287],[-75.07837871719137,39.49698197713924],[-75.07407471524805,39.49282197672948],[-75.07542271539064,39.489740975995595],[-75.07335871503761,39.485589975514664],[-75.08035371563736,39.47203097212806],[-75.08179771647737,39.46548597100651],[-75.08085671544764,39.46094996984875],[-75.0838247166219,39.45736196879124],[-75.11278372609075,39.47677897248179],[-75.17791774936916,39.52106897867374],[-75.23843577088746,39.5590469839632],[-75.27044477937487,39.53090697715936],[-75.29391178587264,39.511559972802175],[-75.30508978890867,39.503444970249646],[-75.31802179159821,39.49204796782877],[-75.32609079405005,39.48850196722084],[-75.34237779931935,39.490629966616254],[-75.34394380028814,39.48573396588813],[-75.34990980093355,39.47987296407758],[-75.35104180115152,39.47213396269229],[-75.35703180270721,39.47029496200122],[-75.36303980496604,39.46451496094963],[-75.36821480634282,39.456486958916386],[-75.37309880715968,39.45578695887467],[-75.38656481154798,39.45784495813857],[-75.40063681675707,39.4621729586733],[-75.40767981821888,39.458788957748894],[-75.41469281974511,39.45226695677514],[-75.41027481807343,39.45002295642606],[-75.41157081930687,39.445445955045194],[-75.40921381797203,39.44306495479705],[-75.4159888190614,39.43437195252799],[-75.41767982027154,39.42970095177506],[-75.41369081897062,39.42903695194116],[-75.41173381749634,39.42367595075478],[-75.41830581867846,39.41545294896932],[-75.41891281931349,39.41042494752174],[-75.41167681604338,39.40546094718746],[-75.40976881561261,39.40870994823517],[-75.4053558145679,39.40764394784405],[-75.40668381456665,39.40363894646735],[-75.41116381656146,39.40110094590427],[-75.40737381490115,39.39803994538624],[-75.40936281556448,39.3949209454089],[-75.4168668171022,39.3958699447437],[-75.41728981687798,39.38867894391539],[-75.41405781627803,39.38466094260306],[-75.40891281485129,39.38756994316727],[-75.40668681323933,39.380302941889504],[-75.41288581541893,39.37512094062556],[-75.44475282394303,39.35509693585271],[-75.40182180761906,39.31829392995851],[-75.38113180042014,39.30085292743444],[-75.32102277923687,39.25138691881281],[-75.30052277053011,39.2252819146801],[-75.2490187503392,39.15895290296737],[-75.2190767390366,39.115954895513305],[-75.19167272758422,39.079007889209926],[-75.1684637190217,39.056186884986495],[-75.12472170651874,39.07647889107959],[-74.99962167067649,39.135781907534245],[-74.91569064692558,39.17576291780569],[-74.91219364619586,39.17864591904525],[-74.9157706474631,39.184603919826976],[-74.91412464646163,39.18839592114929],[-74.92090864859752,39.18803492098029],[-74.92196464928783,39.19222392173932],[-74.91846064823692,39.19470992223265],[-74.92608765112666,39.19708392238118],[-74.9257286516041,39.20130292304979],[-74.92228465072232,39.20492592369571],[-74.92539265200787,39.21256792537596],[-74.92278665136025,39.22377192808981],[-74.91282464836513,39.22697292872178],[-74.89638564361765,39.23506193077418],[-74.88214764323477,39.30839794583511],[-74.87374364178332,39.312608947118264],[-74.86824463943002,39.318071948779696],[-74.86460963881238,39.32438095041539],[-74.86129563853414,39.32382295004194],[-74.86415463929455,39.3283869505865],[-74.86491263998454,39.338886953247076],[-74.85924263949073,39.35904195746576],[-74.85865863946319,39.36439795866852],[-74.8534126383723,39.3723319603169],[-74.85199063871077,39.38375296259509],[-74.85821664084366,39.395555964473274],[-74.85729164189891,39.403019966529484],[-74.85304964001824,39.40925796753697],[-74.85311164094395,39.41554296897151],[-74.85740964267801,39.42327697012026],[-74.85597964203453,39.42424597048552],[-74.87227964757855,39.43615697192355],[-74.89678965683005,39.45267197495812],[-74.98527268889309,39.51497498419964],[-75.06185571524799,39.568753991917795]]]},properties:{geoid:”34011″,name:”Cumberland”,state_name:”New Jersey”,county_state_name:”Cumberland County, New Jersey”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:84.32,”60_65k_diff”:696.41,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:483.91,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.05,”27_65k_eptc”:446.7,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:446.7,”40_95k_eptc”:544.74,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:446.7,”40_65k_no_eptc”:544.74,”60_65k_no_eptc”:1156.83,”27_95k_no_eptc”:446.7,”40_95k_no_eptc”:544.74,”60_95k_no_eptc”:1156.83}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-74.27197654530337,40.897329283329285],[-74.27219654590192,40.90527628494515],[-74.26713454370076,40.91066528606854],[-74.27168254599948,40.91543328651418],[-74.28263854931188,40.9168882862031],[-74.28374955057718,40.92068228736764],[-74.28851255241105,40.924841287783025],[-74.28924755262216,40.928799288171234],[-74.28510555169554,40.931386288913934],[-74.27942254967266,40.94332729204774],[-74.27723854984599,40.954603293663595],[-74.28055955204819,40.958003294721344],[-74.27930355182141,40.96495129559787],[-74.2823085528522,40.96952029691502],[-74.27886655261689,40.975478298305966],[-74.28168955268288,40.97996929856715],[-74.29717655832185,40.97945129778255],[-74.29751455799489,40.98349229878661],[-74.29283455725724,40.98796329980215],[-74.29555355871817,40.994711300808646],[-74.30168656038197,40.999181302228],[-74.30949556290537,40.998417301609535],[-74.31555556569144,41.00237730229369],[-74.32822456931527,41.00116830132492],[-74.33468957201204,41.00362130138281],[-74.33579657223414,41.00728330230856],[-74.3419935743631,41.00693630226199],[-74.34954557646888,41.00399230101207],[-74.35243857736535,41.005710300857174],[-74.3512785776489,41.01068430235209],[-74.35509457886927,41.01378030272207],[-74.3627375811382,41.013504302575235],[-74.37126858355266,41.01132730193816],[-74.37673758533543,41.013869301847414],[-74.38938159008593,41.01231430155122],[-74.39129559085713,41.01597230225531],[-74.3998285934979,41.01734330148536],[-74.40620559557632,41.02418430255215],[-74.4153795992669,41.02801930295739],[-74.4236876019497,41.02762330339836],[-74.4281546029461,41.02068130139954],[-74.43504160495253,41.020029301108664],[-74.43253660467857,41.02636930241955],[-74.42769160283599,41.03189930407948],[-74.42821460428712,41.03743430483338],[-74.43252460485337,41.03784430470984],[-74.44048960787055,41.043861305061796],[-74.44187860879185,41.05031930694275],[-74.44701861138347,41.05443730718735],[-74.45641461331398,41.05201230685324],[-74.46122061469661,41.05204030671938],[-74.4683516177368,41.04828730578958],[-74.47588361984869,41.0479043051947],[-74.48493862282679,41.04286230409816],[-74.48738162288731,41.03930330292649],[-74.49939762599143,41.035575301616596],[-74.50169362807273,41.04210630325029],[-74.49863762706845,41.04840330451543],[-74.49569962652133,41.05997030672986],[-74.48790262463002,41.06527530824578],[-74.48907262501365,41.071917308977966],[-74.48683662498557,41.07645331057242],[-74.50321363138539,41.08588131128435],[-74.52194163643034,41.070742307475875],[-74.54711064262524,41.04859630285594],[-74.60634565878523,40.99837929076163],[-74.63237966534106,40.97372528474556],[-74.63327266561781,40.97103128426349],[-74.64156166753405,40.96220728245534],[-74.64135466706112,40.9593962814614],[-74.63641366548478,40.954028280706005],[-74.63487966387805,40.949666279944964],[-74.63689866459042,40.94174927832542],[-74.64158266526279,40.93365527648278],[-74.65034566776936,40.93139027650897],[-74.65403766870081,40.926650274864485],[-74.65161066794822,40.92305727421596],[-74.65832167038756,40.91809227313653],[-74.66531167234787,40.917482272936326],[-74.6699346739208,40.91394727163545],[-74.67949867614766,40.909164270804055],[-74.6861056781489,40.91000427060703],[-74.68953367942677,40.90733026982029],[-74.69687668197041,40.90743127009911],[-74.7034806838432,40.90171326809056],[-74.71151868569376,40.89917626765361],[-74.71425868683734,40.90128826810535],[-74.71261668668765,40.90742226935539],[-74.71816868912747,40.91229926979687],[-74.72871869215855,40.916485269963275],[-74.73192969365786,40.920860271184715],[-74.7375426956782,40.91892527031376],[-74.74758469825223,40.919989270458096],[-74.75553570124255,40.91365726918971],[-74.76606070404603,40.91274226852151],[-74.7694267048059,40.91094226777644],[-74.7760577070333,40.90535126605363],[-74.79030271025157,40.89642926422812],[-74.7916537107166,40.890676262683165],[-74.80383371458954,40.88578126198958],[-74.80741871559444,40.88155726041217],[-74.80573971396227,40.8742042593735],[-74.80826971474272,40.86943325832018],[-74.80194371210122,40.86390625770305],[-74.80370171221354,40.86106925648235],[-74.80924271418664,40.860215256339764],[-74.80995271416236,40.85448725573819],[-74.8141167151969,40.85123125488684],[-74.82159171756724,40.84917325348345],[-74.82373771779524,40.84363125289475],[-74.8196937168444,40.84094825192094],[-74.81905171610374,40.83605425166994],[-74.82761071813567,40.83220325009562],[-74.83502772071711,40.821530247597074],[-74.83565971996867,40.818585247211715],[-74.8463897233963,40.81096124527004],[-74.85026472347802,40.804181244247474],[-74.8548667249403,40.804204244190494],[-74.85999172641547,40.801028242705904],[-74.86489572824279,40.802901243574574],[-74.86695972881388,40.796825241831755],[-74.87346873087077,40.79472824112453],[-74.88059973340252,40.79071723999012],[-74.88414173353358,40.79145024075369],[-74.88982073566775,40.78773723969704],[-74.84406971958482,40.75859223497593],[-74.84302571926975,40.756029235074685],[-74.82748571293311,40.74408023362877],[-74.82363271217757,40.74221823310362],[-74.81706970965719,40.74289923298157],[-74.80822970706598,40.7411502332367],[-74.79797470356144,40.74219423362715],[-74.79367770156144,40.74034723367741],[-74.77099069453105,40.73605623364407],[-74.75290168894578,40.73113723304891],[-74.73733468302223,40.72162723208971],[-74.72566767856841,40.719540232540545],[-74.55601962769774,40.758296245952316],[-74.55192762548167,40.75465924510146],[-74.55268162599599,40.7495202443318],[-74.54871262402042,40.74612724360043],[-74.54767762288512,40.73699524153267],[-74.54334062119653,40.73422324143567],[-74.53089461770857,40.72986224095669],[-74.52976761717048,40.72651324071807],[-74.53150661725381,40.72127523907397],[-74.5275206156779,40.716672239043234],[-74.52411961451564,40.71565123881593],[-74.52683361464075,40.71081723766246],[-74.51789761197517,40.70558123665563],[-74.51468361049226,40.70191723621677],[-74.51434761027502,40.694373234897625],[-74.52447861324889,40.68915023377396],[-74.52788061418282,40.68435223272437],[-74.52871461407071,40.67984523100143],[-74.52568761176606,40.6705772294457],[-74.5298556130833,40.66757522927131],[-74.52323060989471,40.64916522571007],[-74.51308960716372,40.64957122633674],[-74.50770260553153,40.652591226406955],[-74.50370160466942,40.65963822875094],[-74.4989346024209,40.661390228587265],[-74.48579759837425,40.66236822962071],[-74.48243659807537,40.6660372301888],[-74.47025459449036,40.66794023075136],[-74.46103659130726,40.67351223242889],[-74.45484858918921,40.674051233256684],[-74.45153558866772,40.679595233771785],[-74.45190458919278,40.68540523504419],[-74.44819958808068,40.68549123504487],[-74.43454958402745,40.693570237773386],[-74.4268155826904,40.70185323898389],[-74.42150958110746,40.70320123990397],[-74.40896957755955,40.709816241909394],[-74.40232457528501,40.71799224376817],[-74.39615857397726,40.71725024366309],[-74.39074157221245,40.718530243757705],[-74.39104657203949,40.72452624523783],[-74.38438857060156,40.724422245144844],[-74.3776505685411,40.730342246353956],[-74.37774856887981,40.73435624766595],[-74.37200656673832,40.73408324750315],[-74.3717395670528,40.73964824863419],[-74.3722015672384,40.743411249075855],[-74.36627356544841,40.74390124962288],[-74.36694256625668,40.74954725120023],[-74.35969156458978,40.751014251210314],[-74.36174256474457,40.755923252474105],[-74.36784356673094,40.76106825337085],[-74.37403356890111,40.757982251825354],[-74.3757645693816,40.76300125297672],[-74.37113756789326,40.76404425332646],[-74.369550568111,40.77140025528835],[-74.37274156929143,40.7760282559918],[-74.36686956840991,40.780356256417406],[-74.3670635693651,40.79329425923634],[-74.3643365684867,40.798882260130675],[-74.35948656664951,40.800085261344414],[-74.35072356486751,40.807433262455135],[-74.34893956478344,40.812727263894075],[-74.33842156066335,40.81303326431504],[-74.33220155898827,40.82171026633248],[-74.33495356074265,40.82740726746587],[-74.32879955903708,40.83192526847607],[-74.32985155981069,40.834166268571366],[-74.32800455944508,40.8499532720069],[-74.32431655939611,40.8581932734142],[-74.31913255734857,40.85844527336527],[-74.32209555946258,40.86405327455666],[-74.32624356034661,40.86609327474717],[-74.33634456391125,40.86771127453781],[-74.33802056492398,40.87840927671754],[-74.34040456567776,40.88139927768324],[-74.33666856596659,40.89377528029277],[-74.33763156633455,40.898797280629054],[-74.33429556561315,40.90546828210592],[-74.32733256270356,40.90530628297761],[-74.31864956114428,40.907600283738795],[-74.3186565601988,40.903248282560654],[-74.31241055873839,40.90540728310839],[-74.30304755566196,40.904337283737924],[-74.29242255195472,40.90581228395899],[-74.29127655166302,40.89978428265989],[-74.27197654530337,40.897329283329285]]]},properties:{geoid:”34027″,name:”Morris”,state_name:”New Jersey”,county_state_name:”Morris County, New Jersey”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:84.32,”60_65k_diff”:696.41,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:483.91,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.05,”27_65k_eptc”:446.7,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:446.7,”40_95k_eptc”:544.74,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:446.7,”40_65k_no_eptc”:544.74,”60_65k_no_eptc”:1156.83,”27_95k_no_eptc”:446.7,”40_95k_no_eptc”:544.74,”60_95k_no_eptc”:1156.83}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-74.14753049846883,40.78649926612258],[-74.13808649566421,40.79885426902083],[-74.13955749691088,40.80370726962353],[-74.13847549698792,40.813267271706906],[-74.1363544967592,40.8180862720689],[-74.1300174948672,40.81994627256062],[-74.19789051923014,40.85721727778691],[-74.2128505243642,40.86510227878337],[-74.24029153350274,40.88044428066566],[-74.25316953787136,40.88158128094348],[-74.26429054225787,40.886914281359644],[-74.26565054276932,40.892733281998325],[-74.27197654530337,40.897329283329285],[-74.29127655166302,40.89978428265989],[-74.29242255195472,40.90581228395899],[-74.30304755566196,40.904337283737924],[-74.31241055873839,40.90540728310839],[-74.3186565601988,40.903248282560654],[-74.31864956114428,40.907600283738795],[-74.32733256270356,40.90530628297761],[-74.33429556561315,40.90546828210592],[-74.33763156633455,40.898797280629054],[-74.33666856596659,40.89377528029277],[-74.34040456567776,40.88139927768324],[-74.33802056492398,40.87840927671754],[-74.33634456391125,40.86771127453781],[-74.32624356034661,40.86609327474717],[-74.32209555946258,40.86405327455666],[-74.31913255734857,40.85844527336527],[-74.32431655939611,40.8581932734142],[-74.32800455944508,40.8499532720069],[-74.32985155981069,40.834166268571366],[-74.32879955903708,40.83192526847607],[-74.33495356074265,40.82740726746587],[-74.33220155898827,40.82171026633248],[-74.33842156066335,40.81303326431504],[-74.34893956478344,40.812727263894075],[-74.35072356486751,40.807433262455135],[-74.35948656664951,40.800085261344414],[-74.3643365684867,40.798882260130675],[-74.3670635693651,40.79329425923634],[-74.36686956840991,40.780356256417406],[-74.37274156929143,40.7760282559918],[-74.369550568111,40.77140025528835],[-74.37113756789326,40.76404425332646],[-74.3757645693816,40.76300125297672],[-74.37403356890111,40.757982251825354],[-74.36784356673094,40.76106825337085],[-74.36174256474457,40.755923252474105],[-74.35969156458978,40.751014251210314],[-74.36694256625668,40.74954725120023],[-74.36627356544841,40.74390124962288],[-74.3722015672384,40.743411249075855],[-74.3717395670528,40.73964824863419],[-74.35894056321804,40.73598324873502],[-74.34866455884585,40.73022924749864],[-74.34268355737836,40.72518924729304],[-74.32559755125904,40.71708324633185],[-74.31628254824221,40.71927224659526],[-74.30925454542917,40.71444724645101],[-74.30352454363133,40.71319624610456],[-74.29721354175868,40.71519724624839],[-74.29258054076988,40.72091124787862],[-74.28552653879517,40.722270248478154],[-74.25584652864714,40.71337724740976],[-74.22195051722285,40.707349247541394],[-74.21300951421227,40.700916246516236],[-74.20924951169552,40.69071724469837],[-74.20154850934813,40.68668024402935],[-74.16992849895331,40.68855724582431],[-74.16505149789485,40.690169246390894],[-74.15786249495102,40.685960245751],[-74.15386249457364,40.68592524634649],[-74.14898549234518,40.68224424540136],[-74.13577648783026,40.67556724425643],[-74.13670448743999,40.674452244119436],[-74.11278848154636,40.70311025029891],[-74.12028848479173,40.715909253227636],[-74.1213884861359,40.72100925429412],[-74.11699448576331,40.73713325737274],[-74.12278748712284,40.742109257739415],[-74.13749349280108,40.74140625703545],[-74.14268949384575,40.739309256869205],[-74.14718949469946,40.7344092560545],[-74.15568849777907,40.733509255361604],[-74.16209449973866,40.736117255544464],[-74.16598850174887,40.74520725741019],[-74.16451450141533,40.75639625918568],[-74.162075501915,40.76148726047739],[-74.15768950022104,40.766108261139834],[-74.15579949949817,40.77082326290091],[-74.14898849859632,40.77800926448031],[-74.14753049846883,40.78649926612258]]]},properties:{geoid:”34013″,name:”Essex”,state_name:”New Jersey”,county_state_name:”Essex County, New Jersey”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:84.32,”60_65k_diff”:696.41,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:483.91,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.05,”27_65k_eptc”:446.7,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:446.7,”40_95k_eptc”:544.74,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:446.7,”40_65k_no_eptc”:544.74,”60_65k_no_eptc”:1156.83,”27_95k_no_eptc”:446.7,”40_95k_no_eptc”:544.74,”60_95k_no_eptc”:1156.83}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-78.91889909963128,41.99812730829597],[-78.96138111331081,41.99871530621486],[-79.05247314171783,41.999395302171564],[-79.15844117463513,41.99967829758328],[-79.25639720503575,41.99884329327677],[-79.31427622408997,41.99871329044395],[-79.3423452329433,41.99894128936781],[-79.41173425433136,41.99841228622607],[-79.51099628534931,41.998372282395316],[-79.61084031702369,41.99876527778528],[-79.61065131666014,41.989545275512405],[-79.6114763074364,41.882964255958406],[-79.61197630760783,41.87506425491538],[-79.61207430600395,41.850336250515845],[-79.61256430130283,41.79532424027325],[-79.61298929373199,41.70106722258007],[-79.61255428824889,41.63043820919169],[-79.61315028800772,41.62387120792491],[-79.51207325623581,41.62456721291854],[-79.47547324548292,41.625168214210916],[-79.36111620951795,41.62642421955074],[-79.29669418896145,41.625832222478465],[-79.2298861685434,41.62618122564164],[-79.15296414406511,41.626787228674395],[-79.1141661319451,41.626669230462696],[-79.03423310718746,41.62542623361825],[-78.99394509445023,41.62455323594927],[-78.95614108170575,41.62334223674294],[-78.95467208313187,41.64025224032185],[-78.95469008508913,41.66423324425301],[-78.95402508572138,41.68588424909861],[-78.95192308915281,41.7357042583686],[-78.95164709081547,41.75120726100559],[-78.94861509567578,41.8304892756101],[-78.92141108728215,41.830927276891245],[-78.92154708785985,41.84089027906743],[-78.91564508561476,41.84090427898931],[-78.91600708758475,41.86182028324643],[-78.91706008747119,41.86182928259679],[-78.91550309464508,41.952956299391985],[-78.91848409608129,41.95294829975001],[-78.91889909963128,41.99812730829597]]]},properties:{geoid:”42123″,name:”Warren”,state_name:”Pennsylvania”,county_state_name:”Warren County, Pennsylvania”,”27_22k_diff”:66.19,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.84,”40_35k_diff”:131.84,”60_35k_diff”:131.84,”27_65k_diff”:72.39,”40_65k_diff”:189.32,”60_65k_diff”:919.39,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:706.89,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.42,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:532.81,”40_95k_eptc”:649.74,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.19,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.88,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:532.81,”40_65k_no_eptc”:649.74,”60_65k_no_eptc”:1379.81,”27_95k_no_eptc”:532.81,”40_95k_no_eptc”:649.74,”60_95k_no_eptc”:1379.81}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-76.52802626290298,40.88262119591356],[-76.52486426379129,40.915944203067745],[-76.52833126460129,40.91848020335158],[-76.52224226302981,40.92275120396785],[-76.52014026283967,40.92664220474039],[-76.52178226441558,40.93166120581914],[-76.52582626525947,40.93457520584329],[-76.52939726693712,40.94015120681971],[-76.51242326151181,40.946110208608836],[-76.51587026378853,40.95026321009967],[-76.51456326287244,40.95675921052018],[-76.52734426801716,40.97152021289504],[-76.5652352818639,40.99982021688857],[-76.56621028275057,41.00859521925969],[-76.56284928327521,41.02345522195543],[-76.56226528314158,41.034222224084616],[-76.56991728725457,41.05376922734691],[-76.61897330330692,41.06376722759166],[-76.61604130347395,41.06875622890199],[-76.61736530411548,41.07336122949769],[-76.61549730360372,41.07971623088164],[-76.6204603054159,41.08484823114674],[-76.62085130622717,41.08996523243319],[-76.63089431189177,41.12521623837692],[-76.64076931749435,41.155726244270156],[-76.67877832878717,41.15418024229537],[-76.72999934609035,41.17188924405329],[-76.73267434730377,41.17204824365073],[-76.73127734645713,41.163088242108095],[-76.73169134612426,41.153247240428804],[-76.73580634565188,41.13784123710801],[-76.73351634394801,41.1276952356151],[-76.73534434393208,41.11010623170163],[-76.73419834351765,41.103809230371404],[-76.7348933421463,41.09214122863737],[-76.74650734412506,41.0655412231915],[-76.75650534692858,41.05051121960631],[-76.75967934683202,41.03871421745618],[-76.76450734747891,41.02961921481473],[-76.76196534585985,41.02594021437969],[-76.77059934833633,41.018735212483875],[-76.77377034970539,41.014364211553485],[-76.77578834930138,41.00812621018136],[-76.77371434813338,41.00256020969351],[-76.78490934948861,40.96693420256131],[-76.78654535035918,40.96517120234591],[-76.78544934939978,40.958915200543615],[-76.79050235070164,40.95671619988561],[-76.79005035058283,40.9516331991478],[-76.79261235128133,40.946655198410674],[-76.77570334593206,40.94947919930284],[-76.76737834263108,40.9497921999399],[-76.74302033582052,40.95449220185578],[-76.7348283327131,40.95445620222636],[-76.68714731847244,40.962761204943014],[-76.68212131659344,40.964970205864056],[-76.67486431452967,40.965510206238505],[-76.66135031078932,40.96800420736483],[-76.6524533077572,40.961651206597146],[-76.64533130567476,40.964432206983105],[-76.635061301679,40.96438620817972],[-76.62508229844035,40.96031720717415],[-76.60143828948856,40.942194204421455],[-76.58956728633741,40.94013520527931],[-76.55697927600922,40.93861720581737],[-76.55857227508714,40.9305042043759],[-76.56167227591044,40.92478620263513],[-76.56557427725276,40.92115420231889],[-76.5681132775164,40.91546220063138],[-76.56479727626616,40.90424119853547],[-76.56029627366902,40.898869198368075],[-76.55738027177676,40.88890219647061],[-76.55079127029427,40.88258519504377],[-76.52802626290298,40.88262119591356]]]},properties:{geoid:”42093″,name:”Montour”,state_name:”Pennsylvania”,county_state_name:”Montour County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.84,”27_65k_diff”:188.06,”40_65k_diff”:330.38,”60_65k_diff”:1218.95,”27_95k_diff”:0,”40_95k_diff”:117.88,”60_95k_diff”:1006.45,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.42,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:648.48,”40_95k_eptc”:672.92,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:648.48,”40_65k_no_eptc”:790.8,”60_65k_no_eptc”:1679.37,”27_95k_no_eptc”:648.48,”40_95k_no_eptc”:790.8,”60_95k_no_eptc”:1679.37}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-74.14753049846883,40.78649926612258],[-74.13077249257661,40.77784826466762],[-74.12719149031524,40.77135026314362],[-74.11640648770812,40.77328126396205],[-74.11396048751706,40.77631626492335],[-74.10533848478549,40.77716726573075],[-74.0984374815692,40.77253226475192],[-74.0986984818018,40.767749263601324],[-74.09583748089385,40.76286826286144],[-74.0879804780222,40.76444826396033],[-74.09009947932442,40.776891265612925],[-74.08914447945943,40.77960426651512],[-74.07985147735964,40.78973426843448],[-74.07785647698009,40.79429126998716],[-74.06903347420536,40.798357270968324],[-74.0638384727666,40.80416027191772],[-74.0585504709564,40.806285272961404],[-74.03654046371511,40.80785627390748],[-74.03165346256444,40.81326427528074],[-74.020415459496,40.81865227645284],[-74.0178204591164,40.82334927783566],[-74.01129445636487,40.82048327736237],[-74.01235345720568,40.81598527634865],[-73.99316244988552,40.80576727531177],[-73.99331145036126,40.80129427393276],[-73.98474044743897,40.79767027399576],[-73.96357844229857,40.826650280071426],[-73.952830439333,40.85111428498287],[-73.92982243528638,40.88869029344375],[-73.91425443237664,40.927968301250246],[-73.90846443177772,40.947888306011556],[-73.89614542981772,40.98188131237948],[-73.8936294298239,40.99717331602915],[-73.90271643264246,40.99733531602614],[-73.95232944997917,41.01968831781146],[-74.09676950032518,41.08390532597089],[-74.1681395253919,41.11531532904715],[-74.2112255399168,41.133722331074466],[-74.2518595490755,41.05816631496041],[-74.27222755204761,41.01794330654513],[-74.26426954940337,41.011943305759694],[-74.24859754390098,40.9921903024625],[-74.22453453447982,40.981311300796875],[-74.17114251798198,40.97707430201813],[-74.170276517958,40.983912303719364],[-74.14109550681877,40.966382301477275],[-74.14766750800916,40.9446202965641],[-74.13959150538986,40.93376729466149],[-74.1424315058847,40.929570294330006],[-74.140219504874,40.92401029286427],[-74.13151850114271,40.92209229248064],[-74.1294125012742,40.919742292872115],[-74.13337150102103,40.91321729116704],[-74.13165650033795,40.906327289348674],[-74.13341750069947,40.902366288978996],[-74.13282450093968,40.897082287760234],[-74.12845749905017,40.894285287742896],[-74.12969149915439,40.88490428606693],[-74.1215054954944,40.880962284754766],[-74.11549849287283,40.874783284459475],[-74.11072649103996,40.86505628227227],[-74.10707849043155,40.86224328185412],[-74.10720848954942,40.857537280802546],[-74.11339249238354,40.859420281402045],[-74.12082249463948,40.858263281050924],[-74.11923949312084,40.85205127950214],[-74.12403649380839,40.838725276924194],[-74.12099149258775,40.83054727496783],[-74.12377449299393,40.822765274147706],[-74.1300174948672,40.81994627256062],[-74.1363544967592,40.8180862720689],[-74.13847549698792,40.813267271706906],[-74.13955749691088,40.80370726962353],[-74.13808649566421,40.79885426902083],[-74.14753049846883,40.78649926612258]]]},properties:{geoid:”34003″,name:”Bergen”,state_name:”New Jersey”,county_state_name:”Bergen County, New Jersey”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:84.32,”60_65k_diff”:696.41,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:483.91,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.05,”27_65k_eptc”:446.7,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:446.7,”40_95k_eptc”:544.74,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:446.7,”40_65k_no_eptc”:544.74,”60_65k_no_eptc”:1156.83,”27_95k_no_eptc”:446.7,”40_95k_no_eptc”:544.74,”60_95k_no_eptc”:1156.83}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-76.99932033488686,39.720113951386594],[-76.99965234057116,39.81964197060366],[-77.00031434188568,39.83122697315669],[-76.99066533977654,39.83435597355847],[-76.98304533696516,39.84136097531205],[-76.97854533671271,39.847734976673046],[-76.97408533532865,39.849667977649666],[-76.96484233189707,39.85077997858403],[-76.95493432926331,39.85685798007115],[-76.96224033244802,39.86484298065306],[-76.96362233339624,39.8740249828874],[-76.97253833627983,39.872921982077585],[-76.9783593387744,39.88215898342427],[-76.97771633851234,39.885805984735654],[-76.98399434113279,39.89473898625389],[-76.98205734021668,39.897403986536105],[-76.98385134194983,39.902064988025565],[-76.97288333867516,39.91108898941145],[-76.97284133844839,39.91386899011796],[-76.96698533696606,39.916190990655174],[-76.96715933729563,39.92211299186651],[-76.97235433897715,39.92614899313678],[-76.9710623398338,39.9309629938065],[-76.97258733969296,39.93419499458095],[-76.96961733927196,39.93990499561544],[-76.9861073464329,39.96438999995041],[-76.99267434846347,39.97320500142198],[-77.01054935623439,40.00048900594462],[-77.01865035984494,40.013955008176794],[-77.0262403624896,40.01838600896512],[-77.03321336495505,40.01873200863215],[-77.04069236730403,40.02132800916406],[-77.05618337149319,40.02344600852355],[-77.06848737582618,40.02888000958344],[-77.07235637736383,40.03401701008911],[-77.07856538002626,40.03787601096683],[-77.08081438079809,40.04323001198435],[-77.09263038492996,40.05392801365524],[-77.10431838909203,40.057965013572755],[-77.10630939063365,40.059767013979865],[-77.12344639559458,40.066201014845234],[-77.1279183975036,40.06869701491253],[-77.13742740030403,40.06995301460877],[-77.16207340683653,40.05170501029992],[-77.18563241334202,40.02950900510181],[-77.22925142647237,40.025054002561255],[-77.27672344076026,40.017209998747546],[-77.36096946671435,40.002000992189906],[-77.40360847858919,39.99448598960789],[-77.47108749710748,39.94408497698868],[-77.46961349433118,39.91617697123581],[-77.46609349011725,39.86112396114242],[-77.4631774859871,39.82048095331266],[-77.46065848112208,39.753618940266044],[-77.45941947936993,39.73543093675158],[-77.4591364789427,39.719991933083115],[-77.39159645778413,39.71982793618088],[-77.30662043088529,39.719914939090174],[-77.17605938997043,39.71982394467522],[-77.03986134749577,39.71990094979783],[-76.99932033488686,39.720113951386594]]]},properties:{geoid:”42001″,name:”Adams”,state_name:”Pennsylvania”,county_state_name:”Adams County, Pennsylvania”,”27_22k_diff”:66.19,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.84,”40_35k_diff”:131.84,”60_35k_diff”:131.84,”27_65k_diff”:237.88,”40_65k_diff”:391.13,”60_65k_diff”:1347.96,”27_95k_diff”:25.38,”40_95k_diff”:178.63,”60_95k_diff”:1135.46,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.42,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:672.92,”40_95k_eptc”:672.92,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.19,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.88,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:698.3,”40_65k_no_eptc”:851.55,”60_65k_no_eptc”:1808.38,”27_95k_no_eptc”:698.3,”40_95k_no_eptc”:851.55,”60_95k_no_eptc”:1808.38}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-75.3335158607908,40.53706517411074],[-75.40441388687786,40.581162179983465],[-75.39127688309928,40.59655918332671],[-75.38856088339995,40.61443118762729],[-75.38283188174483,40.617163187905156],[-75.38305088200894,40.6236711896261],[-75.38841488482592,40.627977190428325],[-75.38746588375554,40.63313019148528],[-75.39289288659037,40.63442319117605],[-75.40893289196077,40.648282193456424],[-75.43012389965692,40.6684351963677],[-75.43040590082258,40.67416019777908],[-75.48147091591515,40.65575219215161],[-75.48372891627594,40.66020419311361],[-75.48502891796346,40.67150419511069],[-75.4911289197573,40.67700419569059],[-75.49871792221187,40.680013196431744],[-75.50305492481623,40.689723197932416],[-75.50974692758344,40.69416619856744],[-75.51562992928561,40.70220419953261],[-75.52255793299554,40.71349520130014],[-75.52552993395659,40.7201032026503],[-75.52654193459476,40.73330320496433],[-75.53015093633704,40.736351205627535],[-75.53736793907363,40.7376022061912],[-75.54055693949326,40.735627205520686],[-75.54180793896298,40.727926204192194],[-75.54814594085565,40.72311720303716],[-75.55816694390144,40.720894201934485],[-75.56441994596236,40.72347820200815],[-75.56885894814455,40.727359202329566],[-75.5706359490833,40.73247820360512],[-75.5761639512594,40.73518420358688],[-75.587903954172,40.73389520295658],[-75.59255995615112,40.736135203095536],[-75.59670395819006,40.743607204641876],[-75.60192796010327,40.7501032058662],[-75.60357096139991,40.75681320714658],[-75.60287196143783,40.76596420898125],[-75.6066609633686,40.771327209684905],[-75.60466696203302,40.77578521052882],[-75.60546096272746,40.78079121135755],[-75.60898696512045,40.78739521249067],[-75.67277298446993,40.775731207976875],[-75.6946229907684,40.77019420654971],[-75.70241999269837,40.76224820406957],[-75.7286020005005,40.75392320144811],[-75.73931100355661,40.7441631998016],[-75.74486500504854,40.740317198482565],[-75.75780900892455,40.735422197089406],[-75.76594901077985,40.730934196207265],[-75.77769201420824,40.72954219564952],[-75.77968401483109,40.72503019425823],[-75.79652001949559,40.71704219178452],[-75.80779102244514,40.70750019021248],[-75.84466503310092,40.69300918580603],[-75.85481103609285,40.69320018501357],[-75.89147504709355,40.67727818058984],[-75.8495150325553,40.649948176986456],[-75.82560602363503,40.633871174510865],[-75.77892300697553,40.60447017080586],[-75.73803999230869,40.57911316737137],[-75.6685719668022,40.534953161649014],[-75.57950493539643,40.4780651534092],[-75.52969591821261,40.447003149286964],[-75.48405890155193,40.41845914544603],[-75.40973488230416,40.48799216160751],[-75.36661187064225,40.51543216858609],[-75.33863486251805,40.53407617314423],[-75.3335158607908,40.53706517411074]]]},properties:{geoid:”42077″,name:”Lehigh”,state_name:”Pennsylvania”,county_state_name:”Lehigh County, Pennsylvania”,”27_22k_diff”:66.19,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.84,”40_35k_diff”:131.83,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:83.74,”60_65k_diff”:695.18,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:482.68,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:446.23,”40_65k_eptc”:460.42,”60_65k_eptc”:460.41,”27_95k_eptc”:446.23,”40_95k_eptc”:544.16,”60_95k_eptc”:672.91,”27_22k_no_eptc”:66.19,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.88,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.87,”27_65k_no_eptc”:446.23,”40_65k_no_eptc”:544.16,”60_65k_no_eptc”:1155.59,”27_95k_no_eptc”:446.23,”40_95k_no_eptc”:544.16,”60_95k_no_eptc”:1155.59}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-75.19680482235896,40.60858819294119],[-75.20181382431899,40.617196194508274],[-75.19789282273318,40.619340195633875],[-75.19068982084048,40.61996519531418],[-75.18859682042907,40.62364419695804],[-75.19051682173236,40.63543519877546],[-75.20045382565694,40.64922720145348],[-75.19085382337308,40.66194620416451],[-75.18297782183535,40.665755204673474],[-75.17802082063677,40.67177120638805],[-75.17694882001551,40.676699207001654],[-75.18056582169967,40.679371207747394],[-75.19112582535121,40.679467207394396],[-75.19692282641502,40.6813052073621],[-75.20092382862035,40.68550920803679],[-75.2039228292275,40.69150620891908],[-75.19872182927197,40.705306212418435],[-75.19261682727878,40.7158822144506],[-75.18674182643953,40.7194982148553],[-75.18605382576946,40.725690216958725],[-75.18294982510369,40.72933821776213],[-75.18280582507062,40.733658218361036],[-75.18773382800632,40.7392742190878],[-75.19535083023644,40.74548121990515],[-75.196536831081,40.75163922088503],[-75.19179783007489,40.75583822207204],[-75.18303882757618,40.75935222293413],[-75.17747882611417,40.764233224259115],[-75.17562182620135,40.772931226198295],[-75.17158882541791,40.77775322705316],[-75.16364982178122,40.77839422790399],[-75.1520648189844,40.77533522786721],[-75.13910781373296,40.773614227767084],[-75.13146681235314,40.77595822825875],[-75.12308981015916,40.78675423091602],[-75.11685580859167,40.78935623182853],[-75.10850680517699,40.791102231905],[-75.10080180425267,40.79980523371304],[-75.10027880422133,40.80758623591388],[-75.0905198008596,40.815921237186146],[-75.08393079987141,40.824479239232815],[-75.08551880049905,40.83009324046629],[-75.09494180423471,40.837111241174],[-75.09757380544512,40.84097524179218],[-75.09578580503724,40.84709024307449],[-75.09096380384497,40.84919524375982],[-75.07668579930639,40.8498832446147],[-75.07083179661795,40.84740024441018],[-75.06432979500585,40.848346244908925],[-75.06392679575275,40.85543224582715],[-75.05846379380272,40.860714247263246],[-75.05144979232112,40.864217248043104],[-75.05084079166343,40.86807524904459],[-75.05366579355999,40.873668250029084],[-75.05865679509307,40.87766225082139],[-75.06544179778182,40.885683252091326],[-75.07392680119223,40.892185253342234],[-75.07598180132602,40.89570025358946],[-75.07609180243197,40.907047255492],[-75.07929680352812,40.913888257182],[-75.09552980983516,40.92415625835817],[-75.10551581381061,40.936303260560514],[-75.10614981435862,40.93967826066448],[-75.11169081669291,40.94813526277048],[-75.11776881862374,40.95302126360081],[-75.12078782066979,40.962788265002814],[-75.1202338206216,40.968710266306424],[-75.1292338227182,40.95893826391864],[-75.14513182715606,40.95159226223099],[-75.15293682968124,40.94931926085197],[-75.16946483563434,40.94802326030047],[-75.17683783695009,40.94553125946161],[-75.17807483687362,40.940328258302294],[-75.18753284050696,40.93713925712137],[-75.19553784318018,40.93634525670534],[-75.2181918492665,40.9278832542831],[-75.22182285017612,40.91958925296117],[-75.24113185540114,40.90944624981751],[-75.23250385244768,40.899767248429306],[-75.26722586156586,40.8824812437561],[-75.27353186293368,40.87315824177394],[-75.28404086635061,40.86604823999217],[-75.30059587100052,40.85957123814031],[-75.32093287687469,40.855665236994014],[-75.34175388313587,40.84532523424737],[-75.38326789617236,40.83104522938131],[-75.41676090633787,40.82611022766176],[-75.4204919070842,40.8234592265384],[-75.44245191310688,40.81837522496968],[-75.47419492314522,40.81475422275559],[-75.48527392661572,40.812533222550655],[-75.50801993408191,40.809109220545494],[-75.51904693711276,40.80882122014777],[-75.52844594001286,40.80673321979385],[-75.54155094402422,40.80682321951487],[-75.55136094708338,40.804560218085385],[-75.55753394919063,40.80119621749638],[-75.56509295186183,40.801113216840854],[-75.57748995545315,40.79942221653372],[-75.59545496107634,40.79331021407364],[-75.6026099626999,40.788051213023515],[-75.60898696512045,40.78739521249067],[-75.60546096272746,40.78079121135755],[-75.60466696203302,40.77578521052882],[-75.6066609633686,40.771327209684905],[-75.60287196143783,40.76596420898125],[-75.60357096139991,40.75681320714658],[-75.60192796010327,40.7501032058662],[-75.59670395819006,40.743607204641876],[-75.59255995615112,40.736135203095536],[-75.587903954172,40.73389520295658],[-75.5761639512594,40.73518420358688],[-75.5706359490833,40.73247820360512],[-75.56885894814455,40.727359202329566],[-75.56441994596236,40.72347820200815],[-75.55816694390144,40.720894201934485],[-75.54814594085565,40.72311720303716],[-75.54180793896298,40.727926204192194],[-75.54055693949326,40.735627205520686],[-75.53736793907363,40.7376022061912],[-75.53015093633704,40.736351205627535],[-75.52654193459476,40.73330320496433],[-75.52552993395659,40.7201032026503],[-75.52255793299554,40.71349520130014],[-75.51562992928561,40.70220419953261],[-75.50974692758344,40.69416619856744],[-75.50305492481623,40.689723197932416],[-75.49871792221187,40.680013196431744],[-75.4911289197573,40.67700419569059],[-75.48502891796346,40.67150419511069],[-75.48372891627594,40.66020419311361],[-75.48147091591515,40.65575219215161],[-75.43040590082258,40.67416019777908],[-75.43012389965692,40.6684351963677],[-75.40893289196077,40.648282193456424],[-75.39289288659037,40.63442319117605],[-75.38746588375554,40.63313019148528],[-75.38841488482592,40.627977190428325],[-75.38305088200894,40.6236711896261],[-75.38283188174483,40.617163187905156],[-75.38856088339995,40.61443118762729],[-75.39127688309928,40.59655918332671],[-75.40441388687786,40.581162179983465],[-75.3335158607908,40.53706517411074],[-75.29352985026722,40.56198618065717],[-75.25815283944443,40.58201718539675],[-75.23684983409146,40.59075618799709],[-75.19680482235896,40.60858819294119]]]},properties:{geoid:”42095″,name:”Northampton”,state_name:”Pennsylvania”,county_state_name:”Northampton County, Pennsylvania”,”27_22k_diff”:66.19,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.84,”40_35k_diff”:131.83,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:83.74,”60_65k_diff”:695.18,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:482.68,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:446.23,”40_65k_eptc”:460.42,”60_65k_eptc”:460.41,”27_95k_eptc”:446.23,”40_95k_eptc”:544.16,”60_95k_eptc”:672.91,”27_22k_no_eptc”:66.19,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.88,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.87,”27_65k_no_eptc”:446.23,”40_65k_no_eptc”:544.16,”60_65k_no_eptc”:1155.59,”27_95k_no_eptc”:446.23,”40_95k_no_eptc”:544.16,”60_95k_no_eptc”:1155.59}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-75.18960181860332,40.59178419017929],[-75.18099081634631,40.59421219093415],[-75.18088881647712,40.59719519204939],[-75.17488781399793,40.59893419257653],[-75.17369681492465,40.6032131934442],[-75.16305981187516,40.61097519517387],[-75.16119781180717,40.61821119681335],[-75.15442081006442,40.621700197075626],[-75.14966880817033,40.620509197597464],[-75.14818880767088,40.6256341987855],[-75.1436828069393,40.629462198952886],[-75.13633580444959,40.63015819941024],[-75.1274868021831,40.63445020043131],[-75.11386779708123,40.637281201604566],[-75.10836079562009,40.6397622027126],[-75.10598879574195,40.644589203388],[-75.09625979299362,40.64797720426376],[-75.0889867905509,40.65540920636805],[-75.08200578918714,40.65770020746245],[-75.0772077880364,40.663333208317134],[-75.06825078509456,40.66861520979601],[-75.06208878269629,40.66975121034178],[-75.06019878274962,40.67304021128583],[-75.04916177979362,40.67947221220758],[-75.04405177811695,40.67872321250417],[-75.03766477633002,40.68363521366605],[-75.03402777497936,40.68357721409035],[-75.02318277151976,40.69095821569033],[-75.01411776902911,40.692784216139096],[-75.00244776557963,40.69383921726222],[-74.99614176360059,40.70002921880575],[-74.99076976230322,40.70323921897888],[-74.9818527603257,40.70566722012421],[-74.98001675938741,40.7105552212529],[-74.97011375623998,40.709870221596425],[-74.96804875632928,40.711332221955395],[-74.9635107549182,40.72047622347372],[-74.95832475309909,40.72543522510663],[-74.95172875172636,40.72774822561585],[-74.9465257505752,40.73481922727235],[-74.9307367465363,40.74915623057418],[-74.92694074544478,40.75494923182524],[-74.92264174411788,40.75665523195119],[-74.91523374245946,40.76244823386102],[-74.91330374126801,40.76655523464057],[-74.90271973840893,40.77184423602066],[-74.90396273991213,40.78115423793804],[-74.89553273759199,40.78400023891787],[-74.88982073566775,40.78773723969704],[-74.88414173353358,40.79145024075369],[-74.88059973340252,40.79071723999012],[-74.87346873087077,40.79472824112453],[-74.86695972881388,40.796825241831755],[-74.86489572824279,40.802901243574574],[-74.85999172641547,40.801028242705904],[-74.8548667249403,40.804204244190494],[-74.85026472347802,40.804181244247474],[-74.8463897233963,40.81096124527004],[-74.83565971996867,40.818585247211715],[-74.83502772071711,40.821530247597074],[-74.82761071813567,40.83220325009562],[-74.81905171610374,40.83605425166994],[-74.8196937168444,40.84094825192094],[-74.82373771779524,40.84363125289475],[-74.82159171756724,40.84917325348345],[-74.8141167151969,40.85123125488684],[-74.80995271416236,40.85448725573819],[-74.80924271418664,40.860215256339764],[-74.80370171221354,40.86106925648235],[-74.80194371210122,40.86390625770305],[-74.80826971474272,40.86943325832018],[-74.80573971396227,40.8742042593735],[-74.80741871559444,40.88155726041217],[-74.80383371458954,40.88578126198958],[-74.7916537107166,40.890676262683165],[-74.79030271025157,40.89642926422812],[-74.7760577070333,40.90535126605363],[-74.7694267048059,40.91094226777644],[-74.81540772277236,40.95367527483489],[-74.82309172526212,40.960527275527625],[-74.85933573857217,40.994742280488786],[-74.90188975554999,41.03409828703728],[-74.93889376892372,41.068777292481236],[-74.96690777928738,41.09441829601194],[-74.967409779313,41.09012529493623],[-74.97098878101372,41.0853012943927],[-74.98259178366823,41.07918029244987],[-74.9948487870941,41.07656429117817],[-75.00078178977809,41.073218291038124],[-75.00656579048916,41.06779028911636],[-75.0134707924994,41.06594928865975],[-75.01713079357857,41.05663128667839],[-75.02739179599833,41.0441142841539],[-75.02684879496495,41.03973928366525],[-75.03505979795551,41.03684428206985],[-75.0401077992365,41.03274328152878],[-75.04755880088854,41.02969728061591],[-75.07053380757272,41.01862827726548],[-75.084496812114,41.01592827616387],[-75.09352481437521,41.00945027525745],[-75.10911481947527,41.00411027308198],[-75.11059681952965,41.00218227337742],[-75.12342482378877,40.996137271732486],[-75.13057682588925,40.99110127037043],[-75.1325238259745,40.98124326802266],[-75.13552282579911,40.976873267582434],[-75.13470282574909,40.97204626665588],[-75.13136182371711,40.969284266240216],[-75.12260482195131,40.97016026617142],[-75.1202338206216,40.968710266306424],[-75.12078782066979,40.962788265002814],[-75.11776881862374,40.95302126360081],[-75.11169081669291,40.94813526277048],[-75.10614981435862,40.93967826066448],[-75.10551581381061,40.936303260560514],[-75.09552980983516,40.92415625835817],[-75.07929680352812,40.913888257182],[-75.07609180243197,40.907047255492],[-75.07598180132602,40.89570025358946],[-75.07392680119223,40.892185253342234],[-75.06544179778182,40.885683252091326],[-75.05865679509307,40.87766225082139],[-75.05366579355999,40.873668250029084],[-75.05084079166343,40.86807524904459],[-75.05144979232112,40.864217248043104],[-75.05846379380272,40.860714247263246],[-75.06392679575275,40.85543224582715],[-75.06432979500585,40.848346244908925],[-75.07083179661795,40.84740024441018],[-75.07668579930639,40.8498832446147],[-75.09096380384497,40.84919524375982],[-75.09578580503724,40.84709024307449],[-75.09757380544512,40.84097524179218],[-75.09494180423471,40.837111241174],[-75.08551880049905,40.83009324046629],[-75.08393079987141,40.824479239232815],[-75.0905198008596,40.815921237186146],[-75.10027880422133,40.80758623591388],[-75.10080180425267,40.79980523371304],[-75.10850680517699,40.791102231905],[-75.11685580859167,40.78935623182853],[-75.12308981015916,40.78675423091602],[-75.13146681235314,40.77595822825875],[-75.13910781373296,40.773614227767084],[-75.1520648189844,40.77533522786721],[-75.16364982178122,40.77839422790399],[-75.17158882541791,40.77775322705316],[-75.17562182620135,40.772931226198295],[-75.17747882611417,40.764233224259115],[-75.18303882757618,40.75935222293413],[-75.19179783007489,40.75583822207204],[-75.196536831081,40.75163922088503],[-75.19535083023644,40.74548121990515],[-75.18773382800632,40.7392742190878],[-75.18280582507062,40.733658218361036],[-75.18294982510369,40.72933821776213],[-75.18605382576946,40.725690216958725],[-75.18674182643953,40.7194982148553],[-75.19261682727878,40.7158822144506],[-75.19872182927197,40.705306212418435],[-75.2039228292275,40.69150620891908],[-75.20092382862035,40.68550920803679],[-75.19692282641502,40.6813052073621],[-75.19112582535121,40.679467207394396],[-75.18056582169967,40.679371207747394],[-75.17694882001551,40.676699207001654],[-75.17802082063677,40.67177120638805],[-75.18297782183535,40.665755204673474],[-75.19085382337308,40.66194620416451],[-75.20045382565694,40.64922720145348],[-75.19051682173236,40.63543519877546],[-75.18859682042907,40.62364419695804],[-75.19068982084048,40.61996519531418],[-75.19789282273318,40.619340195633875],[-75.20181382431899,40.617196194508274],[-75.19680482235896,40.60858819294119],[-75.19229282053661,40.6026841922697],[-75.18960181860332,40.59178419017929]]]},properties:{geoid:”34041″,name:”Warren”,state_name:”New Jersey”,county_state_name:”Warren County, New Jersey”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:84.32,”60_65k_diff”:696.41,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:483.91,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.05,”27_65k_eptc”:446.7,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:446.7,”40_95k_eptc”:544.74,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:446.7,”40_65k_no_eptc”:544.74,”60_65k_no_eptc”:1156.83,”27_95k_no_eptc”:446.7,”40_95k_no_eptc”:544.74,”60_95k_no_eptc”:1156.83}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-77.13742740030403,40.06995301460877],[-77.05521737848785,40.12906902908971],[-77.02886337150336,40.14774003371527],[-77.02275136985408,40.14582203417488],[-77.01967736910764,40.148317034622714],[-77.0113453659509,40.148457035157996],[-77.00365436371848,40.153110035996136],[-76.99236836109756,40.15517503658733],[-76.98681435929338,40.15513503758037],[-76.97901135581367,40.152037036501135],[-76.97477035515263,40.15323403688601],[-76.97122835368218,40.15703003786216],[-76.97366435449011,40.15929503881382],[-76.98067735742634,40.16056403883004],[-76.97802635701895,40.164785039659215],[-76.96687835335035,40.16271203904599],[-76.94991934781493,40.16579204089171],[-76.93928534490408,40.164272040733465],[-76.92910934144895,40.16128204060814],[-76.90728333462425,40.16549204236259],[-76.9076523345844,40.169380042556504],[-76.92329634010858,40.17709504416048],[-76.92830534205812,40.18381004487448],[-76.92655034241425,40.18848804594378],[-76.9202763406007,40.18648204594949],[-76.91672233832412,40.18324504491457],[-76.91345333776471,40.18768504635855],[-76.90855733623825,40.19073704669236],[-76.91330533794861,40.193195047123304],[-76.9186143404828,40.19831904852651],[-76.9294833431062,40.19686104764277],[-76.92221634208398,40.208348049788555],[-76.91785534054202,40.21038605057932],[-76.91491833975974,40.20594804979778],[-76.91053933800566,40.2055490497849],[-76.90257733608978,40.212984051825835],[-76.89867833543953,40.214640052592685],[-76.9033233371249,40.22111205340639],[-76.89696333566877,40.2246740546165],[-76.89180333253697,40.21590305302336],[-76.88562733072003,40.214001052220155],[-76.87750032827067,40.217842053839185],[-76.872746326463,40.215633053676314],[-76.86701732514429,40.21601005379039],[-76.86089532331982,40.21942205420727],[-76.8617533240989,40.22329705562806],[-76.85902532342105,40.2263360555814],[-76.86647532574476,40.231165056284354],[-76.87870933055864,40.2438970590094],[-76.88973633412527,40.24932105920165],[-76.89777333730781,40.254673059636225],[-76.90465233957491,40.26072506133496],[-76.91375434393403,40.271137062633336],[-76.91604234471195,40.279904064078245],[-76.92016134634287,40.28301806480924],[-76.92447834868742,40.29130206643648],[-76.9229773480045,40.30096406808397],[-76.91348734603557,40.31755607206771],[-76.91213134626389,40.32550307374626],[-76.9149723475798,40.32849207415658],[-76.94928435776241,40.31686907052365],[-76.97422136539738,40.31033806793827],[-77.00513037431072,40.30562506600991],[-77.02452138008121,40.303966065024014],[-77.04177138639874,40.30441006416469],[-77.05966139116335,40.30330106337466],[-77.06387639245986,40.30197506255507],[-77.07466239644874,40.30224406203107],[-77.09636740302945,40.300403061541836],[-77.10174640486528,40.29864906108243],[-77.12264641090957,40.296872059166894],[-77.13485141477915,40.29491205912723],[-77.15039941949816,40.291260057307255],[-77.18279742881937,40.28775105517615],[-77.20449843550442,40.287088054870914],[-77.23090444416016,40.28357905296561],[-77.23916544728948,40.28411005237907],[-77.24169344772527,40.282855052378004],[-77.27005945633663,40.278660049958674],[-77.29157846283489,40.27281004822479],[-77.31223746859462,40.26774804685073],[-77.31729046984046,40.26759804612952],[-77.33049347535214,40.275604047576735],[-77.33069847487232,40.28059604786855],[-77.32392647308134,40.28861304970358],[-77.32856347555925,40.29231905033048],[-77.3406494783709,40.28692304923486],[-77.35430148247245,40.279286047416655],[-77.36072048453421,40.274709046158776],[-77.38511649136673,40.26272004283205],[-77.40245949668117,40.256962040948736],[-77.41386149942471,40.25522303983139],[-77.42084750231393,40.25537603989065],[-77.42317950268756,40.257938040069504],[-77.41979750189802,40.26407804152201],[-77.4110464998079,40.26932304330172],[-77.40930649928767,40.2745620439207],[-77.40289549803113,40.28013604562931],[-77.38696949354238,40.29035904832294],[-77.36476448748547,40.30254905111449],[-77.35987548619212,40.30669205249854],[-77.35763748539206,40.31248405350054],[-77.36602048899572,40.31357705322017],[-77.37569549189458,40.31069905229271],[-77.39444749722165,40.30351404986697],[-77.41378050195905,40.29390004742209],[-77.42659750611647,40.286618045416496],[-77.45782751455741,40.26613304026262],[-77.47359851801096,40.254224037250374],[-77.49731752427576,40.24024203413281],[-77.5101115278797,40.23442403215758],[-77.51550453014421,40.230512031077474],[-77.52675253320862,40.22559502991641],[-77.5289625330851,40.223007029644194],[-77.53687053608476,40.21908002821808],[-77.55808754286039,40.21864602699602],[-77.57834354808078,40.206634023803595],[-77.58044154851115,40.20386402363791],[-77.58995655075746,40.196522021781604],[-77.59355155143913,40.192018020704175],[-77.60545055528891,40.185370019188916],[-77.61466755826257,40.19855702088096],[-77.62755456219129,40.18867301865542],[-77.61638755720111,40.17248801572301],[-77.61364455595694,40.170169015403786],[-77.61292055513786,40.16124201362924],[-77.60826355414439,40.15274601223064],[-77.60417755261699,40.1514200123714],[-77.59327954881863,40.141982011117314],[-77.59295454794646,40.13540100933652],[-77.59035054670312,40.1339530092486],[-77.58259854486795,40.134438009790784],[-77.57467354204432,40.12773700894964],[-77.56904654005517,40.12632100851477],[-77.562873537417,40.11929400771255],[-77.5610185363865,40.10836600543235],[-77.55791653417945,40.1031050044938],[-77.5615905350399,40.09834300320035],[-77.56041953445857,40.09426400276048],[-77.55388553238241,40.09589100302179],[-77.54809953067722,40.09013800262307],[-77.54317852894619,40.08979800310627],[-77.53993252743001,40.07394499990573],[-77.54196752680988,40.069882998688215],[-77.53489152482148,40.07027999934324],[-77.53049752303026,40.05923999677273],[-77.53248352320381,40.04875699461641],[-77.52627352055897,40.04568799509699],[-77.52199451932425,40.04658999540733],[-77.51710951765453,40.0443669949252],[-77.51975851896138,40.04047599390225],[-77.51489551698556,40.03438599256976],[-77.50763451422289,40.02839399211533],[-77.50921051360987,40.0249419910662],[-77.50011651000133,40.013453989285445],[-77.4954055087903,40.00515298792971],[-77.48923450586028,40.00134098768324],[-77.48433350445748,39.99559198654361],[-77.4789585022923,39.99176298583992],[-77.47439450127607,39.991944986256655],[-77.47097449935676,39.98685298525296],[-77.46578549809841,39.98444398529361],[-77.45966349545948,39.97548498401659],[-77.45411149359931,39.972439983361646],[-77.47108749710748,39.94408497698868],[-77.40360847858919,39.99448598960789],[-77.36096946671435,40.002000992189906],[-77.27672344076026,40.017209998747546],[-77.22925142647237,40.025054002561255],[-77.18563241334202,40.02950900510181],[-77.16207340683653,40.05170501029992],[-77.13742740030403,40.06995301460877]]]},properties:{geoid:”42041″,name:”Cumberland”,state_name:”Pennsylvania”,county_state_name:”Cumberland County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.83,”60_35k_diff”:131.83,”27_65k_diff”:230.11,”40_65k_diff”:381.65,”60_65k_diff”:1327.83,”27_95k_diff”:17.61,”40_95k_diff”:169.15,”60_95k_diff”:1115.33,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.05,”27_65k_eptc”:460.41,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:672.91,”40_95k_eptc”:672.92,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:690.52,”40_65k_no_eptc”:842.07,”60_65k_no_eptc”:1788.25,”27_95k_no_eptc”:690.52,”40_95k_no_eptc”:842.07,”60_95k_no_eptc”:1788.25}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-77.47108749710748,39.94408497698868],[-77.45411149359931,39.972439983361646],[-77.45966349545948,39.97548498401659],[-77.46578549809841,39.98444398529361],[-77.47097449935676,39.98685298525296],[-77.47439450127607,39.991944986256655],[-77.4789585022923,39.99176298583992],[-77.48433350445748,39.99559198654361],[-77.48923450586028,40.00134098768324],[-77.4954055087903,40.00515298792971],[-77.50011651000133,40.013453989285445],[-77.50921051360987,40.0249419910662],[-77.50763451422289,40.02839399211533],[-77.51489551698556,40.03438599256976],[-77.51975851896138,40.04047599390225],[-77.51710951765453,40.0443669949252],[-77.52199451932425,40.04658999540733],[-77.52627352055897,40.04568799509699],[-77.53248352320381,40.04875699461641],[-77.53049752303026,40.05923999677273],[-77.53489152482148,40.07027999934324],[-77.54196752680988,40.069882998688215],[-77.53993252743001,40.07394499990573],[-77.54317852894619,40.08979800310627],[-77.54809953067722,40.09013800262307],[-77.55388553238241,40.09589100302179],[-77.56041953445857,40.09426400276048],[-77.5615905350399,40.09834300320035],[-77.55791653417945,40.1031050044938],[-77.5610185363865,40.10836600543235],[-77.562873537417,40.11929400771255],[-77.56904654005517,40.12632100851477],[-77.57467354204432,40.12773700894964],[-77.58259854486795,40.134438009790784],[-77.59035054670312,40.1339530092486],[-77.59295454794646,40.13540100933652],[-77.59327954881863,40.141982011117314],[-77.60417755261699,40.1514200123714],[-77.60826355414439,40.15274601223064],[-77.61292055513786,40.16124201362924],[-77.61364455595694,40.170169015403786],[-77.61638755720111,40.17248801572301],[-77.62755456219129,40.18867301865542],[-77.61466755826257,40.19855702088096],[-77.60477055610303,40.206041023137125],[-77.60489055781069,40.22493002622222],[-77.60277255679551,40.227496026806705],[-77.6091735588517,40.23276102800948],[-77.61616956175519,40.23262402781053],[-77.6398955678107,40.21768602370747],[-77.64339656973598,40.22317302473192],[-77.64764457017421,40.22248502408327],[-77.64995357170969,40.22629102467102],[-77.6488805716105,40.23332702643298],[-77.6454045713883,40.23893602785322],[-77.64999257285805,40.247965029436806],[-77.64502557256498,40.25394003097892],[-77.64950457389344,40.257559031209254],[-77.65344957532253,40.257415030613544],[-77.66549657787078,40.2520570297418],[-77.67115758088666,40.25757703069231],[-77.65641857629602,40.27040103369397],[-77.66427757935737,40.2782350345708],[-77.66419757991947,40.280487035436],[-77.67176358289021,40.2898330364985],[-77.67586258394333,40.284707035256375],[-77.68516558627832,40.27631203344521],[-77.69895659000045,40.26578303116388],[-77.70303259060022,40.263584030526815],[-77.70839159210857,40.261356029385546],[-77.71347859376144,40.25652002833581],[-77.72419959610504,40.25013202649674],[-77.73763459935006,40.23741302391265],[-77.76832760667294,40.204137015850286],[-77.79638861384844,40.16682200722225],[-77.80519861515371,40.152868004858306],[-77.81297561725545,40.139094001176765],[-77.81586861779618,40.132449999951525],[-77.82799561944809,40.116771996956395],[-77.85677462535905,40.06923898600588],[-77.86141162679841,40.062959984449954],[-77.86449162771042,40.06157598423458],[-77.87665763155482,40.054668982739486],[-77.88332963260977,40.0485259812765],[-77.89357263441809,40.03334797753178],[-77.90478763746117,40.02278497515412],[-77.9056346376786,40.018733974824094],[-77.91433163942949,40.010310972136054],[-77.92095464121446,40.00045797056888],[-77.91979464088232,39.992659968785595],[-77.92486764140372,39.98433696725599],[-77.92659164104232,39.97919796635425],[-77.93241364246438,39.972400963955366],[-77.93384764313815,39.965422962538355],[-77.93655564327807,39.961131962032034],[-77.93779164315148,39.94895195931223],[-77.94727564442829,39.93494795616531],[-77.95317364627195,39.93164095545583],[-77.95619064723071,39.927031954385946],[-77.95438864687047,39.92321695386647],[-77.95654564644909,39.914831951669946],[-77.96269464755305,39.901733949742365],[-77.96474564863769,39.89963394911465],[-77.9751376489935,39.871795943264566],[-77.98383565082928,39.856505939255904],[-78.00270265475261,39.82660693317648],[-78.01909865915911,39.8071059286432],[-78.02850566094382,39.799907926521286],[-78.04640466524141,39.77930792159498],[-78.05310266664222,39.77030892028969],[-78.06450067022848,39.75770891668782],[-78.069299670429,39.74830591497055],[-78.09940567841932,39.722106908972364],[-78.05971566627441,39.72247991061733],[-77.92948662568256,39.722334915473795],[-77.80323658616659,39.72169392056195],[-77.75576357067162,39.72125092187104],[-77.67849254740212,39.72091492456179],[-77.66956554417547,39.72067192527149],[-77.56748851171083,39.7204179289584],[-77.50282349156599,39.71989393183079],[-77.4591364789427,39.719991933083115],[-77.45941947936993,39.73543093675158],[-77.46065848112208,39.753618940266044],[-77.4631774859871,39.82048095331266],[-77.46609349011725,39.86112396114242],[-77.46961349433118,39.91617697123581],[-77.47108749710748,39.94408497698868]]]},properties:{geoid:”42055″,name:”Franklin”,state_name:”Pennsylvania”,county_state_name:”Franklin County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.83,”60_35k_diff”:131.83,”27_65k_diff”:230.11,”40_65k_diff”:381.65,”60_65k_diff”:1327.83,”27_95k_diff”:17.61,”40_95k_diff”:169.15,”60_95k_diff”:1115.33,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.05,”27_65k_eptc”:460.41,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:672.91,”40_95k_eptc”:672.92,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:690.52,”40_65k_no_eptc”:842.07,”60_65k_no_eptc”:1788.25,”27_95k_no_eptc”:690.52,”40_95k_no_eptc”:842.07,”60_95k_no_eptc”:1788.25}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-75.9976380967849,40.913267222141855],[-75.89264606508156,40.950564233313024],[-75.86886005820516,40.959357236599594],[-75.84802605265959,40.96636523801128],[-75.84962705324428,40.97161323953712],[-75.81957704397104,40.98207724234582],[-75.80170403866612,40.98292524339953],[-75.76467402792062,40.99671824770941],[-75.7321850180767,41.00813225103125],[-75.73846802038115,41.016828252087706],[-75.73915102127594,41.02803925449413],[-75.74274702375853,41.03140525457928],[-75.75756102827013,41.03154725440231],[-75.761227029611,41.04106325586419],[-75.76554203103774,41.043976256829865],[-75.77044003278034,41.050560257340344],[-75.77153803413337,41.06109725945122],[-75.7700450338728,41.068419260821514],[-75.77197603541579,41.07690026297156],[-75.76566803452504,41.084398264218365],[-75.7675520349764,41.091663265513056],[-75.7614720327062,41.091581265597895],[-75.75502503131452,41.09407126693676],[-75.7528450312599,41.09723826681381],[-75.75436503129751,41.102313268169794],[-75.74737102930341,41.10393726836191],[-75.74083702688628,41.102232268296625],[-75.73250102506634,41.10297626885526],[-75.72883602374353,41.10800027047174],[-75.72365602240458,41.109442271132494],[-75.71648702084985,41.118209272457094],[-75.70789701730764,41.11630627224864],[-75.70967001866578,41.121994273890444],[-75.70281601698916,41.12262727420474],[-75.70059501653894,41.127331274919044],[-75.6913130133215,41.1314952761113],[-75.6842890107826,41.13042427631572],[-75.67861101008448,41.133031277239354],[-75.66749700629481,41.13398827731758],[-75.66150400353779,41.12923327668037],[-75.65642600226462,41.122939275832806],[-75.65821600191015,41.118559274646394],[-75.65454800101179,41.11657327443397],[-75.64941399940439,41.1223122757284],[-75.64838599991205,41.125503277093856],[-75.64026699700602,41.12683127711843],[-75.63416399463159,41.123254276870775],[-75.63283199421141,41.12795327764738],[-75.62806999276668,41.12829527832712],[-75.62838699403997,41.136854279551265],[-75.61417498922205,41.145176281646954],[-75.61557899042838,41.15071328304942],[-75.60931398849021,41.15006028328017],[-75.6030909866706,41.15215728335735],[-75.60450198777228,41.15611828427447],[-75.60073798635908,41.16150528520922],[-75.60721798917173,41.16420228527307],[-75.61171899063872,41.16419528570538],[-75.61655999225242,41.172686286885344],[-75.62405599405338,41.16975828567355],[-75.63184499647642,41.16967728622814],[-75.63665299825492,41.17136728589345],[-75.63949900006148,41.17622228661457],[-75.64339400102224,41.17618028670948],[-75.64375300158248,41.18223628736472],[-75.64923500328311,41.18718128868667],[-75.65081400750572,41.22836729616607],[-75.65227500911016,41.25739130167986],[-75.67930601860425,41.264309301990856],[-75.67934601982368,41.287968306727535],[-75.68966302294805,41.28779330600367],[-75.69082602489559,41.304343309127276],[-75.69412202617936,41.30411830935113],[-75.69496102662772,41.31758531137591],[-75.68784302433029,41.317844311783865],[-75.68860802664369,41.33945431633162],[-75.74211604410696,41.34835231625126],[-75.76782805390746,41.36536231836461],[-75.79511806332282,41.37712731955304],[-75.79768806391024,41.38154331976724],[-75.80655206682017,41.38519132049916],[-75.81957707090676,41.38752632005466],[-75.82900107541926,41.39320632124073],[-75.8326330762135,41.39994232207193],[-75.83122507779213,41.41781432568665],[-75.83451407879005,41.42697332714255],[-75.83928908053936,41.42464132622879],[-75.9014070987122,41.409571321319056],[-75.92914610732264,41.40348131876394],[-75.96884111945245,41.394040316225514],[-75.98327212345266,41.391071314785975],[-76.00507213009493,41.38455931309379],[-76.05247514488201,41.382714310758246],[-76.15888317932804,41.3799153061574],[-76.28280121799624,41.37725230034644],[-76.31026322300154,41.31020628677205],[-76.31291522202682,41.287829282580745],[-76.31859021988912,41.23548027237433],[-76.31995921863381,41.21126326714852],[-76.31923821846736,41.20810026700551],[-76.2999852103953,41.17172726037657],[-76.2776411996569,41.1318122536554],[-76.24977219121303,41.135070255169516],[-76.228977185554,41.138474256977915],[-76.22848017912406,41.05364024063229],[-76.23119617963329,41.05017624016913],[-76.22077117264107,41.00009323111791],[-76.20782916556635,40.94974822149622],[-76.10970813322771,40.923653220056394],[-76.02800810569146,40.90232121959711],[-75.9976380967849,40.913267222141855]]]},properties:{geoid:”42079″,name:”Luzerne”,state_name:”Pennsylvania”,county_state_name:”Luzerne County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.83,”40_35k_diff”:131.83,”60_35k_diff”:131.84,”27_65k_diff”:87.26,”40_65k_diff”:207.45,”60_65k_diff”:957.89,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:745.39,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.41,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:547.67,”40_95k_eptc”:667.87,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:547.67,”40_65k_no_eptc”:667.87,”60_65k_no_eptc”:1418.31,”27_95k_no_eptc”:547.67,”40_95k_no_eptc”:667.87,”60_95k_no_eptc”:1418.31}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-78.20638287447056,41.99952633915302],[-78.20617686792569,41.913030323278036],[-78.20666586552248,41.8762303159504],[-78.20495885857896,41.791421300164934],[-78.20400085101691,41.70593528429667],[-78.20364284484296,41.617607267608605],[-78.18785683915024,41.6036992663076],[-78.14174382082307,41.56066625951145],[-78.12133481349211,41.541322257172496],[-78.10291980560496,41.52450825467008],[-78.08047379699903,41.50327025171817],[-78.05044478512805,41.47547024742285],[-77.98919676600318,41.47483024981132],[-77.95213975522569,41.475613251894465],[-77.861294726608,41.476207255665685],[-77.82829171508357,41.47699025719084],[-77.77232969764806,41.47752925953763],[-77.73366668585096,41.47759326135811],[-77.59813164284154,41.478584267040894],[-77.59897464541503,41.50995127289529],[-77.59928064783205,41.54227927870558],[-77.60093765393819,41.61604529293923],[-77.60386466396925,41.74458131659821],[-77.6045216650633,41.759960319762264],[-77.60671167456668,41.87507734067145],[-77.6079186790435,41.9242993498308],[-77.60916168244414,41.96125735717078],[-77.61002968473923,41.99937636391792],[-77.6487216973062,41.999481362665286],[-77.7132027182797,41.998847359767616],[-77.82293975270048,41.99830435529917],[-77.89435377543032,41.99821535181898],[-77.94035678962578,41.998478350431505],[-78.04042282175712,41.999427345843436],[-78.12213384787523,42.00036634271615],[-78.17689086468225,42.000029340069666],[-78.20638287447056,41.99952633915302]]]},properties:{geoid:”42105″,name:”Potter”,state_name:”Pennsylvania”,county_state_name:”Potter County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.83,”60_35k_diff”:131.83,”27_65k_diff”:55.33,”40_65k_diff”:168.51,”60_65k_diff”:875.2,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:662.7,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.05,”27_65k_eptc”:460.41,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:515.74,”40_95k_eptc”:628.93,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:515.74,”40_65k_no_eptc”:628.93,”60_65k_no_eptc”:1335.62,”27_95k_no_eptc”:515.74,”40_95k_no_eptc”:628.93,”60_95k_no_eptc”:1335.62}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-79.87142826030298,40.197398928220785],[-79.83925325223427,40.208762932038056],[-79.81442324426071,40.21668793444435],[-79.78259123591663,40.22763393758485],[-79.80296724194766,40.23149693752425],[-79.8074342437055,40.236901938476066],[-79.79911224199638,40.2469739410457],[-79.796656241563,40.252840941508296],[-79.78924324020402,40.25959994315965],[-79.78750523932496,40.2632499443953],[-79.79450524263751,40.27134394512024],[-79.79651924331658,40.279452947248224],[-79.79471824334419,40.28169094720497],[-79.78012023890386,40.282116947963544],[-79.77643323783158,40.284444949130005],[-79.77596623786849,40.289217949399834],[-79.78456924146153,40.29607395093893],[-79.78865124265535,40.29774595092278],[-79.7842112419683,40.31390195452578],[-79.77951524186417,40.33510995858735],[-79.77108524318645,40.37542696655423],[-79.76561324162502,40.38447896841875],[-79.76464124141678,40.39032497002806],[-79.75861223960338,40.39207197044621],[-79.75377923813078,40.38854596991498],[-79.74802723629927,40.39076497080811],[-79.7446372357662,40.3961709713658],[-79.73252623263978,40.39960697251345],[-79.73228123303655,40.40523597408244],[-79.7276582317547,40.41299497552143],[-79.72234122996463,40.41492697585038],[-79.71749222850107,40.41367897621751],[-79.71603122917764,40.417420977088334],[-79.7069422263906,40.42232697795845],[-79.70478622642196,40.42633197943682],[-79.70339622792353,40.4514689842896],[-79.70213422999043,40.489642991080814],[-79.70209023212499,40.52177099734985],[-79.70162723193216,40.525456998311306],[-79.70790523501073,40.53067099852254],[-79.71437623726348,40.5328859987714],[-79.72113123929283,40.54117000069302],[-79.7286692415577,40.543443000091564],[-79.73665224502017,40.54932300096101],[-79.74265924624002,40.548531000369884],[-79.75170424924659,40.55183100076122],[-79.765093253352,40.54924599972765],[-79.76854625535096,40.55500400084637],[-79.77413425842585,40.568384003496305],[-79.77480525855738,40.572812004115875],[-79.77336425843812,40.58209500542547],[-79.77162625806075,40.58563700629151],[-79.76319325664475,40.59362700875062],[-79.74944025239697,40.598875009713026],[-79.73609024795189,40.60205101135669],[-79.72315724528877,40.60699701269695],[-79.7145792423898,40.61701801457435],[-79.70333724000145,40.62570301675044],[-79.69435623835574,40.635135019632514],[-79.6902812373859,40.64088102095543],[-79.68897823669626,40.645443021681565],[-79.69108523799461,40.65247602300176],[-79.6958252400251,40.66151302464331],[-79.692881240698,40.66961902576937],[-79.70754924437438,40.66985902539147],[-79.7327472529399,40.6692480241209],[-79.78065426769724,40.67123602208621],[-79.81873227919145,40.67171602045886],[-79.82943628254102,40.6711500205172],[-79.85155929008795,40.672296019182454],[-79.87523729728055,40.672405018402344],[-79.91462930973557,40.673294017332765],[-79.95994232333577,40.672288015290924],[-79.98784533201541,40.673595013884636],[-80.02100934179832,40.674069013000185],[-80.07139635745709,40.6741820106137],[-80.07143735795084,40.674943010491106],[-80.10106136714174,40.67401700885313],[-80.12779437559725,40.6736120077141],[-80.1485003817312,40.67377700705386],[-80.14511337650778,40.613454995906714],[-80.15164537828412,40.611152994698564],[-80.15501637851989,40.608020994547516],[-80.16082838107565,40.609498993937876],[-80.1648473814831,40.60696499393572],[-80.17602838492395,40.60812099348085],[-80.18056638682842,40.6073519927766],[-80.18475638756911,40.603592991974736],[-80.18652238724073,40.596133990843974],[-80.19328439018042,40.5969409906512],[-80.20416639226066,40.58857598815154],[-80.20797939387703,40.58808198853686],[-80.21455239452814,40.580826986405754],[-80.21791339570557,40.58188198678515],[-80.22709239880315,40.57416198470331],[-80.25142340476681,40.556030980083385],[-80.27802941104602,40.536743975716554],[-80.36080443222788,40.47759896013245],[-80.31284841483746,40.43937095541137],[-80.2961974090554,40.42548395299482],[-80.22193238166281,40.36509394538978],[-80.20019937378541,40.34716094248926],[-80.18460636712668,40.33314694079266],[-80.10971534304369,40.31028393990169],[-80.08291333392575,40.30252093958947],[-80.02663531510112,40.285452938093975],[-79.91446427833631,40.25245093641893],[-79.92525928117466,40.24506893481221],[-79.93759328464775,40.24152693384277],[-79.95683729048837,40.240205932735066],[-79.9625962921898,40.23877593193374],[-79.97004529371681,40.23331193055233],[-79.97091929372661,40.22690092972703],[-79.96685229264989,40.2220959284849],[-79.95794328847447,40.214266927698084],[-79.95038528662255,40.211566927522625],[-79.92929227933492,40.20708892765724],[-79.91871527505526,40.20028692634159],[-79.91078627322004,40.19698492624026],[-79.90033726910772,40.194848926698675],[-79.88874226602145,40.19474092712124],[-79.88111826350074,40.19665492767314],[-79.87142826030298,40.197398928220785]]]},properties:{geoid:”42003″,name:”Allegheny”,state_name:”Pennsylvania”,county_state_name:”Allegheny County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:26.92,”60_65k_diff”:574.51,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:362.01,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:399.63,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:399.63,”40_95k_eptc”:487.34,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.87,”27_65k_no_eptc”:399.63,”40_65k_no_eptc”:487.34,”60_65k_no_eptc”:1034.93,”27_95k_no_eptc”:399.63,”40_95k_no_eptc”:487.34,”60_95k_no_eptc”:1034.93}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-76.8961163969011,41.139078230926486],[-76.88814739564812,41.153815234087496],[-76.88415739446948,41.157354234984346],[-76.8702633905371,41.160063235730384],[-76.85691838637185,41.16364923707814],[-76.82817037757793,41.16578823874086],[-76.8259653767622,41.16667923904783],[-76.79080936636252,41.17574024179244],[-76.73267434730377,41.17204824365073],[-76.72999934609035,41.17188924405329],[-76.67877832878717,41.15418024229537],[-76.64076931749435,41.155726244270156],[-76.59260930208491,41.15777324654787],[-76.52165428353335,41.2142682599492],[-76.49965427776195,41.2338642647722],[-76.47881327236514,41.25009126824722],[-76.4475992640472,41.27563727426822],[-76.49969128120773,41.28548727457606],[-76.52027828816362,41.28823327396674],[-76.54849029678165,41.29314327430875],[-76.54782329761997,41.29573027480946],[-76.59253431193862,41.304340274462724],[-76.66129933678985,41.34957328076333],[-76.70730835378552,41.378790284433244],[-76.7451703675353,41.40236228678522],[-76.74949936886024,41.40558028748115],[-76.76785637842165,41.45820929692207],[-76.78279938644361,41.502631304875095],[-76.79755439404285,41.54299731144566],[-76.80461739760078,41.564541315569656],[-76.81373340230542,41.590042319637504],[-76.87471642231779,41.59692731835535],[-76.87833342247934,41.59055431734416],[-76.88288842362711,41.58838331691312],[-76.90843443116232,41.58147131446468],[-76.91743743464743,41.58271131449052],[-76.92217343659406,41.58104531391339],[-76.92657243629604,41.571099311548416],[-76.9329644381753,41.56900031065257],[-76.94307944181269,41.56933131042403],[-76.95239344456407,41.56505830955726],[-76.96325144765193,41.55478030745259],[-76.96048144606146,41.55137930631721],[-77.02264746595856,41.54961430372033],[-77.11718549517981,41.5471422995759],[-77.28499154889735,41.5441262921611],[-77.2985075526741,41.544398291666866],[-77.33787156505268,41.54408929029585],[-77.40009858463696,41.54403928702144],[-77.50549661820207,41.543129283307785],[-77.54727263168708,41.54288228076386],[-77.59928064783205,41.54227927870558],[-77.59897464541503,41.50995127289529],[-77.59813164284154,41.478584267040894],[-77.59728463979886,41.441064260125614],[-77.58467363639429,41.441309260256695],[-77.58054263411294,41.4355872598328],[-77.57574263144346,41.42161025754231],[-77.57093263009476,41.415246255910574],[-77.56443762700724,41.412691255911284],[-77.55045162190638,41.395834252928175],[-77.54190161862716,41.381304251091954],[-77.54001061722046,41.36810924896225],[-77.53744061611324,41.364811248172636],[-77.52653961150871,41.35853624699193],[-77.51614760857036,41.35587524718603],[-77.49919560248858,41.35358524705578],[-77.48556959778793,41.34528924641573],[-77.47598959471219,41.33830224552277],[-77.47453559303598,41.33402924499086],[-77.4750315933356,41.32669724343197],[-77.4718645913088,41.31428124082815],[-77.46824758944312,41.31043724023645],[-77.45642658585328,41.30464723955282],[-77.45005658343754,41.293270237707496],[-77.44516058109713,41.28777023706221],[-77.42940257607168,41.282148236751645],[-77.4249475731555,41.27311123560773],[-77.41612756987854,41.27006423498256],[-77.41066956833558,41.26622923484306],[-77.40440956539945,41.258178233566625],[-77.3990455643052,41.25306123278122],[-77.39082656064512,41.247794231745864],[-77.37035255313147,41.23308722975754],[-77.36273155148066,41.23358823066441],[-77.35804954913299,41.23060522944808],[-77.34962954607792,41.22888122962504],[-77.34976754541363,41.21992622824442],[-77.33430554142437,41.22048422884996],[-77.32089353673209,41.21894022898158],[-77.30636653105809,41.208085227767086],[-77.29901252819286,41.20097522666273],[-77.29058252503343,41.19510822556793],[-77.29365352670513,41.19107722511361],[-77.29306152569299,41.18648122418463],[-77.28830852437802,41.18299822323704],[-77.27741352029294,41.180547223178486],[-77.27245251844118,41.17545122245084],[-77.27202051801741,41.17254222223234],[-77.26223351476628,41.162417220393564],[-77.24969350984061,41.15091521928457],[-77.16428047640328,41.06871620705769],[-77.14411346978856,41.06884820776083],[-77.11384146112556,41.06904020904809],[-77.0682384478852,41.0852392141006],[-76.97794141940466,41.08789121781746],[-76.96792341837731,41.12157722488631],[-76.96023141789424,41.14880922992035],[-76.8961163969011,41.139078230926486]]]},properties:{geoid:”42081″,name:”Lycoming”,state_name:”Pennsylvania”,county_state_name:”Lycoming County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.83,”40_35k_diff”:131.83,”60_35k_diff”:131.83,”27_65k_diff”:52.73,”40_65k_diff”:165.35,”60_65k_diff”:868.49,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:655.99,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.42,”40_65k_eptc”:460.42,”60_65k_eptc”:460.41,”27_95k_eptc”:513.15,”40_95k_eptc”:625.77,”60_95k_eptc”:672.91,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.87,”27_65k_no_eptc”:513.15,”40_65k_no_eptc”:625.77,”60_65k_no_eptc”:1328.9,”27_95k_no_eptc”:513.15,”40_95k_no_eptc”:625.77,”60_95k_no_eptc”:1328.9}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-76.56634122940726,40.196652061278385],[-76.50204621007333,40.217443067634875],[-76.47035920076765,40.22708107106495],[-76.4354121908463,40.23822907424108],[-76.36820017012619,40.24742407893062],[-76.30758015171806,40.255074083060556],[-76.26106513808517,40.273354087884805],[-76.15121710576648,40.31597910027737],[-76.15788510867286,40.32095710082173],[-76.20553012607792,40.360669107662574],[-76.23191813527953,40.36630010771689],[-76.24967514153367,40.37722910859278],[-76.32843916905017,40.42682811504948],[-76.35225617775289,40.441467117560705],[-76.44018320867728,40.49596012434046],[-76.49968623026912,40.532610129397874],[-76.53541624302886,40.555165132401825],[-76.58926025762597,40.52488512429168],[-76.62468926767616,40.504689119566926],[-76.67804228244565,40.47472511183401],[-76.66565527653916,40.44217110521599],[-76.63627126258514,40.36644709160926],[-76.62625725716038,40.341166087824114],[-76.61264925076011,40.30818808192341],[-76.59133824030455,40.25209507125608],[-76.56953422974124,40.19608106139943],[-76.56634122940726,40.196652061278385]]]},properties:{geoid:”42075″,name:”Lebanon”,state_name:”Pennsylvania”,county_state_name:”Lebanon County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.83,”60_35k_diff”:131.83,”27_65k_diff”:230.11,”40_65k_diff”:381.65,”60_65k_diff”:1327.83,”27_95k_diff”:17.61,”40_95k_diff”:169.15,”60_95k_diff”:1115.33,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.05,”27_65k_eptc”:460.41,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:672.91,”40_95k_eptc”:672.92,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:690.52,”40_65k_no_eptc”:842.07,”60_65k_no_eptc”:1788.25,”27_95k_no_eptc”:690.52,”40_95k_no_eptc”:842.07,”60_95k_no_eptc”:1788.25}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-74.1300174948672,40.81994627256062],[-74.12377449299393,40.822765274147706],[-74.12099149258775,40.83054727496783],[-74.12403649380839,40.838725276924194],[-74.11923949312084,40.85205127950214],[-74.12082249463948,40.858263281050924],[-74.11339249238354,40.859420281402045],[-74.10720848954942,40.857537280802546],[-74.10707849043155,40.86224328185412],[-74.11072649103996,40.86505628227227],[-74.11549849287283,40.874783284459475],[-74.1215054954944,40.880962284754766],[-74.12969149915439,40.88490428606693],[-74.12845749905017,40.894285287742896],[-74.13282450093968,40.897082287760234],[-74.13341750069947,40.902366288978996],[-74.13165650033795,40.906327289348674],[-74.13337150102103,40.91321729116704],[-74.1294125012742,40.919742292872115],[-74.13151850114271,40.92209229248064],[-74.140219504874,40.92401029286427],[-74.1424315058847,40.929570294330006],[-74.13959150538986,40.93376729466149],[-74.14766750800916,40.9446202965641],[-74.14109550681877,40.966382301477275],[-74.170276517958,40.983912303719364],[-74.17114251798198,40.97707430201813],[-74.22453453447982,40.981311300796875],[-74.24859754390098,40.9921903024625],[-74.26426954940337,41.011943305759694],[-74.27222755204761,41.01794330654513],[-74.2518595490755,41.05816631496041],[-74.2112255399168,41.133722331074466],[-74.21776754274515,41.136025331433345],[-74.25073855413221,41.1501763331805],[-74.26701855944546,41.157729333470364],[-74.29991257101175,41.17187933500938],[-74.34641758769281,41.19274233789486],[-74.36751159449284,41.20324933920463],[-74.39001060035551,41.18580333516015],[-74.42126160956751,41.160542328430175],[-74.47676162340859,41.109666316639036],[-74.48313662537768,41.10439631577114],[-74.50321363138539,41.08588131128435],[-74.48683662498557,41.07645331057242],[-74.48907262501365,41.071917308977966],[-74.48790262463002,41.06527530824578],[-74.49569962652133,41.05997030672986],[-74.49863762706845,41.04840330451543],[-74.50169362807273,41.04210630325029],[-74.49939762599143,41.035575301616596],[-74.48738162288731,41.03930330292649],[-74.48493862282679,41.04286230409816],[-74.47588361984869,41.0479043051947],[-74.4683516177368,41.04828730578958],[-74.46122061469661,41.05204030671938],[-74.45641461331398,41.05201230685324],[-74.44701861138347,41.05443730718735],[-74.44187860879185,41.05031930694275],[-74.44048960787055,41.043861305061796],[-74.43252460485337,41.03784430470984],[-74.42821460428712,41.03743430483338],[-74.42769160283599,41.03189930407948],[-74.43253660467857,41.02636930241955],[-74.43504160495253,41.020029301108664],[-74.4281546029461,41.02068130139954],[-74.4236876019497,41.02762330339836],[-74.4153795992669,41.02801930295739],[-74.40620559557632,41.02418430255215],[-74.3998285934979,41.01734330148536],[-74.39129559085713,41.01597230225531],[-74.38938159008593,41.01231430155122],[-74.37673758533543,41.013869301847414],[-74.37126858355266,41.01132730193816],[-74.3627375811382,41.013504302575235],[-74.35509457886927,41.01378030272207],[-74.3512785776489,41.01068430235209],[-74.35243857736535,41.005710300857174],[-74.34954557646888,41.00399230101207],[-74.3419935743631,41.00693630226199],[-74.33579657223414,41.00728330230856],[-74.33468957201204,41.00362130138281],[-74.32822456931527,41.00116830132492],[-74.31555556569144,41.00237730229369],[-74.30949556290537,40.998417301609535],[-74.30168656038197,40.999181302228],[-74.29555355871817,40.994711300808646],[-74.29283455725724,40.98796329980215],[-74.29751455799489,40.98349229878661],[-74.29717655832185,40.97945129778255],[-74.28168955268288,40.97996929856715],[-74.27886655261689,40.975478298305966],[-74.2823085528522,40.96952029691502],[-74.27930355182141,40.96495129559787],[-74.28055955204819,40.958003294721344],[-74.27723854984599,40.954603293663595],[-74.27942254967266,40.94332729204774],[-74.28510555169554,40.931386288913934],[-74.28924755262216,40.928799288171234],[-74.28851255241105,40.924841287783025],[-74.28374955057718,40.92068228736764],[-74.28263854931188,40.9168882862031],[-74.27168254599948,40.91543328651418],[-74.26713454370076,40.91066528606854],[-74.27219654590192,40.90527628494515],[-74.27197654530337,40.897329283329285],[-74.26565054276932,40.892733281998325],[-74.26429054225787,40.886914281359644],[-74.25316953787136,40.88158128094348],[-74.24029153350274,40.88044428066566],[-74.2128505243642,40.86510227878337],[-74.19789051923014,40.85721727778691],[-74.1300174948672,40.81994627256062]]]},properties:{geoid:”34031″,name:”Passaic”,state_name:”New Jersey”,county_state_name:”Passaic County, New Jersey”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:84.32,”60_65k_diff”:696.41,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:483.91,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.05,”27_65k_eptc”:446.7,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:446.7,”40_95k_eptc”:544.74,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:446.7,”40_65k_no_eptc”:544.74,”60_65k_no_eptc”:1156.83,”27_95k_no_eptc”:446.7,”40_95k_no_eptc”:544.74,”60_95k_no_eptc”:1156.83}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-77.68133661652679,40.72976612072839],[-77.66199061025557,40.73775012381599],[-77.65257660827459,40.74492912475487],[-77.62472160017668,40.75226912750416],[-77.59335759082552,40.761255130312435],[-77.571940584346,40.76934113325809],[-77.55253957851517,40.77759913551319],[-77.5110985666112,40.793962140652575],[-77.43903554672366,40.82381814862581],[-77.40730353759903,40.83528215201964],[-77.37471052717227,40.84530315545199],[-77.36418252459318,40.846945156150674],[-77.33278451628661,40.870617162062594],[-77.31588951213224,40.88267816540372],[-77.27923850170617,40.909718172118325],[-77.20402948422715,40.99271819087431],[-77.14380646790283,41.042809202777185],[-77.14416246804348,41.04434620276905],[-77.22888949399498,41.019656194629285],[-77.33992752679038,40.98717518424204],[-77.39390954256415,40.978293180183584],[-77.44027655692517,40.97445617732955],[-77.50859857781533,40.962946172884315],[-77.55909659795796,41.02182618160649],[-77.58019660640514,41.047278185666514],[-77.56173860180414,41.057650188498364],[-77.56761460376039,41.06538518972202],[-77.57356760546625,41.06869019071825],[-77.58143060857985,41.0671231900238],[-77.58382360928177,41.070105189943654],[-77.59200361155033,41.07163518979877],[-77.59526461376832,41.07771919160285],[-77.61203261881728,41.08581719238576],[-77.62095062183742,41.08909519211474],[-77.62176162314695,41.09119319220884],[-77.64766863140379,41.098088193175066],[-77.65006963179478,41.09756119274326],[-77.6589726346975,41.10096319307401],[-77.66081463563386,41.1067661938964],[-77.66709463868197,41.108289193927384],[-77.67272463925927,41.10520819309569],[-77.68375364405394,41.10931419365094],[-77.69039164557795,41.10625719248045],[-77.69549264683319,41.10760819302981],[-77.70622765055117,41.11388019321437],[-77.7122686520328,41.1103541923635],[-77.7139436521951,41.10598319163378],[-77.7177616540986,41.1049621911566],[-77.72478665590998,41.10740119197107],[-77.73023965788235,41.11137619173249],[-77.73698866059884,41.10791419153098],[-77.74667766293173,41.106269190052394],[-77.77799867601325,41.14662019675145],[-77.78956567900762,41.14213519585456],[-77.79001168225135,41.177150201723755],[-77.89766971523474,41.17692619759371],[-77.89826472161619,41.252673212411246],[-77.9137897257285,41.24057320898228],[-77.92016972640222,41.229247206987736],[-77.92363372698925,41.226435205916474],[-77.9362637310915,41.226006205574244],[-77.93901073170079,41.22271520431608],[-77.93561773050477,41.21489920353034],[-77.93565873028422,41.21174920238878],[-77.94083573165746,41.209444201828255],[-77.95060873540105,41.213799202349676],[-77.95561773716706,41.21743520327474],[-77.95944073873329,41.21750520318219],[-77.96565273911182,41.20959220073573],[-77.97308074196793,41.204196199625464],[-77.97359074036278,41.18910119698582],[-77.970835738479,41.17832219518141],[-77.97301473917783,41.17302919365706],[-77.98418974305874,41.170244193159675],[-77.98671374252176,41.16380719170706],[-77.99027474399576,41.16171219133532],[-77.99791074660536,41.16337719088707],[-78.00179874724282,41.158141189626974],[-78.00033174634943,41.150958188497526],[-78.00357174640801,41.144864187414704],[-78.00910774785063,41.14332418638517],[-78.01202374932667,41.14507918687449],[-78.01447875039852,41.15200418788571],[-78.01735075198123,41.15319518858855],[-78.02859675531214,41.15033318691524],[-78.0349717574879,41.15392818736777],[-78.03817375791068,41.15361118726554],[-78.04344275944577,41.146516186239666],[-78.05273576252893,41.14532518529438],[-78.05483876214684,41.134185182787874],[-78.05884676267502,41.13091718206315],[-78.0655917658476,41.13234918266751],[-78.0704347669897,41.12898918112113],[-78.06866176562743,41.12431618029312],[-78.07373476745106,41.12206318016734],[-78.07767476870151,41.12517518013573],[-78.08414077103954,41.12595318041597],[-78.08644977075971,41.123581179350104],[-78.08759777096284,41.117181178329524],[-78.09037277185357,41.11564117790185],[-78.0947597741157,41.119674178628436],[-78.10034777607083,41.12179117923023],[-78.10870477806381,41.11765317790334],[-78.11225277829128,41.11364817726734],[-78.10761677642566,41.10551817572859],[-78.09811377269453,41.08604717175381],[-78.0926737706756,41.07957017090247],[-78.09575477004176,41.07091116984539],[-78.08563976725755,41.06865816977541],[-78.09065376747267,41.059420167186055],[-78.0846207665965,41.057400167668206],[-78.07556276374258,41.05966516783401],[-78.07285176182859,41.051930166454675],[-78.06820576035712,41.04996716678468],[-78.06236575866208,41.053238167023004],[-78.05938775774723,41.05084216716407],[-78.06408275924113,41.045921166037104],[-78.05726075617851,41.03935916529075],[-78.06562275822559,41.03578816418296],[-78.06927175909229,41.03272916326948],[-78.07616576201417,41.03448716325498],[-78.07990576253218,41.02948816235476],[-78.07560176091773,41.02219316057717],[-78.0678917581717,41.01949216097218],[-78.06983375797628,41.01470215950643],[-78.06200475555039,41.01327915970903],[-78.05595875359441,41.00828115910062],[-78.05616575273264,41.004264158402535],[-78.06514075630687,41.003346157902904],[-78.06185275436155,40.997908156964996],[-78.0681177568717,40.997653156320844],[-78.07361075758214,40.99394515537484],[-78.08470476123739,40.99090015451343],[-78.08183776024526,40.98542215374888],[-78.08443076103734,40.9808391529671],[-78.09052476238585,40.98088915281977],[-78.08814976135773,40.970329150767384],[-78.0840517595006,40.96773915036291],[-78.07774275658814,40.95883214837656],[-78.08150875722927,40.955072148135706],[-78.08957075977321,40.95446614717887],[-78.0949027612194,40.950444146266314],[-78.09926576255701,40.95159714621295],[-78.10421676393248,40.94952614578963],[-78.10998076618169,40.94955514557577],[-78.11133676681196,40.9451321449446],[-78.1202717689206,40.9419381440227],[-78.12703677134408,40.945689144100925],[-78.13406577318766,40.9472251440616],[-78.13062377296579,40.951349145112225],[-78.1363787744863,40.95602914605952],[-78.12996677384501,40.961849147070396],[-78.13197177401759,40.96591414767473],[-78.1363537756708,40.96602614789332],[-78.13644977485933,40.96142114729332],[-78.13965077636118,40.95711014613599],[-78.14106177656902,40.94985214430284],[-78.14772677828415,40.95005614456521],[-78.1468557787838,40.95659414511887],[-78.15160678021913,40.957374145135724],[-78.15850978271791,40.96093714619572],[-78.16512778448178,40.96160014543977],[-78.16897978509462,40.95962514553665],[-78.1676577849111,40.95193914337735],[-78.16272678264814,40.95469114416963],[-78.15941478194235,40.950374143886776],[-78.15581277972994,40.94144514223568],[-78.16245678161197,40.94207714195426],[-78.16646378306051,40.93669414136027],[-78.17128178447886,40.93677514079508],[-78.17148378422623,40.93242613997584],[-78.17794378654932,40.92915713878678],[-78.17987778597123,40.923567137987455],[-78.19043778924328,40.91868013630621],[-78.19598779126267,40.920000136972774],[-78.20163979274498,40.915821135750086],[-78.20941679547848,40.91738013552938],[-78.21981579829216,40.91274913414659],[-78.22594479931146,40.907408133206296],[-78.2288387995872,40.90107913156541],[-78.22133579691912,40.89217712998118],[-78.22122479724577,40.88876912914252],[-78.22793979864312,40.886741128658436],[-78.23004079931516,40.88030712719475],[-78.24298980283749,40.88148712739186],[-78.24776380410091,40.87956512690255],[-78.24647780439723,40.87585212644801],[-78.23972780233798,40.876914126833654],[-78.23611179988619,40.873263126401866],[-78.24897780366365,40.86952712501007],[-78.24922280315899,40.85539112242353],[-78.25735180535034,40.85542412163382],[-78.26717180874694,40.85027212018709],[-78.2738298105148,40.848063119165964],[-78.27773181179175,40.851001120010096],[-78.2842398138621,40.851057119589086],[-78.29131881608356,40.846756119006926],[-78.29060281556268,40.842528118070675],[-78.29443981651804,40.837927116446394],[-78.3019858183367,40.83350311575155],[-78.29997281756037,40.83142411556765],[-78.29938581731429,40.82456811447266],[-78.30562781841513,40.82064611346508],[-78.30801081919343,40.8157281124495],[-78.31163481978953,40.81390011153664],[-78.3137538201987,40.80856611047514],[-78.32047282228332,40.808207110518026],[-78.32692882377256,40.80590710956572],[-78.33166382534587,40.8011301084516],[-78.33947082781995,40.79794110729513],[-78.34025182756649,40.791570106193305],[-78.342581827671,40.790879105848454],[-78.34258082685874,40.78190310439554],[-78.3501498287854,40.7761141027577],[-78.35225482897566,40.76858710116539],[-78.35913583160405,40.76790310038936],[-78.3652588334038,40.76455309983941],[-78.373425835091,40.757561098487095],[-78.37664283573866,40.751969097086494],[-78.3730198349116,40.74990009717618],[-78.36639383189816,40.73605109408621],[-78.36062182975648,40.733189094202096],[-78.3400108224259,40.73354309473099],[-78.22173778581005,40.73938310124835],[-78.13183675797652,40.74302510495372],[-78.11652375307669,40.739135105435736],[-78.11621075307866,40.73938610570411],[-78.01074171792551,40.710371104513094],[-77.99334271235398,40.705215103926655],[-77.94425269584795,40.691565102996535],[-77.90464368536558,40.71074210828425],[-77.89428468248943,40.71621110982708],[-77.85922267214787,40.73082711393192],[-77.82490566159561,40.74354211798665],[-77.76855164283181,40.719474115569824],[-77.71867962783465,40.72738011902877],[-77.71055062461429,40.71457211670486],[-77.68133661652679,40.72976612072839]]]},properties:{geoid:”42027″,name:”Centre”,state_name:”Pennsylvania”,county_state_name:”Centre County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.84,”27_65k_diff”:188.06,”40_65k_diff”:330.38,”60_65k_diff”:1218.95,”27_95k_diff”:0,”40_95k_diff”:117.88,”60_95k_diff”:1006.45,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.42,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:648.48,”40_95k_eptc”:672.92,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:648.48,”40_65k_no_eptc”:790.8,”60_65k_no_eptc”:1679.37,”27_95k_no_eptc”:648.48,”40_95k_no_eptc”:790.8,”60_95k_no_eptc”:1679.37}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-75.44475282394303,39.35509693585271],[-75.41288581541893,39.37512094062556],[-75.40668681323933,39.380302941889504],[-75.40891281485129,39.38756994316727],[-75.41405781627803,39.38466094260306],[-75.41728981687798,39.38867894391539],[-75.4168668171022,39.3958699447437],[-75.40936281556448,39.3949209454089],[-75.40737381490115,39.39803994538624],[-75.41116381656146,39.40110094590427],[-75.40668381456665,39.40363894646735],[-75.4053558145679,39.40764394784405],[-75.40976881561261,39.40870994823517],[-75.41167681604338,39.40546094718746],[-75.41891281931349,39.41042494752174],[-75.41830581867846,39.41545294896932],[-75.41173381749634,39.42367595075478],[-75.41369081897062,39.42903695194116],[-75.41767982027154,39.42970095177506],[-75.4159888190614,39.43437195252799],[-75.40921381797203,39.44306495479705],[-75.41157081930687,39.445445955045194],[-75.41027481807343,39.45002295642606],[-75.41469281974511,39.45226695677514],[-75.40767981821888,39.458788957748894],[-75.40063681675707,39.4621729586733],[-75.38656481154798,39.45784495813857],[-75.37309880715968,39.45578695887467],[-75.36821480634282,39.456486958916386],[-75.36303980496604,39.46451496094963],[-75.35703180270721,39.47029496200122],[-75.35104180115152,39.47213396269229],[-75.34990980093355,39.47987296407758],[-75.34394380028814,39.48573396588813],[-75.34237779931935,39.490629966616254],[-75.32609079405005,39.48850196722084],[-75.31802179159821,39.49204796782877],[-75.30508978890867,39.503444970249646],[-75.29391178587264,39.511559972802175],[-75.27044477937487,39.53090697715936],[-75.23843577088746,39.5590469839632],[-75.17791774936916,39.52106897867374],[-75.11278372609075,39.47677897248179],[-75.0838247166219,39.45736196879124],[-75.08085671544764,39.46094996984875],[-75.08179771647737,39.46548597100651],[-75.08035371563736,39.47203097212806],[-75.07335871503761,39.485589975514664],[-75.07542271539064,39.489740975995595],[-75.07407471524805,39.49282197672948],[-75.07837871719137,39.49698197713924],[-75.07970071712356,39.501441978287],[-75.07664371702327,39.50783297971828],[-75.07801671745723,39.511991979976905],[-75.07560571737599,39.51894398192614],[-75.0729187160629,39.52189798260942],[-75.07339871706655,39.5267249830734],[-75.07106471698533,39.53245298483842],[-75.072642716717,39.53608298570493],[-75.0710487164748,39.53995498614558],[-75.0744587183984,39.54457198739878],[-75.06987271781922,39.55312698892462],[-75.06666271638964,39.556233989903454],[-75.0662877163405,39.56048299075506],[-75.06185571524799,39.568753991917795],[-75.07705572084431,39.57939199368372],[-75.10992773284912,39.603325997452636],[-75.19979476460819,39.66700400670331],[-75.21294676941305,39.66451200638528],[-75.2193747707489,39.66183000561467],[-75.22393177298777,39.66308500505683],[-75.23345477557088,39.6614380047638],[-75.24747577988437,39.66449400458014],[-75.25070578118712,39.66862800571761],[-75.25122778233515,39.67661600757918],[-75.26197078514454,39.68172400752399],[-75.26846978802641,39.682271007313425],[-75.27602279053916,39.680432007214186],[-75.28600079348728,39.6795960063291],[-75.29514679685767,39.686162007325244],[-75.30645280012415,39.689540008066544],[-75.31039480182429,39.68903800748629],[-75.31671580335603,39.691405008032596],[-75.32672180702605,39.690380007280744],[-75.32742380679463,39.696623008795726],[-75.3345838094952,39.69980500867344],[-75.33683581126692,39.70429900990095],[-75.34742981451429,39.7071160095282],[-75.35025381495625,39.71125501075545],[-75.3606178189232,39.7140310103799],[-75.36724082125572,39.717573011504456],[-75.36929482245344,39.72199301174676],[-75.376636824705,39.72658001262332],[-75.37481082527053,39.73716201457364],[-75.37862882677369,39.747038016196335],[-75.38584882880467,39.74697701611485],[-75.38790482995934,39.75176201766853],[-75.39184083058144,39.75001601707078],[-75.39466383235144,39.75312501745697],[-75.39117183071309,39.7553170182631],[-75.38996683064995,39.759667018604404],[-75.39611983329586,39.761388018534696],[-75.40320583514153,39.76126101818425],[-75.40596083647276,39.763492019029535],[-75.40492383638721,39.76905102026999],[-75.39736883405463,39.76924202023228],[-75.40039583470097,39.772978020999126],[-75.40010583536198,39.77736202204997],[-75.40232583667202,39.78247702301841],[-75.40592983697928,39.78113002268537],[-75.4075188376215,39.787248023714504],[-75.41351183946632,39.785019022931074],[-75.41739984099821,39.78563402333688],[-75.41933084148889,39.789733023821064],[-75.4054908380238,39.79637602586484],[-75.43830184789611,39.78441002195263],[-75.45029485078636,39.77528701985075],[-75.4523408515033,39.76902101815213],[-75.45944185354223,39.76581901765757],[-75.46392285469757,39.760771015833235],[-75.46355185387763,39.75702201509467],[-75.46939785462148,39.74286901269091],[-75.47555885611315,39.733540010281374],[-75.47652085526788,39.716109007103434],[-75.48188485703243,39.713694006328254],[-75.48838585872033,39.71471600578178],[-75.49631386051693,39.700964003414825],[-75.5065378635126,39.697271002471645],[-75.50929286493987,39.69420300104813],[-75.50925386342328,39.684871999698714],[-75.51219186437685,39.671774996439346],[-75.51600986510411,39.66576599532928],[-75.52183986694848,39.66099599437606],[-75.52783086761774,39.65307199206333],[-75.53352586938804,39.64756499127619],[-75.54197987208845,39.645432990068066],[-75.54853587322518,39.63777798872445],[-75.55426787545092,39.635573987699885],[-75.55877487590048,39.629994986890146],[-75.55890987592245,39.61849098401618],[-75.55697587413687,39.60758398197511],[-75.55339987229007,39.60177398092613],[-75.55031987206647,39.60077398107282],[-75.54214786902021,39.59452698007045],[-75.53128086555719,39.58870497961562],[-75.52769486333752,39.58411997883624],[-75.51806686082196,39.58284797873376],[-75.51277185870136,39.57829797783138],[-75.51196185718844,39.5672979757999],[-75.51814585956733,39.55669197395864],[-75.53341386336747,39.542051970523204],[-75.53196986223118,39.537172968886],[-75.52780086036954,39.53537196865466],[-75.52667286003503,39.53022296817846],[-75.53002386051547,39.51042196402218],[-75.53005285968447,39.50482496250536],[-75.52786285838252,39.49814696128328],[-75.54648786441903,39.49624996049828],[-75.55909186818916,39.49581395974567],[-75.5635878688975,39.48305595749206],[-75.56053986659349,39.455652952106966],[-75.53112685524965,39.43020494801769],[-75.4813618376742,39.38756294134767],[-75.46943783289059,39.37315493841724],[-75.44475282394303,39.35509693585271]]]},properties:{geoid:”34033″,name:”Salem”,state_name:”New Jersey”,county_state_name:”Salem County, New Jersey”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:84.32,”60_65k_diff”:696.41,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:483.91,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.05,”27_65k_eptc”:446.7,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:446.7,”40_95k_eptc”:544.74,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:446.7,”40_65k_no_eptc”:544.74,”60_65k_no_eptc”:1156.83,”27_95k_no_eptc”:446.7,”40_95k_no_eptc”:544.74,”60_95k_no_eptc”:1156.83}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-75.1684637190217,39.056186884986495],[-75.19167272758422,39.079007889209926],[-75.2190767390366,39.115954895513305],[-75.2490187503392,39.15895290296737],[-75.30052277053011,39.2252819146801],[-75.32102277923687,39.25138691881281],[-75.38113180042014,39.30085292743444],[-75.40182180761906,39.31829392995851],[-75.44475282394303,39.35509693585271],[-75.46943783289059,39.37315493841724],[-75.4813618376742,39.38756294134767],[-75.51177884619055,39.36603793521713],[-75.51597684702847,39.364370934864475],[-75.51689884719919,39.36099593407035],[-75.5214218479189,39.35861493344312],[-75.52845484986008,39.35831293317277],[-75.53585085285684,39.35062493195349],[-75.54326485443023,39.35324393197732],[-75.54521785550828,39.35077093142699],[-75.5573798594612,39.34910893031886],[-75.56052085963113,39.345074929407886],[-75.55735985899538,39.3415089291669],[-75.55620685764345,39.33533292806377],[-75.5648078601699,39.33194392678233],[-75.56900886083473,39.32875192604759],[-75.56871786070096,39.32353092511672],[-75.57443086167224,39.31361892254676],[-75.58434286503793,39.30872592144746],[-75.59133686730519,39.31164592133041],[-75.59496486843953,39.309934921324164],[-75.60659987190148,39.30809792046265],[-75.61963287665046,39.31006592078084],[-75.62576587736699,39.30415391882327],[-75.6325928799449,39.30128091863297],[-75.64084288228106,39.30146191802147],[-75.64845188494728,39.295442916576675],[-75.6511608851393,39.29160191568583],[-75.6604778877597,39.29167991492333],[-75.66727089049712,39.2904249146512],[-75.67556289279321,39.290660914274035],[-75.68026289409772,39.292503915114],[-75.68518989656324,39.29709691568285],[-75.71490290499007,39.29937391442228],[-75.7600759199095,39.296826912337124],[-75.7537959133324,39.21876889725952],[-75.74195290046288,39.07063586765069],[-75.73490389253081,38.982274850467945],[-75.72279888061315,38.829858819474985],[-75.68317586752445,38.83132382112899],[-75.58488583752033,38.834560825373295],[-75.55501482835044,38.835656826830615],[-75.54872782653419,38.841084828421046],[-75.53958182352586,38.843641829034226],[-75.53623582357514,38.84989782986332],[-75.5204408188665,38.85574983245253],[-75.50974681668359,38.87500483668676],[-75.50816981545758,38.878958836849826],[-75.49688981266267,38.88300883796701],[-75.49438481190877,38.887889839706105],[-75.48802781076661,38.89279184082606],[-75.48815781111084,38.898990841806835],[-75.4858348106516,38.903560842603056],[-75.47722380803515,38.90584884411471],[-75.46534480406915,38.911272845551046],[-75.45684380176752,38.909719845362176],[-75.44418879805923,38.91307584630112],[-75.43470979425246,38.91089984641244],[-75.42979479291361,38.91358984743335],[-75.4246937915065,38.91342584744845],[-75.41670178969044,38.918025848195164],[-75.40881978691732,38.916831848568634],[-75.40839578686308,38.92008684865333],[-75.39911078397975,38.92691785109655],[-75.40095178479463,38.92948885091475],[-75.3986147848385,38.933524852336426],[-75.40287478632263,38.937457852995266],[-75.39850478543559,38.94080185323795],[-75.40104178572834,38.94703885497979],[-75.39361678398329,38.952853856027495],[-75.38252678096306,38.95591385744306],[-75.38134078085913,38.96129285877735],[-75.37213277775575,38.96144385866856],[-75.36788777658701,38.95958785834385],[-75.36620977618006,38.953942857187755],[-75.36102677388863,38.957540858166794],[-75.35277577124413,38.94793285687166],[-75.34406276866355,38.95527685883006],[-75.34217576845253,38.951442858140226],[-75.34351776868573,38.947446857338115],[-75.33679876645495,38.94654285675197],[-75.33244576461773,38.95071485819224],[-75.3246367622067,38.94971785763554],[-75.321267761981,38.95346285883837],[-75.31353575836603,38.950437858840445],[-75.31207975876005,38.94587285755729],[-75.13846270644503,39.002704875121516],[-75.14282870824489,39.01149487665068],[-75.1684637190217,39.056186884986495]]]},properties:{geoid:”10001″,name:”Kent”,state_name:”Delaware”,county_state_name:”Kent County, Delaware”,”27_22k_diff”:66.19,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.84,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:106.11,”40_65k_diff”:230.44,”60_65k_diff”:1006.71,”27_95k_diff”:0,”40_95k_diff”:17.94,”60_95k_diff”:794.21,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.42,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:566.53,”40_95k_eptc”:672.92,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.19,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.88,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.87,”27_65k_no_eptc”:566.53,”40_65k_no_eptc”:690.86,”60_65k_no_eptc”:1467.13,”27_95k_no_eptc”:566.53,”40_95k_no_eptc”:690.86,”60_95k_no_eptc”:1467.13}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-74.88982073566775,40.78773723969704],[-74.89553273759199,40.78400023891787],[-74.90396273991213,40.78115423793804],[-74.90271973840893,40.77184423602066],[-74.91330374126801,40.76655523464057],[-74.91523374245946,40.76244823386102],[-74.92264174411788,40.75665523195119],[-74.92694074544478,40.75494923182524],[-74.9307367465363,40.74915623057418],[-74.9465257505752,40.73481922727235],[-74.95172875172636,40.72774822561585],[-74.95832475309909,40.72543522510663],[-74.9635107549182,40.72047622347372],[-74.96804875632928,40.711332221955395],[-74.97011375623998,40.709870221596425],[-74.98001675938741,40.7105552212529],[-74.9818527603257,40.70566722012421],[-74.99076976230322,40.70323921897888],[-74.99614176360059,40.70002921880575],[-75.00244776557963,40.69383921726222],[-75.01411776902911,40.692784216139096],[-75.02318277151976,40.69095821569033],[-75.03402777497936,40.68357721409035],[-75.03766477633002,40.68363521366605],[-75.04405177811695,40.67872321250417],[-75.04916177979362,40.67947221220758],[-75.06019878274962,40.67304021128583],[-75.06208878269629,40.66975121034178],[-75.06825078509456,40.66861520979601],[-75.0772077880364,40.663333208317134],[-75.08200578918714,40.65770020746245],[-75.0889867905509,40.65540920636805],[-75.09625979299362,40.64797720426376],[-75.10598879574195,40.644589203388],[-75.10836079562009,40.6397622027126],[-75.11386779708123,40.637281201604566],[-75.1274868021831,40.63445020043131],[-75.13633580444959,40.63015819941024],[-75.1436828069393,40.629462198952886],[-75.14818880767088,40.6256341987855],[-75.14966880817033,40.620509197597464],[-75.15442081006442,40.621700197075626],[-75.16119781180717,40.61821119681335],[-75.16305981187516,40.61097519517387],[-75.17369681492465,40.6032131934442],[-75.17488781399793,40.59893419257653],[-75.18088881647712,40.59719519204939],[-75.18099081634631,40.59421219093415],[-75.18960181860332,40.59178419017929],[-75.18969381798873,40.58767918989849],[-75.19415182010557,40.58285118858486],[-75.19549782030921,40.57863518703029],[-75.18827181666082,40.570555186373724],[-75.18125281463931,40.566723185254055],[-75.17287881228086,40.56443118551487],[-75.16231580805844,40.56420118575598],[-75.15785380661316,40.565432185918276],[-75.14875880410855,40.571827188072575],[-75.1401738016437,40.57537818924043],[-75.13499680039676,40.575670189497686],[-75.11553779418186,40.5728681896667],[-75.09982878824623,40.5674061890322],[-75.07513977893316,40.54558718552901],[-75.06810177664502,40.54149618469968],[-75.065091775338,40.52628618197333],[-75.06568977464873,40.522114180748964],[-75.06484377347168,40.5035111774267],[-75.0625777721967,40.494082175798276],[-75.06276277200092,40.48003417339753],[-75.06771677216157,40.473677171439256],[-75.06701777235786,40.465316170327995],[-75.07060977276417,40.45620416848184],[-75.06651677062334,40.447184166099944],[-75.0609187672136,40.42174516134633],[-75.05762076647699,40.41734416115614],[-75.04552776197731,40.41368716091873],[-75.03177975692786,40.40482115895903],[-75.02302975368815,40.403701159295224],[-74.99586174621854,40.4103921621123],[-74.98841474291659,40.40850216185527],[-74.9831327408949,40.40460716144947],[-74.96750073652979,40.39882116095418],[-74.96443273547577,40.39595616005761],[-74.96147973314658,40.38894315840807],[-74.95578673097813,40.38003615716636],[-74.94712372708234,40.360217153729764],[-74.94451872557475,40.34507115032733],[-74.94291072506262,40.34169115003049],[-74.932278721511,40.33943515027951],[-74.85626369719441,40.34670415403421],[-74.86967970383932,40.377782159612416],[-74.80201768251733,40.38498016379092],[-74.80847168615138,40.416672169440076],[-74.74814866781051,40.42416417347584],[-74.78042768214777,40.4841711842898],[-74.79784268920197,40.5155651894202],[-74.78721768548773,40.512001188978005],[-74.78139468326484,40.505009187735986],[-74.77598068151237,40.50361418786222],[-74.74266067436167,40.5539061987039],[-74.730703671464,40.56359220095992],[-74.72459866911538,40.56619220181551],[-74.7131516665838,40.58391120581298],[-74.72493867016476,40.58876320671274],[-74.7185836691315,40.5996642086056],[-74.72175367030871,40.600710208778736],[-74.7133016688128,40.61210521177697],[-74.71147766798609,40.611540211477376],[-74.7027046654971,40.62112521368044],[-74.71154666802964,40.625046213951535],[-74.71327866921601,40.63062421501885],[-74.72654567427173,40.63241821497707],[-74.72765967427723,40.636241215546136],[-74.7229526733929,40.63894021652095],[-74.72363567390788,40.64776821856984],[-74.71956967280735,40.65414521967777],[-74.72755367536811,40.658622220326855],[-74.73059567710861,40.66574522171679],[-74.72270267458964,40.67009822271951],[-74.72160767532286,40.67877922433831],[-74.71774567364683,40.683996225435365],[-74.72393967692054,40.68784522596548],[-74.72115767558896,40.69158422642268],[-74.7207326758628,40.69683822741376],[-74.71662867449986,40.69869522831437],[-74.7168876754346,40.704861229318404],[-74.72014167693796,40.706485229794104],[-74.72215367734796,40.71601323188041],[-74.72566767856841,40.719540232540545],[-74.73733468302223,40.72162723208971],[-74.75290168894578,40.73113723304891],[-74.77099069453105,40.73605623364407],[-74.79367770156144,40.74034723367741],[-74.79797470356144,40.74219423362715],[-74.80822970706598,40.7411502332367],[-74.81706970965719,40.74289923298157],[-74.82363271217757,40.74221823310362],[-74.82748571293311,40.74408023362877],[-74.84302571926975,40.756029235074685],[-74.84406971958482,40.75859223497593],[-74.88982073566775,40.78773723969704]]]},properties:{geoid:”34019″,name:”Hunterdon”,state_name:”New Jersey”,county_state_name:”Hunterdon County, New Jersey”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:84.32,”60_65k_diff”:696.41,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:483.91,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.05,”27_65k_eptc”:446.7,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:446.7,”40_95k_eptc”:544.74,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:446.7,”40_65k_no_eptc”:544.74,”60_65k_no_eptc”:1156.83,”27_95k_no_eptc”:446.7,”40_95k_no_eptc”:544.74,”60_95k_no_eptc”:1156.83}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-74.99171978728133,41.09229229512348],[-74.97998678481467,41.11051529880122],[-74.97359178267516,41.11319429921634],[-74.96323477948313,41.114684300332435],[-74.94811377532336,41.123200302086744],[-74.94449977513176,41.12998230386473],[-74.93114777098627,41.13374230526721],[-74.9244707688835,41.13753830618384],[-74.9052577644432,41.15567631031102],[-74.90073976268518,41.16519731211815],[-74.8899897602379,41.173225313786084],[-74.88233275887643,41.18082931623074],[-74.8790267579908,41.186519316692575],[-74.8747947573105,41.19724731942597],[-74.86897975615628,41.206126321377006],[-74.85947475363075,41.21878132404941],[-74.86083875353667,41.22232632455106],[-74.86743875674972,41.2274283258417],[-74.86617475658244,41.23270132606037],[-74.86233575573938,41.23743932719478],[-74.86111875586262,41.24365332884987],[-74.85567075425728,41.250139330376655],[-74.8496187521527,41.25112233099044],[-74.84488475084702,41.25813833182708],[-74.84645675217196,41.262421332706886],[-74.84044175035011,41.27199233524771],[-74.83778875063497,41.27801733633676],[-74.83034874839414,41.28707333828771],[-74.82121274587499,41.29432133996029],[-74.81203474285957,41.29816634146788],[-74.80742974168739,41.302820342107054],[-74.79192373733228,41.31121834462583],[-74.79607073924886,41.319611345515725],[-74.79158573844181,41.323027346438224],[-74.78414073599781,41.32429334749309],[-74.77265873298373,41.32478934752068],[-74.76348673035191,41.33127934954884],[-74.76082273002328,41.339518350580576],[-74.75609372899716,41.34519835183622],[-74.75239972740916,41.346544352966916],[-74.7259527186385,41.34620035329603],[-74.71762371637949,41.3485733545044],[-74.70953271371309,41.352334354850704],[-74.70009871112774,41.35466335634183],[-74.69558171005325,41.35761535692806],[-74.6897557085388,41.361755357490665],[-74.69003170884105,41.365237358403704],[-74.69410571079334,41.37011335904567],[-74.707307715277,41.37810136041365],[-74.71230971700778,41.38834836182685],[-74.7194817196846,41.394536363008],[-74.72902972264438,41.3953393625056],[-74.73601172509625,41.39833836282405],[-74.74122072733505,41.40543336465063],[-74.74173672777712,41.40878536469627],[-74.73486472658078,41.4219123676971],[-74.73720472748882,41.429774369226045],[-74.74145772909098,41.4311623688967],[-74.75093773197807,41.42786536832251],[-74.75447273275073,41.42496136780008],[-74.7615617355739,41.42319136709707],[-74.77270873888781,41.42635036757614],[-74.78828774331788,41.42149936594044],[-74.79423174582772,41.42285936594008],[-74.79925774764725,41.43081436731952],[-74.8014047487336,41.43867836853053],[-74.80515975063079,41.44186136861592],[-74.81248975230315,41.44281036928059],[-74.82258575630941,41.437022367158356],[-74.82685975655262,41.43140036604469],[-74.83585876022255,41.43110336597934],[-74.85391076615781,41.443154367296636],[-74.86314376960325,41.44439536757419],[-74.8793897740645,41.439804366040214],[-74.88901177761629,41.43817336525617],[-74.8951297795714,41.43934336471802],[-74.89485677989398,41.4461993662142],[-74.88909977807135,41.45143836786853],[-74.8903097781613,41.455817368808546],[-74.89476978064904,41.45815336879428],[-74.90655478367076,41.46088436871986],[-74.90954478550672,41.473243371130145],[-74.91303678708135,41.47602537151264],[-74.92283679080451,41.47694037109836],[-74.93276679368739,41.48245237237137],[-74.9434167981216,41.48368937195242],[-74.94808179909703,41.48063337105505],[-74.95823180195949,41.4765893701633],[-74.96698580495341,41.47704536987637],[-74.98180580981244,41.4799573696332],[-74.985630810923,41.48689137071136],[-74.9822718104634,41.4986933729861],[-74.98364081180003,41.50526337413349],[-74.98749281387867,41.50882737468585],[-75.0007348180159,41.50739437429248],[-75.00371681826225,41.51159037530201],[-75.00095781814554,41.517601376152676],[-75.0032138198566,41.52348937728153],[-75.00801882172108,41.52748237771773],[-75.0167988241885,41.53220337792277],[-75.02270082653446,41.53301137868028],[-75.02470182796631,41.54013937991641],[-75.01646782496677,41.54335438011191],[-75.01880582612006,41.552444381746255],[-75.02843683003844,41.564611384206884],[-75.03318983185372,41.56507738402586],[-75.04049183467001,41.56969638498226],[-75.0439058362459,41.57471038589101],[-75.0472478376125,41.583690387192775],[-75.05293584004,41.587902387514795],[-75.06001384173031,41.59082138810379],[-75.06956084631189,41.601882389725894],[-75.09746685222011,41.566215381483175],[-75.10982885547489,41.551052378317756],[-75.12461785914262,41.53185937456616],[-75.16894486874119,41.47510936197387],[-75.17792387110015,41.46538735934803],[-75.1783558709969,41.461961358585214],[-75.18763687380384,41.45825235755934],[-75.18691887304408,41.45359135700118],[-75.18928587339401,41.44726735570923],[-75.18623787259548,41.44284435528641],[-75.19138187407255,41.438902354179504],[-75.19942187671418,41.43753635313231],[-75.19962987622601,41.43365135301268],[-75.20686187857176,41.43095335168361],[-75.21831688150212,41.424125349878594],[-75.2295188858653,41.42497935021844],[-75.24234788930696,41.42131934837994],[-75.25008689117914,41.41822734792362],[-75.25179789136065,41.41046934669578],[-75.24843489037085,41.40849134621179],[-75.24681088975325,41.402443345111315],[-75.25490689221785,41.39913534393123],[-75.25671089216056,41.394073343145],[-75.25308489032504,41.3913023421206],[-75.25507489056659,41.38699434200121],[-75.2619058923322,41.381962340597426],[-75.26263489325046,41.37509733883289],[-75.26571389291506,41.37239033887329],[-75.27829489750037,41.372489338033134],[-75.29814990320396,41.367293336562504],[-75.30606190669961,41.37423133754844],[-75.30906890765222,41.37468733724181],[-75.31429390822377,41.36861433587826],[-75.32365891175681,41.366053335519226],[-75.33067191416852,41.36960133506279],[-75.3377599170202,41.376260336793706],[-75.35064992083129,41.367702334362725],[-75.3464159179517,41.35728933226503],[-75.34204191674901,41.35527533211749],[-75.336752913986,41.345502330703894],[-75.34435791684828,41.341036329279795],[-75.34297891596945,41.33609732827783],[-75.32938191117374,41.335550329072184],[-75.32595791051399,41.34068333025532],[-75.32245190907493,41.34004833053448],[-75.31755390746828,41.33467332939602],[-75.31114490550351,41.33144732884627],[-75.31205190537841,41.32113132652273],[-75.31626890597275,41.315985325361446],[-75.31356490434682,41.31270532509839],[-75.31500090484333,41.30906532477796],[-75.32228290670975,41.299890322404345],[-75.32761090870744,41.29901632209708],[-75.3278139085912,41.295330321095506],[-75.3246089069467,41.288885319944505],[-75.32975790853102,41.28558431967719],[-75.33364590909751,41.279455318326725],[-75.33172590825484,41.27519831759509],[-75.33460490883935,41.26972831604154],[-75.34724691200435,41.26603831490596],[-75.35013691336232,41.25954431355456],[-75.34439791154658,41.257849313778244],[-75.34136590934745,41.254458312735125],[-75.34491391042774,41.249302311983],[-75.35049791215027,41.244397310735735],[-75.35918591495425,41.239214309331466],[-75.24208787747756,41.245898314872605],[-75.1297228424135,41.25210932030635],[-75.14788084311895,41.18222430605277],[-75.15650884454317,41.150349300182725],[-75.10599482717312,41.144209300845674],[-75.07681281797053,41.14113030079367],[-75.03921780269076,41.08880529275467],[-75.03259479966785,41.08527529167501],[-75.0250027979941,41.08352529145997],[-75.01854879526348,41.084896292385054],[-75.01260379375141,41.083809292260746],[-75.00317879104723,41.091781294024564],[-75.00031478961411,41.08949329393185],[-74.99171978728133,41.09229229512348]]]},properties:{geoid:”42103″,name:”Pike”,state_name:”Pennsylvania”,county_state_name:”Pike County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.83,”60_35k_diff”:131.84,”27_65k_diff”:203.19,”40_65k_diff”:348.82,”60_65k_diff”:1258.11,”27_95k_diff”:0,”40_95k_diff”:136.32,”60_95k_diff”:1045.61,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.41,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:663.6,”40_95k_eptc”:672.92,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:663.6,”40_65k_no_eptc”:809.24,”60_65k_no_eptc”:1718.53,”27_95k_no_eptc”:663.6,”40_95k_no_eptc”:809.24,”60_95k_no_eptc”:1718.53}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-75.48314200543223,41.999259448848285],[-75.63476805400056,41.99877344339697],[-75.76468509621793,41.99786443818571],[-75.8332151184392,41.99818743558067],[-75.98308416582238,41.99904342995559],[-76.1455212183487,41.99885042295573],[-76.1399662113675,41.937011411775124],[-76.13681520855663,41.906742406334565],[-76.13404820571446,41.873596400362196],[-76.1256131961511,41.78032238316419],[-76.12590119614677,41.77062238076665],[-76.12462019518676,41.766923380422135],[-76.11953718897172,41.710438369836226],[-76.11517418356637,41.65183335871219],[-76.11422618345833,41.64339335801251],[-76.08776117434924,41.644732359030186],[-76.01430615078603,41.64427736162385],[-75.98630614225289,41.64480936312621],[-75.97273113852145,41.644325363190724],[-75.87901110845353,41.643470366907664],[-75.86872610508956,41.644364367565544],[-75.83189009254183,41.6431503680604],[-75.79733808184567,41.64262336949335],[-75.79222207951375,41.64205836976743],[-75.76792607296244,41.64341737102821],[-75.71988905655843,41.64227137243547],[-75.65218903573849,41.64220437549063],[-75.50201198706773,41.6414503804131],[-75.46241297497549,41.641595382526575],[-75.46705198121998,41.72239639739235],[-75.47014298538085,41.772114407152905],[-75.4744679924526,41.8519634216627],[-75.47674399496942,41.87755442655227],[-75.48067500191777,41.958359441619926],[-75.48314200543223,41.999259448848285]]]},properties:{geoid:”42115″,name:”Susquehanna”,state_name:”Pennsylvania”,county_state_name:”Susquehanna County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.83,”60_35k_diff”:131.84,”27_65k_diff”:110.27,”40_65k_diff”:235.51,”60_65k_diff”:1017.48,”27_95k_diff”:0,”40_95k_diff”:23.01,”60_95k_diff”:804.98,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.41,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:570.68,”40_95k_eptc”:672.92,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:570.68,”40_65k_no_eptc”:695.93,”60_65k_no_eptc”:1477.9,”27_95k_no_eptc”:570.68,”40_95k_no_eptc”:695.93,”60_95k_no_eptc”:1477.9}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-79.99801728452181,39.98332988111519],[-79.99089728275648,39.986561882093085],[-79.99430528460212,39.99721688409872],[-79.99572928518226,40.00510488598127],[-79.9935692851997,40.00913688665363],[-79.98517028261257,40.0131088877038],[-79.97141027847151,40.013817888658764],[-79.9632012752982,40.00797488806528],[-79.95902327321177,40.000033886462106],[-79.95462327194544,39.99528188568038],[-79.94673526955285,39.99425788585087],[-79.93452626601346,39.99963388734829],[-79.92978926549868,40.011752889499896],[-79.92484726390845,40.01613189077043],[-79.91432326150776,40.021044892559985],[-79.904326257932,40.022540892822796],[-79.8899572543248,40.02246989397173],[-79.87999525151766,40.028289895118036],[-79.87621925054127,40.03376189687175],[-79.87868325146773,40.03822589692225],[-79.89046025580107,40.04536089797441],[-79.89161225594476,40.04942489863767],[-79.88110025348597,40.05780890113873],[-79.87894025346634,40.06304090169241],[-79.88511625548477,40.068560902513056],[-79.89615625893872,40.07048090234184],[-79.90153326128058,40.073600903107135],[-79.8995482606175,40.078448904117494],[-79.89439625929072,40.080272904550206],[-79.87974025424373,40.07870490461078],[-79.87156325174632,40.075456904259475],[-79.86245924893684,40.075664905087955],[-79.84937024569135,40.07955290596181],[-79.84261824355957,40.08379290739508],[-79.83927424273114,40.09248090901519],[-79.84338624557182,40.09969691079568],[-79.84913124828374,40.112623913048054],[-79.85253924929364,40.116111913011025],[-79.86005925159309,40.11884791379447],[-79.87786725799504,40.12696691393126],[-79.88550026063956,40.129503914072],[-79.88878026171437,40.1326559149698],[-79.89324426296885,40.14078391648518],[-79.90207726701055,40.14865491718047],[-79.90489326828848,40.15423891802206],[-79.90199726737153,40.16137492026402],[-79.89330926498752,40.16499092068096],[-79.88734026302495,40.16499092078114],[-79.87042825765676,40.162094921456074],[-79.86415625562607,40.16182292135509],[-79.85601125383988,40.165806922382465],[-79.85135525224142,40.17215892371249],[-79.85037925306689,40.17731092478626],[-79.85445925544325,40.191262927655096],[-79.86582025869889,40.197038928694425],[-79.87142826030298,40.197398928220785],[-79.88111826350074,40.19665492767314],[-79.88874226602145,40.19474092712124],[-79.90033726910772,40.194848926698675],[-79.91078627322004,40.19698492624026],[-79.91871527505526,40.20028692634159],[-79.92929227933492,40.20708892765724],[-79.95038528662255,40.211566927522625],[-79.95794328847447,40.214266927698084],[-79.96685229264989,40.2220959284849],[-79.97091929372661,40.22690092972703],[-79.97004529371681,40.23331193055233],[-79.9625962921898,40.23877593193374],[-79.95683729048837,40.240205932735066],[-79.93759328464775,40.24152693384277],[-79.92525928117466,40.24506893481221],[-79.91446427833631,40.25245093641893],[-80.02663531510112,40.285452938093975],[-80.08291333392575,40.30252093958947],[-80.10971534304369,40.31028393990169],[-80.18460636712668,40.33314694079266],[-80.20019937378541,40.34716094248926],[-80.22193238166281,40.36509394538978],[-80.2961974090554,40.42548395299482],[-80.31284841483746,40.43937095541137],[-80.36080443222788,40.47759896013245],[-80.39351644250593,40.47729395910577],[-80.43817845604087,40.47779095700122],[-80.46680546513859,40.47734895586173],[-80.5190414809271,40.477370953392786],[-80.51769247961826,40.46222495046447],[-80.51809447561749,40.39857593850942],[-80.51797347249074,40.36666393291798],[-80.51897847233393,40.34979692928258],[-80.51899446771539,40.29419091914709],[-80.5191374591661,40.172326895002406],[-80.51889845402917,40.117711885307855],[-80.51925045326396,40.09532888056521],[-80.51896345117765,40.06820887522699],[-80.5192674488511,40.045409870745644],[-80.51909444277933,39.962207855205236],[-80.50988544032583,39.95930685475578],[-80.5021524373651,39.95416885421142],[-80.49977043689351,39.95760585540199],[-80.48662343313202,39.9602298564564],[-80.49074043425456,39.95532085475689],[-80.47528042933043,39.9520728554003],[-80.46611842716138,39.956810856495174],[-80.46360342618611,39.96091285760635],[-80.45870042472254,39.96408885772531],[-80.46129742643994,39.96738885836987],[-80.45638442416471,39.969404859378486],[-80.45391142381371,39.97310885990505],[-80.44697842158203,39.97115985988548],[-80.44300342110134,39.97607586083898],[-80.43479041850303,39.977512862061914],[-80.42976341730585,39.97584486151484],[-80.42538241462485,39.971887860791945],[-80.41995541345787,39.975423862018474],[-80.41292441194179,39.97696286254143],[-80.40671641034915,39.976763863199196],[-80.40169040871668,39.97868286300317],[-80.39647840697343,39.97789786383014],[-80.39578140730796,39.98352486497414],[-80.39060640536687,39.98837186612512],[-80.37950840271554,39.994132867579296],[-80.36907639983373,39.997196868450835],[-80.35432739509248,39.99730186865283],[-80.3517693951141,40.00015486943617],[-80.32835938737733,40.004711871930745],[-80.3210583858453,40.00562787192443],[-80.31257138230916,40.00330087206078],[-80.30911738226519,40.00585787239372],[-80.31021638308131,40.01766187510216],[-80.30139938040212,40.02056687587533],[-80.29441337784236,40.018554876127595],[-80.28742437656835,40.01921387627995],[-80.28484837514674,40.01263687496705],[-80.2732583713609,40.01328787579633],[-80.27196937081699,40.0077368749699],[-80.27503637144297,40.003560873806194],[-80.26659536852152,40.00169787344317],[-80.25293936511132,40.0051918746875],[-80.25175836385559,40.00779087554824],[-80.24430336168379,40.00705287596891],[-80.24014136064835,40.00948387649625],[-80.22564335613,40.00753387673097],[-80.2228133553759,40.00466987576961],[-80.21479535247855,40.00281187586705],[-80.20821235090008,40.005119876572905],[-80.19944334738283,40.00320387659746],[-80.19389334603328,40.00492087730274],[-80.19123634501113,40.001938876587985],[-80.18241734255642,40.00323887730971],[-80.18126634249231,40.006599878445016],[-80.17592434117547,40.008145878426696],[-80.16045933634993,40.003346878474396],[-80.1552743343635,39.996549877665785],[-80.150986332874,39.99442087727096],[-80.13641232772036,39.99259487720348],[-80.12951332551486,39.98841387705936],[-80.11831132201404,39.99129687819874],[-80.11128831950494,39.98817487728055],[-80.10573531804295,39.99096387814929],[-80.09211731408313,39.992016879316814],[-80.08611731236522,39.99032087902004],[-80.06799530702447,40.00292188220571],[-80.060317305745,40.00946088348026],[-80.05480430396408,40.00429788311617],[-80.04717130168571,40.00513088334372],[-80.04386029896979,39.994532881846055],[-80.05028630096884,39.990149880418166],[-80.04785929979363,39.984760879668215],[-80.04893729987988,39.97926887856549],[-80.03978129696563,39.9741078783723],[-80.03194029427982,39.977698878915966],[-80.03371129487277,39.98333587996504],[-80.02825829368155,39.98303388033254],[-80.01802029071354,39.9774968791331],[-80.01100728849738,39.983205880675925],[-80.00693028767851,39.98470688154405],[-79.99801728452181,39.98332988111519]]]},properties:{geoid:”42125″,name:”Washington”,state_name:”Pennsylvania”,county_state_name:”Washington County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:26.92,”60_65k_diff”:574.51,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:362.01,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:399.63,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:399.63,”40_95k_eptc”:487.34,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.87,”27_65k_no_eptc”:399.63,”40_65k_no_eptc”:487.34,”60_65k_no_eptc”:1034.93,”27_95k_no_eptc”:399.63,”40_95k_no_eptc”:487.34,”60_95k_no_eptc”:1034.93}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-77.35663051877414,40.80734214893679],[-77.32164150936067,40.81711015213323],[-77.2436384848722,40.832017158695024],[-77.12957645132688,40.8538021673612],[-77.07406043394893,40.86834117189172],[-77.05202942782067,40.86939517331683],[-77.0432574245809,40.863674172767084],[-77.03186642067621,40.86412217241912],[-77.02490341859709,40.857497172047765],[-77.0198754162516,40.857937172491035],[-77.01547541574035,40.86093217264284],[-77.01131141489715,40.86877617414526],[-77.00483041286827,40.8721371756581],[-76.99535940964165,40.872728175940644],[-76.99366240995961,40.87514717690038],[-76.9731654030328,40.877140178106536],[-76.97001140271976,40.880936178315594],[-76.94714739574438,40.88576718027199],[-76.94070839399488,40.88803118133647],[-76.92779838970483,40.88739418106972],[-76.91923738643929,40.885198181033786],[-76.90528538249399,40.88497618224403],[-76.89124337835139,40.88866918352235],[-76.878152373982,40.884507183220514],[-76.85905836811389,40.889149184090265],[-76.85196636505776,40.888687184759426],[-76.84986836426604,40.88643618416462],[-76.84127036145634,40.886897184822146],[-76.83427136036109,40.889575185618604],[-76.82555735735393,40.88800318583532],[-76.80797635048505,40.87859318409021],[-76.80166234906407,40.879376184593305],[-76.80024434817499,40.88200218499756],[-76.80649935060839,40.88601118591815],[-76.8226813563192,40.889707186154865],[-76.85147136694474,40.91285418973946],[-76.85992737052514,40.923986191127106],[-76.86979337451783,40.94212919390423],[-76.87622337802891,40.95109719541816],[-76.87739937838916,40.96015319714789],[-76.88225138027211,40.96877119853387],[-76.88187738053867,40.97310919939926],[-76.87558937907447,40.9845902024704],[-76.87011537868129,40.99194220350801],[-76.86758637812376,40.99847620474532],[-76.86743237815945,41.00775720656113],[-76.8647243783578,41.020360209413134],[-76.86125137798481,41.02849721144122],[-76.86129537831782,41.03806821301012],[-76.85776237743225,41.04407221452864],[-76.85619437841603,41.050553215154466],[-76.85757837821086,41.05553821690606],[-76.85698737986799,41.06602521867443],[-76.85833738000946,41.073086219838736],[-76.86520438261685,41.080235220972106],[-76.87271238541193,41.08271022122695],[-76.88438538982129,41.09376122310708],[-76.88968739154126,41.10132122418059],[-76.89588439586669,41.11998622726915],[-76.89792139669956,41.13298822941407],[-76.8961163969011,41.139078230926486],[-76.96023141789424,41.14880922992035],[-76.96792341837731,41.12157722488631],[-76.97794141940466,41.08789121781746],[-77.0682384478852,41.0852392141006],[-77.11384146112556,41.06904020904809],[-77.14411346978856,41.06884820776083],[-77.14416246804348,41.04434620276905],[-77.14380646790283,41.042809202777185],[-77.20402948422715,40.99271819087431],[-77.27923850170617,40.909718172118325],[-77.31588951213224,40.88267816540372],[-77.33278451628661,40.870617162062594],[-77.36418252459318,40.846945156150674],[-77.35711552238749,40.84449215633549],[-77.35663051877414,40.80734214893679]]]},properties:{geoid:”42119″,name:”Union”,state_name:”Pennsylvania”,county_state_name:”Union County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.84,”27_65k_diff”:188.06,”40_65k_diff”:330.38,”60_65k_diff”:1218.95,”27_95k_diff”:0,”40_95k_diff”:117.88,”60_95k_diff”:1006.45,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.42,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:648.48,”40_95k_eptc”:672.92,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:648.48,”40_65k_no_eptc”:790.8,”60_65k_no_eptc”:1679.37,”27_95k_no_eptc”:648.48,”40_95k_no_eptc”:790.8,”60_95k_no_eptc”:1679.37}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-79.61207430600395,41.850336250515845],[-79.68035632719963,41.851532247255136],[-79.71084333602607,41.851462245736734],[-79.7620333526571,41.850918243463006],[-79.79855636398055,41.85111624196949],[-79.84414237868616,41.85085224005417],[-79.91592040115371,41.85068623697364],[-79.93633040671116,41.85039923597705],[-80.01109743001079,41.85020423244263],[-80.05397744442428,41.84986423031273],[-80.08764945429351,41.84985822926348],[-80.14649947216486,41.84904722594303],[-80.21109549339411,41.849048223462546],[-80.25059950495802,41.8494692210112],[-80.40817855455268,41.849472214241665],[-80.51935758882121,41.84957120958579],[-80.51943058111975,41.75270119138803],[-80.51936057638765,41.68894818011982],[-80.51940656942713,41.60710016509489],[-80.5192195603435,41.489119143035026],[-80.44500453637795,41.48712614588713],[-80.44489953701452,41.4922771470014],[-80.43209253328938,41.49209714766114],[-80.43115053229079,41.486966146146095],[-80.37885451642319,41.48583814893351],[-80.35072550687867,41.48472014959502],[-80.27559848362603,41.483490152976565],[-80.25718647735908,41.48342615336025],[-80.22439446784884,41.482499154676724],[-80.16947545063807,41.48153915729134],[-80.1567694462861,41.48089015779467],[-80.12537243619815,41.480404159065074],[-80.1255994370094,41.48628616023926],[-80.0325894088924,41.48890016448023],[-79.99978239854833,41.490057166333074],[-79.99849139908463,41.50095616804175],[-79.98178239307164,41.50016416883355],[-79.98145539467627,41.51290817165714],[-79.96533538986802,41.51286717184921],[-79.95816338775488,41.513632172932034],[-79.95918238854452,41.52536117516503],[-79.94223038364558,41.52535617561601],[-79.94329938418142,41.53784517813303],[-79.92334337772965,41.53760417861239],[-79.92537238032497,41.550216180603215],[-79.90947437529273,41.550157181160614],[-79.9084813756206,41.562184184153914],[-79.89289437049344,41.562165184317905],[-79.89255537174378,41.5741541870266],[-79.8700343641875,41.57426318789759],[-79.873005366058,41.5811601886283],[-79.85005735965255,41.58706419141157],[-79.84961235997919,41.597772192815505],[-79.82972535353073,41.6019611943852],[-79.82911435593417,41.62207819809995],[-79.76834833662508,41.62096320056207],[-79.76836033588366,41.61771920039349],[-79.7480473296535,41.61791820152017],[-79.72762032388248,41.617460202355474],[-79.64335229690005,41.6172082053958],[-79.61317628782423,41.616876207155535],[-79.61315028800772,41.62387120792491],[-79.61255428824889,41.63043820919169],[-79.61298929373199,41.70106722258007],[-79.61256430130283,41.79532424027325],[-79.61207430600395,41.850336250515845]]]},properties:{geoid:”42039″,name:”Crawford”,state_name:”Pennsylvania”,county_state_name:”Crawford County, Pennsylvania”,”27_22k_diff”:66.19,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.84,”40_35k_diff”:131.84,”60_35k_diff”:131.84,”27_65k_diff”:72.39,”40_65k_diff”:189.32,”60_65k_diff”:919.39,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:706.89,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.42,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:532.81,”40_95k_eptc”:649.74,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.19,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.88,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:532.81,”40_65k_no_eptc”:649.74,”60_65k_no_eptc”:1379.81,”27_95k_no_eptc”:532.81,”40_95k_no_eptc”:649.74,”60_95k_no_eptc”:1379.81}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-79.99978237287708,41.17186910683948],[-79.95929336029933,41.17166510885666],[-79.90642734426451,41.172128111166884],[-79.86929633251893,41.172749112698355],[-79.82448431938549,41.1731301149914],[-79.71882228601292,41.172654119861676],[-79.69498727892389,41.17287312109327],[-79.70058428057582,41.17506712133034],[-79.7003362810235,41.18179812190814],[-79.69724528062528,41.18462212320787],[-79.6905662781636,41.181491122681315],[-79.68388027616982,41.18438712299532],[-79.67021627167387,41.1845521244017],[-79.66537127085792,41.18903212544514],[-79.67061727250189,41.19317412560253],[-79.66652227199431,41.19649912595616],[-79.66889527309463,41.199083126576596],[-79.64963126825366,41.217920130805666],[-79.65039727079896,41.25371713819119],[-79.63287826583614,41.25360713840086],[-79.63271326627732,41.26692714121845],[-79.62772926477071,41.26691514112473],[-79.62756426564562,41.27719114353313],[-79.60461325845034,41.27708014388582],[-79.6041642617762,41.32148615244976],[-79.5414772424663,41.321016155000684],[-79.54143324326604,41.33595915761161],[-79.47814322323372,41.33571616107335],[-79.4778252278428,41.386487170539894],[-79.47816623197481,41.440142179939826],[-79.52160224510307,41.44056217791718],[-79.52202724658234,41.465227182805364],[-79.51227924362554,41.46524818329263],[-79.51122324671415,41.50042619015656],[-79.51207325623581,41.62456721291854],[-79.61315028800772,41.62387120792491],[-79.61317628782423,41.616876207155535],[-79.64335229690005,41.6172082053958],[-79.72762032388248,41.617460202355474],[-79.7480473296535,41.61791820152017],[-79.76836033588366,41.61771920039349],[-79.76834833662508,41.62096320056207],[-79.82911435593417,41.62207819809995],[-79.82972535353073,41.6019611943852],[-79.84961235997919,41.597772192815505],[-79.85005735965255,41.58706419141157],[-79.873005366058,41.5811601886283],[-79.8700343641875,41.57426318789759],[-79.89255537174378,41.5741541870266],[-79.89289437049344,41.562165184317905],[-79.9084813756206,41.562184184153914],[-79.90947437529273,41.550157181160614],[-79.92537238032497,41.550216180603215],[-79.92334337772965,41.53760417861239],[-79.94329938418142,41.53784517813303],[-79.94223038364558,41.52535617561601],[-79.95918238854452,41.52536117516503],[-79.95816338775488,41.513632172932034],[-79.96533538986802,41.51286717184921],[-79.98145539467627,41.51290817165714],[-79.98178239307164,41.50016416883355],[-79.99849139908463,41.50095616804175],[-79.99978239854833,41.490057166333074],[-79.999780387018,41.34144813875591],[-79.99978237645965,41.211837114302895],[-79.99920737529692,41.19710011194699],[-79.99978237287708,41.17186910683948]]]},properties:{geoid:”42121″,name:”Venango”,state_name:”Pennsylvania”,county_state_name:”Venango County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.83,”40_35k_diff”:131.83,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:31.55,”60_65k_diff”:584.35,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:371.85,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:403.43,”40_65k_eptc”:460.42,”60_65k_eptc”:460.41,”27_95k_eptc”:403.43,”40_95k_eptc”:491.97,”60_95k_eptc”:672.91,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.87,”27_65k_no_eptc”:403.43,”40_65k_no_eptc”:491.97,”60_65k_no_eptc”:1044.76,”27_95k_no_eptc”:403.43,”40_95k_no_eptc”:491.97,”60_95k_no_eptc”:1044.76}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-78.20364284484296,41.617607267608605],[-78.20400085101691,41.70593528429667],[-78.20495885857896,41.791421300164934],[-78.20666586552248,41.8762303159504],[-78.20617686792569,41.913030323278036],[-78.20638287447056,41.99952633915302],[-78.27290089567116,41.99911933575122],[-78.42878194495302,41.99981832977346],[-78.54175598085534,41.99985332422813],[-78.6228790056533,41.99998332108819],[-78.69881303042393,41.99864231733524],[-78.78033905548936,41.99808431444094],[-78.85736207982718,41.99771331093534],[-78.91889909963128,41.99812730829597],[-78.91848409608129,41.95294829975001],[-78.91550309464508,41.952956299391985],[-78.91706008747119,41.86182928259679],[-78.91600708758475,41.86182028324643],[-78.91564508561476,41.84090427898931],[-78.92154708785985,41.84089027906743],[-78.92141108728215,41.830927276891245],[-78.94861509567578,41.8304892756101],[-78.95164709081547,41.75120726100559],[-78.95192308915281,41.7357042583686],[-78.95402508572138,41.68588424909861],[-78.95469008508913,41.66423324425301],[-78.95467208313187,41.64025224032185],[-78.95614108170575,41.62334223674294],[-78.81497403735332,41.622681242584356],[-78.81524003811533,41.624257243046785],[-78.74462301593944,41.62518024682105],[-78.67601899417578,41.62498124928695],[-78.48381793430207,41.63148925843768],[-78.48291193089456,41.602338252993306],[-78.42050091156848,41.60188225592037],[-78.42084891328138,41.61729225886754],[-78.31494687936173,41.617462263289546],[-78.20364284484296,41.617607267608605]]]},properties:{geoid:”42083″,name:”McKean”,state_name:”Pennsylvania”,county_state_name:”McKean County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.83,”40_35k_diff”:131.83,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:31.55,”60_65k_diff”:584.35,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:371.85,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:403.43,”40_65k_eptc”:460.42,”60_65k_eptc”:460.41,”27_95k_eptc”:403.43,”40_95k_eptc”:491.97,”60_95k_eptc”:672.91,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.87,”27_65k_no_eptc”:403.43,”40_65k_no_eptc”:491.97,”60_65k_no_eptc”:1044.76,”27_95k_no_eptc”:403.43,”40_95k_no_eptc”:491.97,”60_95k_no_eptc”:1044.76}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-76.13548606317389,39.721154983394364],[-76.1364530640474,39.72568998452688],[-76.12826406195263,39.72766498541913],[-76.12225405965525,39.72341498467617],[-76.11852305897672,39.72643998575101],[-76.12030605874176,39.72985598626015],[-76.11992605991716,39.736371987698156],[-76.11361805746253,39.737132988133304],[-76.10856705619726,39.73484398787865],[-76.11117905620132,39.728528986590284],[-76.10796205514053,39.725381986084166],[-76.10248105375963,39.72404098519086],[-76.09262205086745,39.733541987589945],[-76.096190051579,39.737243988037385],[-76.10205205455156,39.73989198880991],[-76.09687905317664,39.74311898983771],[-76.09204205096992,39.7431239895248],[-76.08433604900421,39.74834999096716],[-76.08260104917642,39.75305799221489],[-76.08579605019615,39.75589799262164],[-76.0818540491762,39.76135899378987],[-76.07646304796523,39.761820994017484],[-76.06742904397755,39.75965799355292],[-76.0624700436269,39.76510599509829],[-76.06492504477254,39.77029099597582],[-76.0605260431944,39.775018997371895],[-76.05839904247232,39.77986899864349],[-76.04968004074301,39.783791999209654],[-76.04852704045996,39.789248000187754],[-76.04136703878639,39.79720400248761],[-76.04574003980373,39.80099700316967],[-76.03850303770592,39.80173800351471],[-76.03512503688907,39.80815100439025],[-76.0352180380907,39.81184300586898],[-76.02992703604818,39.8125130055108],[-76.03107403665031,39.817534007190716],[-76.0379550389226,39.82591700809677],[-76.02703603525897,39.82416100784893],[-76.02282803488636,39.830808009288106],[-76.01647503293113,39.8314890104066],[-76.01781103422925,39.83818101152455],[-76.0228250355705,39.849852013946254],[-76.01991203492175,39.853532014145195],[-76.00857703123432,39.851973014582825],[-76.00447403123238,39.87218601850451],[-76.00243403108041,39.874361018964436],[-75.99164602731103,39.86872101850446],[-75.986700026534,39.87438502009404],[-75.99234902845535,39.88216802109731],[-75.99126002826097,39.88759902201258],[-75.98682502769736,39.89220002335736],[-75.99333102985932,39.89900402448507],[-75.99751803160089,39.90989902642681],[-75.99489803196586,39.916593027593564],[-75.99713403209313,39.92207002881219],[-75.99146903106299,39.929011030754424],[-75.98096802856189,39.9334870312919],[-75.98880203077377,39.94084903254068],[-75.99104203203079,39.947584034288525],[-75.99463103391935,39.952437035001225],[-75.98616503210916,39.96389503705363],[-75.98670403215702,39.967248037993805],[-75.96748002714119,39.99444704430827],[-75.93587202029454,40.03747405423364],[-75.93433402014583,40.04757405595825],[-75.93622702203871,40.06529305914588],[-75.9361370228447,40.07859306235227],[-75.94299902722952,40.109274067827414],[-75.9125500178963,40.12064107142718],[-75.89045901154005,40.12953907385453],[-75.87337700684066,40.13711507552625],[-75.8751640078349,40.13807907580123],[-75.95476903616287,40.190150083461425],[-75.98885304791781,40.21164208619209],[-76.00726805486937,40.223831087708426],[-76.04976407040908,40.25080009112711],[-76.06986507667553,40.26390009369221],[-76.14951110526172,40.31446210009639],[-76.15121710576648,40.31597910027737],[-76.26106513808517,40.273354087884805],[-76.30758015171806,40.255074083060556],[-76.36820017012619,40.24742407893062],[-76.4354121908463,40.23822907424108],[-76.47035920076765,40.22708107106495],[-76.50204621007333,40.217443067634875],[-76.56634122940726,40.196652061278385],[-76.57026223010514,40.19456706045131],[-76.5790532337508,40.19486406077949],[-76.58268423467301,40.19096005939916],[-76.59986723948677,40.188272058879946],[-76.60652124210938,40.18999805818924],[-76.6129892432841,40.18538905773438],[-76.61595024419172,40.180615056823626],[-76.62320824627285,40.179320055983425],[-76.62768724701395,40.17674705525871],[-76.63210424854324,40.17062405362638],[-76.63474624962872,40.170548053611654],[-76.64410525200736,40.16491405198994],[-76.65310625494529,40.16605805218553],[-76.65506725572591,40.16396705151812],[-76.66204525737413,40.16347505115567],[-76.67274426060267,40.1576160496791],[-76.67056525897385,40.15449504946997],[-76.68315326319943,40.15180304802415],[-76.69559626726935,40.154105047891804],[-76.69616026767065,40.150125047669796],[-76.69987626760226,40.145118046631055],[-76.70569826998616,40.14302004568767],[-76.71120027113828,40.133280043373304],[-76.71590927245836,40.13148704323797],[-76.72162227347948,40.120078040625785],[-76.71093426963078,40.1138510393754],[-76.69718926481309,40.102500037836],[-76.68753126113413,40.0923110360288],[-76.68043025782265,40.08320003489499],[-76.67550625540453,40.073604032928586],[-76.66382725176288,40.06323503168069],[-76.65372424789807,40.05982103169194],[-76.6436202448794,40.05962703201242],[-76.62060023700697,40.05473703112901],[-76.61336823527071,40.054485031576334],[-76.59759022944908,40.05187503150779],[-76.58848422645728,40.0493210314328],[-76.57121922064641,40.04567703179134],[-76.55389721630074,40.04673303211755],[-76.54145721210712,40.05104503353432],[-76.53452621006944,40.05135603441562],[-76.5315542088517,40.04616503333376],[-76.53217020850198,40.038240031479994],[-76.52787020605581,40.027998030074556],[-76.52032920351424,40.02003002857458],[-76.5136402004953,40.01563102782035],[-76.50958819953439,40.00943102647174],[-76.5006131956169,40.00063202571396],[-76.49845619491794,39.99673802470769],[-76.49535419295003,39.97613602036241],[-76.48739118924969,39.9621430187101],[-76.47920918661231,39.95482101700314],[-76.47358218435305,39.94736001573092],[-76.467579182251,39.94305701560825],[-76.45975217970766,39.94125801522412],[-76.44897117506329,39.934346014301816],[-76.4304031697123,39.928915013977544],[-76.42215816624795,39.925840013222896],[-76.40567216058636,39.91596301231397],[-76.39167615557949,39.91282701215326],[-76.38578815423175,39.90617501094299],[-76.38377915194297,39.893625008577715],[-76.37964415088032,39.88820900740188],[-76.38171115121126,39.87906800577658],[-76.380694150212,39.8736830045193],[-76.37665914805086,39.865650003665344],[-76.3696431454091,39.86040700310215],[-76.36167614266724,39.857062001978036],[-76.35076113903693,39.84709800097023],[-76.35054513843878,39.83776399924371],[-76.34240313484713,39.82887399750607],[-76.33825713391616,39.82206999586576],[-76.3283551297366,39.81479599479346],[-76.31570412628575,39.81004499497688],[-76.31107612410295,39.8036379936924],[-76.29018411661636,39.785018990746856],[-76.27611511066279,39.77562798944096],[-76.27160010949866,39.76581398760618],[-76.26747710765376,39.759365986366454],[-76.26057910471546,39.75204298571329],[-76.25656610365262,39.75004798535495],[-76.24958610103906,39.73998798321407],[-76.24557509917183,39.737181983077676],[-76.24058409676744,39.73032098130485],[-76.2386920964639,39.72510098076914],[-76.23980709677257,39.72134298019924],[-76.18471407924798,39.72131498223827],[-76.14374406586967,39.72152998375833],[-76.13548606317389,39.721154983394364]]]},properties:{geoid:”42071″,name:”Lancaster”,state_name:”Pennsylvania”,county_state_name:”Lancaster County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.83,”40_35k_diff”:131.83,”60_35k_diff”:131.84,”27_65k_diff”:26.17,”40_65k_diff”:132.95,”60_65k_diff”:799.68,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:587.18,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.41,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:486.58,”40_95k_eptc”:593.37,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.87,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:486.58,”40_65k_no_eptc”:593.37,”60_65k_no_eptc”:1260.1,”27_95k_no_eptc”:486.58,”40_95k_no_eptc”:593.37,”60_95k_no_eptc”:1260.1}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-79.69293324021642,40.66975202619481],[-79.6801492357894,40.67195202681436],[-79.66834823360159,40.680057029004544],[-79.66246023094102,40.678329028866024],[-79.65295622758026,40.6719130280782],[-79.64404422448898,40.66885702787438],[-79.63814022319876,40.66560902783412],[-79.63605922173873,40.654489025803024],[-79.62861921825312,40.64868102494593],[-79.62221921620035,40.64570502419825],[-79.61313121340564,40.64362502406847],[-79.60949921232843,40.63981702359383],[-79.6101382111312,40.63101702209531],[-79.60895521113285,40.62596202137372],[-79.60210620912056,40.62450502155796],[-79.59636220704964,40.62832902183248],[-79.59148220648179,40.634345023416884],[-79.5869382053911,40.6367450243885],[-79.58282620343813,40.63317702353554],[-79.58866520486478,40.62552902150864],[-79.58956220465012,40.61660101975849],[-79.58378520157329,40.61042201912864],[-79.58437820239823,40.6070490189646],[-79.58119420066883,40.602537018214036],[-79.57468119819717,40.60263301837624],[-79.5703351969515,40.60672901887239],[-79.56600919566615,40.60796101961509],[-79.55850519359635,40.605001019746155],[-79.5518321914854,40.60471302002944],[-79.55621719238857,40.59981701811655],[-79.5663931953247,40.59296901701923],[-79.57066519528345,40.58375301520704],[-79.56111319176148,40.5641210114846],[-79.55728919015334,40.56096901095485],[-79.53621618321677,40.550341009774016],[-79.52625217955556,40.54237200836318],[-79.52099517696995,40.54131300843441],[-79.5119151748221,40.54269100929702],[-79.50538317254909,40.53594500877076],[-79.49892817016217,40.532160008160176],[-79.49795316885223,40.52654100736269],[-79.49461316773397,40.52488800658688],[-79.48570916525193,40.52838400744843],[-79.48473216586177,40.53420600940305],[-79.47934016417999,40.53704600969589],[-79.47574216284251,40.52954600879964],[-79.4642921593262,40.534088009830796],[-79.45503615634269,40.53411501048743],[-79.45017915470932,40.530157009435285],[-79.37783313688847,40.603967027044746],[-79.27693811436659,40.71106205185264],[-79.21521809915843,40.775950066716405],[-79.21490410065005,40.78851406890591],[-79.21520710502074,40.848648079983356],[-79.21531310952638,40.911354092495806],[-79.21570911137539,40.94005809799634],[-79.21254811215468,40.96053510192483],[-79.21264111262849,40.966491102275135],[-79.21020011784044,41.04909911852806],[-79.21521711998865,41.05052311844085],[-79.21906812079983,41.048593117587814],[-79.23006512467299,41.0460281173461],[-79.2364821261477,41.04203911616071],[-79.24204912732014,41.03535111484478],[-79.26065913244923,41.0293531126086],[-79.26757313334844,41.020233110905906],[-79.2739881358208,41.017623109612956],[-79.28152213781216,41.010372108050646],[-79.28500113851052,41.00930310751323],[-79.29949614292613,41.01176910730565],[-79.3024791442184,41.013543107557744],[-79.32027314866214,41.00154510495744],[-79.3360381535404,41.00011510383581],[-79.34159915511832,41.00138810391991],[-79.34503815579195,40.998078102938635],[-79.35634416026572,40.99980410297233],[-79.36102916172722,41.0037711035241],[-79.3659741629707,41.00080810300363],[-79.37101816391466,40.990173100800746],[-79.37156916336916,40.98256909866172],[-79.3695631620287,40.974928097793274],[-79.37425216338497,40.96889709614984],[-79.37908916465507,40.96841409576728],[-79.38219416552539,40.97119309598035],[-79.38097716601612,40.979889097691185],[-79.37476516513422,40.98374809943403],[-79.38305916744434,40.98498509903689],[-79.38554016862464,40.98977409931418],[-79.37798216618698,40.99077509986516],[-79.37966616747927,40.99510810064422],[-79.38946417029155,40.9935590998543],[-79.3947171718319,40.99475809982042],[-79.39746617263533,40.990070099380375],[-79.40178717298136,40.987858098841464],[-79.40602617497339,40.99103309876859],[-79.4042861747442,40.995672099635065],[-79.40659517613814,40.99858010001359],[-79.41349617733113,40.998245100020604],[-79.41503817897409,41.00071410089916],[-79.41006917708067,41.005306101391234],[-79.41288917793578,41.008325101835524],[-79.42027818008607,41.00398610102527],[-79.42086718003573,40.99904209980209],[-79.42465218079194,40.98897309825988],[-79.43065218229502,40.98536109672166],[-79.43962118489732,40.98741509671953],[-79.44475118660188,40.98644909679827],[-79.45102518805469,40.981738095187545],[-79.46187819193776,40.98268009519146],[-79.46188619207314,40.98529409536581],[-79.45589519047276,40.98818309664366],[-79.45696119118794,40.99115309663957],[-79.46466319253553,40.99031109610318],[-79.46954819540615,40.99346209704042],[-79.4756061969547,40.99491009660862],[-79.48172919816457,40.994078096149195],[-79.48852020043168,40.995377096174295],[-79.49478820211739,40.986189094603866],[-79.49366120083555,40.97790909256466],[-79.50334220433075,40.97643209168891],[-79.50667620578304,40.98308009337365],[-79.5140152081382,40.98681709349887],[-79.51776520934536,40.98305309234463],[-79.51468820806123,40.979033092524666],[-79.52168021014668,40.975076091150044],[-79.52861721244588,40.97842109131371],[-79.53582521420397,40.98007109133436],[-79.53943021620613,40.984296091771284],[-79.54533421811979,40.98225609144403],[-79.553801219824,40.98170009118383],[-79.56222622353528,40.98544509155814],[-79.57279022619385,40.98530809036567],[-79.58156322912761,40.98003008918595],[-79.58898623076358,40.97086508750056],[-79.59342523157267,40.968827086335864],[-79.60122023412134,40.969292086326405],[-79.61835523918171,40.97415008693723],[-79.62429324251123,40.97875308757594],[-79.62349424193606,40.98456808882739],[-79.61907024087189,40.98896808932655],[-79.61043023859604,40.993232090976825],[-79.60337123649042,40.99480609143884],[-79.59701623431856,40.99439609113168],[-79.58610223065145,40.991302090956566],[-79.58185622930476,40.993597091974806],[-79.5822562306974,40.99864909272217],[-79.58795423300386,41.003251093776306],[-79.59539623450476,41.00510009348832],[-79.60763023878515,41.00542409349687],[-79.60918923941779,41.012252094728325],[-79.60261023806227,41.020827096264874],[-79.59893523809971,41.0322190981841],[-79.60200823925138,41.037169099246256],[-79.61091024236457,41.03397309870447],[-79.61957824466378,41.03340409789704],[-79.63293924948832,41.037255097512464],[-79.65126025564686,41.04506509833156],[-79.66247625894655,41.047344098125016],[-79.66576526031952,41.04913109898814],[-79.66720326072088,41.05546009989999],[-79.66542626018179,41.05854610018663],[-79.65896725916848,41.06256510171677],[-79.65550625847295,41.06674210217122],[-79.65905425942941,41.07348610365012],[-79.66603626285844,41.07886310438338],[-79.67403626544716,41.08251810449971],[-79.67695226697064,41.08573810532415],[-79.68006026761216,41.09371810625139],[-79.68134326992855,41.10659710914628],[-79.6792772693661,41.11586911038757],[-79.67982126998805,41.125539112736405],[-79.67866826991664,41.13067611359766],[-79.6797102717183,41.137225114254754],[-79.68618727390948,41.14380111558659],[-79.68625327444197,41.14855711678488],[-79.6802472726846,41.15574911839148],[-79.68150127428069,41.16293111943461],[-79.68933527613534,41.16947912034348],[-79.68878127372258,41.13343711378472],[-79.69027527205961,41.103260108005195],[-79.69019526697713,41.0467160971695],[-79.6899282611156,40.957049080476786],[-79.69169925494529,40.875080065014814],[-79.69212725110617,40.813424053192826],[-79.69280624881225,40.793413049135474],[-79.69328724532504,40.741435039290174],[-79.69235524321277,40.710868034004804],[-79.69293324021642,40.66975202619481]]]},properties:{geoid:”42005″,name:”Armstrong”,state_name:”Pennsylvania”,county_state_name:”Armstrong County, Pennsylvania”,”27_22k_diff”:66.19,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.84,”40_35k_diff”:131.84,”60_35k_diff”:131.84,”27_65k_diff”:72.39,”40_65k_diff”:189.32,”60_65k_diff”:919.39,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:706.89,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:460.42,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:532.81,”40_95k_eptc”:649.74,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.19,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.88,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:532.81,”40_65k_no_eptc”:649.74,”60_65k_no_eptc”:1379.81,”27_95k_no_eptc”:532.81,”40_95k_no_eptc”:649.74,”60_95k_no_eptc”:1379.81}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-74.86129563853414,39.32382295004194],[-74.86023563726665,39.31915494949369],[-74.85099863379894,39.31622894852969],[-74.83755663024945,39.31488594867019],[-74.8248846251353,39.305283947487595],[-74.82268962532565,39.30675694827535],[-74.80942862055109,39.306083948388654],[-74.80064561797857,39.308457948642825],[-74.79831361693317,39.30667494918253],[-74.7843756127949,39.307325949506186],[-74.77364260866644,39.300986948298544],[-74.76221960550028,39.29680494824301],[-74.75436960300391,39.299161948513884],[-74.75216660215493,39.2950129485008],[-74.74093059830166,39.295555948367905],[-74.73804359779102,39.298063949621636],[-74.73159059544214,39.29864794918983],[-74.7284395950643,39.29645894948974],[-74.72167259284647,39.298271949666635],[-74.71969659124439,39.29421494883278],[-74.71439958968344,39.29173594905902],[-74.7111275891868,39.29530494922272],[-74.70151058532878,39.293877949546356],[-74.700182584719,39.29031194853374],[-74.69039058214564,39.29103094959676],[-74.68656358060498,39.29416295058749],[-74.68018257884391,39.29434395083357],[-74.67560857832605,39.2968319509672],[-74.6593035723217,39.297525951792835],[-74.65817057158824,39.289663950491914],[-74.64917956889394,39.289917950614225],[-74.64340956729355,39.29549995220625],[-74.63278056434393,39.295132952256225],[-74.62460056107105,39.292441951745936],[-74.61800555921631,39.29352995260297],[-74.59176755192969,39.30935095622525],[-74.58369154902432,39.308866956737184],[-74.56876354405676,39.29927595497231],[-74.55861954156042,39.29857495513383],[-74.54751553817549,39.30206595679396],[-74.5429635366055,39.30165495625512],[-74.53908453483008,39.298233955826674],[-74.46493151095558,39.29823795840488],[-74.46161651059046,39.30103095889322],[-74.43060250152536,39.30836396149204],[-74.41140049556715,39.30967396252706],[-74.39219748947966,39.31229396404939],[-74.37459248351252,39.31753396578064],[-74.36251447998467,39.32578896811421],[-74.35466047867409,39.335414969715856],[-74.35004847813391,39.345775972231365],[-74.3442404762678,39.34869497327553],[-74.32541647081337,39.36234697665163],[-74.31113646658609,39.37512497930533],[-74.28727246052317,39.398259985318475],[-74.26591945559454,39.422422990546785],[-74.24958645150326,39.452607996836896],[-74.23206344751436,39.475206002273495],[-74.2964624682573,39.47530000017337],[-74.312613475217,39.50012500511119],[-74.32195847755627,39.50515200494814],[-74.3263834796068,39.506340005073824],[-74.33858948313289,39.506863005287045],[-74.35501748799545,39.50537200410165],[-74.36096948995907,39.50203500303751],[-74.3807974956754,39.49854500228882],[-74.40168450551948,39.537930009423874],[-74.4104905081706,39.54786001132493],[-74.41584251034392,39.549458011287655],[-74.41739451131605,39.55726301275352],[-74.42539351398851,39.55352901149502],[-74.43536951659028,39.555439011287774],[-74.43835151700493,39.55132101045312],[-74.43344851595359,39.543847009101206],[-74.43612051646107,39.54127300884802],[-74.4419995186153,39.54278700854027],[-74.44613651966753,39.54975100988194],[-74.44356751982089,39.55476601082311],[-74.44672352003866,39.55906901211542],[-74.45261652226243,39.55692301088835],[-74.45344752211908,39.548581009545195],[-74.4595775242554,39.54858300972671],[-74.46216552512102,39.556102010804004],[-74.46776052656861,39.55567501087521],[-74.47183452776672,39.552002010002255],[-74.47566552963997,39.551468009492275],[-74.48049853086022,39.557047010642094],[-74.48635153348103,39.55821901079005],[-74.49398353492087,39.556221010007214],[-74.49486953539709,39.561348010589015],[-74.50591853949184,39.569653012163585],[-74.51223254178326,39.56996001197022],[-74.51702454331179,39.57415901273749],[-74.52354154585484,39.5695600117045],[-74.52763854669733,39.56963801093824],[-74.53239054850499,39.57337801188067],[-74.53851155084288,39.57452601203947],[-74.54264255190476,39.57912801269332],[-74.54198255234814,39.58582401416647],[-74.54904855459387,39.590320014343625],[-74.55324155673138,39.597748015998434],[-74.56333255927792,39.59672301531636],[-74.57171256229556,39.59894701517768],[-74.57575056388889,39.598403015138445],[-74.5801745653759,39.60286401577331],[-74.58512756695741,39.60496001598508],[-74.5887195681601,39.611810017905015],[-74.59726657190386,39.614692017467],[-74.61099657653655,39.6227790188195],[-74.6163285776076,39.62345201927493],[-74.62102957965547,39.62669901923382],[-74.62474758137918,39.625765018758],[-74.627613581096,39.62039501795633],[-74.63139758240465,39.625014018816486],[-74.63558858490353,39.62712401918918],[-74.64796558831347,39.625082017883926],[-74.65299958999766,39.62659501861209],[-74.6544655906084,39.62992601860689],[-74.65929659216648,39.63124101888618],[-74.65987759231568,39.63941702066975],[-74.65709659194387,39.64485002184694],[-74.66048059420172,39.66880702609458],[-74.66494059688242,39.67479202757367],[-74.66432859620309,39.676771028195674],[-74.669510598408,39.685035029513],[-74.67381560026969,39.68722002975509],[-74.67614260078523,39.69162503077289],[-74.73621762230161,39.72978303644815],[-74.82063964502977,39.65716401813183],[-74.87726165959303,39.608360006558314],[-74.98527268889309,39.51497498419964],[-74.89678965683005,39.45267197495812],[-74.87227964757855,39.43615697192355],[-74.85597964203453,39.42424597048552],[-74.85740964267801,39.42327697012026],[-74.85311164094395,39.41554296897151],[-74.85304964001824,39.40925796753697],[-74.85729164189891,39.403019966529484],[-74.85821664084366,39.395555964473274],[-74.85199063871077,39.38375296259509],[-74.8534126383723,39.3723319603169],[-74.85865863946319,39.36439795866852],[-74.85924263949073,39.35904195746576],[-74.86491263998454,39.338886953247076],[-74.86415463929455,39.3283869505865],[-74.86129563853414,39.32382295004194]]]},properties:{geoid:”34001″,name:”Atlantic”,state_name:”New Jersey”,county_state_name:”Atlantic County, New Jersey”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:84.32,”60_65k_diff”:696.41,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:483.91,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.05,”27_65k_eptc”:446.7,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:446.7,”40_95k_eptc”:544.74,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:446.7,”40_65k_no_eptc”:544.74,”60_65k_no_eptc”:1156.83,”27_95k_no_eptc”:446.7,”40_95k_no_eptc”:544.74,”60_95k_no_eptc”:1156.83}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-79.29388707101101,40.04045392222007],[-79.288581069585,40.041782922604355],[-79.28431306797569,40.04825392397342],[-79.2781040672722,40.05048692473651],[-79.27876906752779,40.05554492541835],[-79.27135406505023,40.06424592773145],[-79.26716906500154,40.066017928155894],[-79.26774206516698,40.07427593020002],[-79.26439006479806,40.07867593057402],[-79.25867406309901,40.0802809317182],[-79.2561400624533,40.08834793325154],[-79.24640106016732,40.09371793466473],[-79.24301605859759,40.09227793441467],[-79.23662305742862,40.096548935595145],[-79.22667505392408,40.098257936140335],[-79.22262305287452,40.10417893790447],[-79.22086705320284,40.11274493937008],[-79.21077705042329,40.11891094101867],[-79.20519204883396,40.11656794071424],[-79.19687504667618,40.11595894046721],[-79.19216404407159,40.11027493987761],[-79.18522504179565,40.10985594033871],[-79.18099004077877,40.11572194174085],[-79.1742520396898,40.12061194244523],[-79.1719590393804,40.12635894375651],[-79.16762903767298,40.12879094408593],[-79.16582803846866,40.13869894650727],[-79.16212603728376,40.143317947230464],[-79.16275703831431,40.15406994976132],[-79.16092803779308,40.16114895089949],[-79.1497710344117,40.16038095101161],[-79.14070503260247,40.16331495218372],[-79.14106803336891,40.17306595413473],[-79.1433090337709,40.17989695508848],[-79.13439603153715,40.178729955075156],[-79.12965602980768,40.180931956170326],[-79.12381702937293,40.1939569584478],[-79.12570303009086,40.20070896031573],[-79.12194502850203,40.20314596055313],[-79.1162420273491,40.20376096142705],[-79.11428902724458,40.210265962367124],[-79.10793202507979,40.21303396345451],[-79.10300602384419,40.21823896468036],[-79.09867302399974,40.2261049664828],[-79.1001560246745,40.23115696723739],[-79.09594902262415,40.232617967116326],[-79.09491002323986,40.23649296868985],[-79.08617702029608,40.242672969922545],[-79.08247502068677,40.25008197155718],[-79.07925301892732,40.25117997154783],[-79.07957302021015,40.25793597302348],[-79.07664101879442,40.26031497399261],[-79.07352601854836,40.2667349754211],[-79.0679660168893,40.272478975942114],[-79.05938101497169,40.27577497725574],[-79.05664901402571,40.27861197839796],[-79.05605601496902,40.284868979579656],[-79.0460760120278,40.29657998213159],[-79.04505001242205,40.29965498217918],[-79.03756101023815,40.3069689844828],[-79.03729801044948,40.31341098545467],[-79.03166800860517,40.31765398672091],[-79.02971500942891,40.322976987801404],[-79.0254140081813,40.32601298831566],[-79.02002200668471,40.3356129905794],[-79.01537100565217,40.33919499134425],[-79.0102820036892,40.340235991984414],[-79.00608100395384,40.351210994178416],[-78.99817400177862,40.35617699537366],[-78.97523299724493,40.391935003406935],[-78.97381699652537,40.3954290037767],[-78.98232700063075,40.40578700592496],[-78.98887300291068,40.41198200613921],[-78.99664000482167,40.41326400612057],[-79.0166200119986,40.42028700657895],[-79.02784001488001,40.41958200614987],[-79.03301001659936,40.41678200589837],[-79.03426501631442,40.40976200445701],[-79.0277170145283,40.406144003641266],[-79.0363310166461,40.396004001124794],[-79.03983801687225,40.396281001283896],[-79.04243901767931,40.39138999986736],[-79.05188802111722,40.38929399989577],[-79.05711202178956,40.384300998055295],[-79.05848402259024,40.38087599782589],[-79.06455602397669,40.379009996678235],[-79.06988802545642,40.38042199694783],[-79.07448602758457,40.38582799806249],[-79.08296803022239,40.38958999844364],[-79.08831503133396,40.38656099773153],[-79.09053003163008,40.38025099659631],[-79.096119033003,40.374042994758845],[-79.09677203331074,40.37073299439597],[-79.10215603456905,40.36887599350939],[-79.10931203775642,40.37332599361365],[-79.12163704112788,40.370583993044505],[-79.12711904284573,40.375075993543106],[-79.12868004434682,40.38506399547422],[-79.12250604226719,40.38936199679839],[-79.11490904031105,40.389886996737076],[-79.11700304145873,40.3942509973683],[-79.12475204418307,40.39536899726114],[-79.13500804704871,40.398311998169],[-79.14789505058616,40.39760799677088],[-79.15400505320129,40.40170899735387],[-79.15205405300733,40.4087739991369],[-79.15579205458442,40.4117729997382],[-79.1643720572946,40.41023199857873],[-79.17371605975194,40.4106299989492],[-79.19120006594908,40.41522899841474],[-79.19923606787684,40.410787997755754],[-79.20651607012762,40.4150399978309],[-79.21478607385926,40.424465999539564],[-79.23320608010897,40.43074899952313],[-79.24017808164469,40.42999899905817],[-79.24757108488734,40.43208799950256],[-79.25411708575506,40.42229599694649],[-79.26328408825277,40.4167709955048],[-79.27285909148482,40.41841899617886],[-79.27354509151246,40.422932996728996],[-79.26935409098053,40.42852499784273],[-79.27260809314643,40.43909000016678],[-79.28285109613083,40.442777000411056],[-79.28941209737626,40.43668099869458],[-79.29943810112218,40.43452299807307],[-79.30175410164283,40.439298998662004],[-79.29990010199404,40.4449199993294],[-79.30168010244839,40.45136400088206],[-79.29763410177054,40.45580400221964],[-79.30035410316223,40.46097800322258],[-79.31610310803087,40.45926100213129],[-79.32278910939257,40.45604000126323],[-79.3254121103845,40.45270700007633],[-79.33027011142069,40.45385899983845],[-79.33173511227638,40.46189700198271],[-79.33844311507272,40.470006003029496],[-79.34541111722568,40.467220001782536],[-79.34592911713678,40.45483300001816],[-79.35385411854209,40.45170899896211],[-79.36052912117806,40.454102999204274],[-79.36227812163996,40.460068999616894],[-79.35803212171645,40.47088700197612],[-79.35859812278684,40.47792400322685],[-79.36592812408546,40.47748200346486],[-79.36707312440504,40.47509800240801],[-79.3663371233842,40.46597400135002],[-79.36959412465934,40.45661199936056],[-79.37419412533366,40.45370099823097],[-79.38175612728591,40.45270499811449],[-79.39110513052825,40.45441999767945],[-79.39546413260949,40.457139997791835],[-79.40663413680969,40.47430900070217],[-79.41569313990573,40.47057999996232],[-79.42131814070379,40.470605999423476],[-79.42357714170551,40.47333699959164],[-79.4306311453194,40.489054002472166],[-79.43846314809879,40.48674500213506],[-79.44754015042088,40.48081900042509],[-79.45401415300309,40.485515001027935],[-79.4524651522273,40.4894380016158],[-79.45530015353216,40.496624002967614],[-79.45455115372746,40.507022005209365],[-79.45974115606226,40.5167450066152],[-79.45654815642561,40.52324500773714],[-79.44964315429495,40.52680000884371],[-79.45017915470932,40.530157009435285],[-79.45503615634269,40.53411501048743],[-79.4642921593262,40.534088009830796],[-79.47574216284251,40.52954600879964],[-79.47934016417999,40.53704600969589],[-79.48473216586177,40.53420600940305],[-79.48570916525193,40.52838400744843],[-79.49461316773397,40.52488800658688],[-79.49795316885223,40.52654100736269],[-79.49892817016217,40.532160008160176],[-79.50538317254909,40.53594500877076],[-79.5119151748221,40.54269100929702],[-79.52099517696995,40.54131300843441],[-79.52625217955556,40.54237200836318],[-79.53621618321677,40.550341009774016],[-79.55728919015334,40.56096901095485],[-79.56111319176148,40.5641210114846],[-79.57066519528345,40.58375301520704],[-79.5663931953247,40.59296901701923],[-79.55621719238857,40.59981701811655],[-79.5518321914854,40.60471302002944],[-79.55850519359635,40.605001019746155],[-79.56600919566615,40.60796101961509],[-79.5703351969515,40.60672901887239],[-79.57468119819717,40.60263301837624],[-79.58119420066883,40.602537018214036],[-79.58437820239823,40.6070490189646],[-79.58378520157329,40.61042201912864],[-79.58956220465012,40.61660101975849],[-79.58866520486478,40.62552902150864],[-79.58282620343813,40.63317702353554],[-79.5869382053911,40.6367450243885],[-79.59148220648179,40.634345023416884],[-79.59636220704964,40.62832902183248],[-79.60210620912056,40.62450502155796],[-79.60895521113285,40.62596202137372],[-79.6101382111312,40.63101702209531],[-79.60949921232843,40.63981702359383],[-79.61313121340564,40.64362502406847],[-79.62221921620035,40.64570502419825],[-79.62861921825312,40.64868102494593],[-79.63605922173873,40.654489025803024],[-79.63814022319876,40.66560902783412],[-79.64404422448898,40.66885702787438],[-79.65295622758026,40.6719130280782],[-79.66246023094102,40.678329028866024],[-79.66834823360159,40.680057029004544],[-79.6801492357894,40.67195202681436],[-79.69293324021642,40.66975202619481],[-79.692881240698,40.66961902576937],[-79.6958252400251,40.66151302464331],[-79.69108523799461,40.65247602300176],[-79.68897823669626,40.645443021681565],[-79.6902812373859,40.64088102095543],[-79.69435623835574,40.635135019632514],[-79.70333724000145,40.62570301675044],[-79.7145792423898,40.61701801457435],[-79.72315724528877,40.60699701269695],[-79.73609024795189,40.60205101135669],[-79.74944025239697,40.598875009713026],[-79.76319325664475,40.59362700875062],[-79.77162625806075,40.58563700629151],[-79.77336425843812,40.58209500542547],[-79.77480525855738,40.572812004115875],[-79.77413425842585,40.568384003496305],[-79.76854625535096,40.55500400084637],[-79.765093253352,40.54924599972765],[-79.75170424924659,40.55183100076122],[-79.74265924624002,40.548531000369884],[-79.73665224502017,40.54932300096101],[-79.7286692415577,40.543443000091564],[-79.72113123929283,40.54117000069302],[-79.71437623726348,40.5328859987714],[-79.70790523501073,40.53067099852254],[-79.70162723193216,40.525456998311306],[-79.70209023212499,40.52177099734985],[-79.70213422999043,40.489642991080814],[-79.70339622792353,40.4514689842896],[-79.70478622642196,40.42633197943682],[-79.7069422263906,40.42232697795845],[-79.71603122917764,40.417420977088334],[-79.71749222850107,40.41367897621751],[-79.72234122996463,40.41492697585038],[-79.7276582317547,40.41299497552143],[-79.73228123303655,40.40523597408244],[-79.73252623263978,40.39960697251345],[-79.7446372357662,40.3961709713658],[-79.74802723629927,40.39076497080811],[-79.75377923813078,40.38854596991498],[-79.75861223960338,40.39207197044621],[-79.76464124141678,40.39032497002806],[-79.76561324162502,40.38447896841875],[-79.77108524318645,40.37542696655423],[-79.77951524186417,40.33510995858735],[-79.7842112419683,40.31390195452578],[-79.78865124265535,40.29774595092278],[-79.78456924146153,40.29607395093893],[-79.77596623786849,40.289217949399834],[-79.77643323783158,40.284444949130005],[-79.78012023890386,40.282116947963544],[-79.79471824334419,40.28169094720497],[-79.79651924331658,40.279452947248224],[-79.79450524263751,40.27134394512024],[-79.78750523932496,40.2632499443953],[-79.78924324020402,40.25959994315965],[-79.796656241563,40.252840941508296],[-79.79911224199638,40.2469739410457],[-79.8074342437055,40.236901938476066],[-79.80296724194766,40.23149693752425],[-79.78259123591663,40.22763393758485],[-79.81442324426071,40.21668793444435],[-79.83925325223427,40.208762932038056],[-79.87142826030298,40.197398928220785],[-79.86582025869889,40.197038928694425],[-79.85445925544325,40.191262927655096],[-79.85037925306689,40.17731092478626],[-79.85135525224142,40.17215892371249],[-79.85601125383988,40.165806922382465],[-79.86415625562607,40.16182292135509],[-79.87042825765676,40.162094921456074],[-79.88734026302495,40.16499092078114],[-79.89330926498752,40.16499092068096],[-79.90199726737153,40.16137492026402],[-79.90489326828848,40.15423891802206],[-79.90207726701055,40.14865491718047],[-79.89324426296885,40.14078391648518],[-79.88878026171437,40.1326559149698],[-79.88550026063956,40.129503914072],[-79.87786725799504,40.12696691393126],[-79.87529925723166,40.129537915032245],[-79.8690132545554,40.12801791499756],[-79.85360625036208,40.12753891505686],[-79.83941224578012,40.128258916267576],[-79.81611623903643,40.12838291687774],[-79.8165972395909,40.132798918319445],[-79.81004323752282,40.132487918187564],[-79.8038202345187,40.128768917955085],[-79.78220322800543,40.128427918784176],[-79.74605921687834,40.12846492053191],[-79.74117721565287,40.12627891982038],[-79.73485421301876,40.121053919308366],[-79.72760321095039,40.120615919460484],[-79.72336221018922,40.1223459199981],[-79.71850220735102,40.1169289189523],[-79.72180820847878,40.11529491828639],[-79.71127020489126,40.108665917712315],[-79.70540220253187,40.107645917587],[-79.69165819929488,40.113097919318214],[-79.68463719747047,40.11312191988476],[-79.68379719592409,40.10862791862553],[-79.67175419305273,40.106254918825634],[-79.66619019042454,40.10266391881818],[-79.66860519143302,40.09885491781738],[-79.6638691893271,40.096739917182724],[-79.65725718720635,40.09660291799354],[-79.6542881867326,40.0936409170649],[-79.65408618628521,40.08930191607557],[-79.64812518383626,40.087650916485806],[-79.63899718073574,40.08286691576629],[-79.63570018051425,40.08591291675647],[-79.62700117767884,40.08843191727463],[-79.62585617773748,40.09194091823547],[-79.61309917317016,40.0934459188834],[-79.60367717031981,40.09084691878872],[-79.60044516937286,40.08431591766788],[-79.5930241663159,40.08206291777488],[-79.59202916644973,40.09346791985665],[-79.5845791646043,40.0978419215618],[-79.58538016509608,40.10213292210016],[-79.57892316345689,40.10523392253738],[-79.56097115782171,40.106615923580925],[-79.5591201575252,40.111164924365326],[-79.55315315681067,40.11258592549834],[-79.548522155129,40.110329924624835],[-79.54128715221165,40.11275292546392],[-79.54107415269266,40.12082192694943],[-79.53399415206619,40.12862492912989],[-79.53086815084008,40.128215928910436],[-79.52698014901914,40.123244928143286],[-79.51786714622048,40.13138593036589],[-79.50519114343935,40.14057593263982],[-79.49667614078182,40.14176793311351],[-79.48852313818433,40.14122793394874],[-79.48313913679824,40.14405093444976],[-79.46152513054584,40.1441059351543],[-79.46122813013828,40.14135693479744],[-79.44748112523219,40.133240933484515],[-79.4477231251544,40.12677793251597],[-79.44213312249694,40.11957793145865],[-79.43756312082326,40.11586793072718],[-79.42347711624369,40.11116393006859],[-79.41539311302476,40.10460792928371],[-79.40131310823445,40.102237929613125],[-79.39371510512557,40.090904928109985],[-79.37252309827056,40.08137792676673],[-79.36746609676854,40.080205926862284],[-79.35563009240325,40.07436692656493],[-79.35124409066741,40.06787692516915],[-79.34445308717974,40.05089792171611],[-79.34268308660361,40.044177921255034],[-79.33864308487766,40.04215792051712],[-79.32368308055966,40.04078792135635],[-79.31609307857516,40.043847921564875],[-79.30979407650007,40.04355792252656],[-79.29388707101101,40.04045392222007]]]},properties:{geoid:”42129″,name:”Westmoreland”,state_name:”Pennsylvania”,county_state_name:”Westmoreland County, Pennsylvania”,”27_22k_diff”:66.19,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:48.08,”60_65k_diff”:619.45,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:406.95,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.05,”40_35k_eptc”:86.04,”60_35k_eptc”:86.05,”27_65k_eptc”:416.99,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:416.99,”40_95k_eptc”:508.5,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.19,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.88,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:416.99,”40_65k_no_eptc”:508.5,”60_65k_no_eptc”:1079.87,”27_95k_no_eptc”:416.99,”40_95k_no_eptc”:508.5,”60_95k_no_eptc”:1079.87}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-74.73621762230161,39.72978303644815],[-74.75578162868815,39.74221503789601],[-74.76638663270714,39.74657003858943],[-74.77209163512897,39.75044403880141],[-74.776938636333,39.757798039815455],[-74.78120563777297,39.75859504031816],[-74.78529563973495,39.76576504148045],[-74.79072564146587,39.771311042729906],[-74.8061016477775,39.78302104410134],[-74.81711265068311,39.785794044317136],[-74.81942065235768,39.78800904496196],[-74.8432096594984,39.789927044410554],[-74.85322966290616,39.78731804307828],[-74.86948366723479,39.78434204245255],[-74.8761096690931,39.78148104141946],[-74.88981567457091,39.78199004134288],[-74.89482367609203,39.78332004072358],[-74.89863467733723,39.78970104223056],[-74.90296467871418,39.79111604226434],[-74.90554368027108,39.80106304429857],[-74.93074669345403,39.88591606072224],[-74.94936070015756,39.89817206178203],[-74.95194870129062,39.90168006284819],[-74.95253170095725,39.907126063722025],[-74.95590570325355,39.91322506465835],[-74.96420670564146,39.920684065777124],[-74.97428470903579,39.921429065509734],[-74.9838747130442,39.92680406669065],[-74.98142371248946,39.93111906744786],[-74.97508571058775,39.93781906918423],[-74.97558171064306,39.939621069129224],[-74.99181171597596,39.94092306926654],[-74.99442971621596,39.9393730688828],[-75.00415071963911,39.94147306863483],[-75.00906672183157,39.94512806952767],[-75.01508272307868,39.94682106951897],[-75.01616072423859,39.95046106995658],[-75.01309372345303,39.95663607173432],[-75.01760172473737,39.959383071684854],[-75.019867726964,39.969369074112805],[-75.01619872551248,39.97014807362419],[-75.01350472456076,39.9776810757354],[-75.01468772535576,39.985072076878474],[-75.01838872755296,39.9889620776347],[-75.02839573025787,39.991952078334265],[-75.03635573278125,39.99608907849716],[-75.0478947362736,39.994092077997365],[-75.04942073732101,39.991269077473035],[-75.05991474009213,39.99153707655212],[-75.06417674130488,39.98603507576272],[-75.07560674489496,39.97804907320192],[-75.08583274758331,39.975110072730914],[-75.0963737514276,39.973989071649896],[-75.10809075472568,39.970340070377866],[-75.11949275804984,39.96538006898689],[-75.130592761085,39.958616067999394],[-75.13524076198945,39.95068506615781],[-75.13626976176727,39.94329006482181],[-75.13615276089004,39.932982062389286],[-75.13448575989705,39.92617606128306],[-75.12825475744691,39.91317205894587],[-75.13136475797998,39.89914605581192],[-75.13729775883013,39.889974053871384],[-75.13983375930421,39.88832505327637],[-75.12748475577101,39.8814880528113],[-75.13139175663898,39.87734905118881],[-75.12550775366094,39.87421505103696],[-75.12189775210982,39.86625604941526],[-75.11746675069632,39.86686005004458],[-75.11352374977912,39.86440904996678],[-75.1130567487399,39.85936304879299],[-75.10698774785986,39.86339004914096],[-75.10539074671274,39.85741504801099],[-75.09412374234647,39.851956048031695],[-75.08886074079987,39.844146046607406],[-75.0832737393581,39.84165904583625],[-75.0870207401366,39.83819404520299],[-75.08311473821068,39.83364404463776],[-75.08495373823263,39.8305320436286],[-75.0827777380278,39.827065043324666],[-75.08856173881586,39.82045904180725],[-75.086384737992,39.81348204004139],[-75.08052973648819,39.807839039859395],[-75.07368473349874,39.803049038673244],[-75.0764927341125,39.798430037428886],[-75.0704927318203,39.79360503676321],[-75.07673973311364,39.790064036457636],[-75.08194073491235,39.79133803583594],[-75.08707173620826,39.77958403354383],[-75.07798773379135,39.78087203434442],[-75.07441473248441,39.77397003292234],[-75.06969773071995,39.77611103323307],[-75.07200473123082,39.7797930343176],[-75.06472672982186,39.78460103530898],[-75.05651872652295,39.78241703540723],[-75.04932672428087,39.77848603479284],[-75.05008272395057,39.77388703348681],[-75.040681719968,39.760935031348474],[-75.03543771791013,39.75511403018072],[-75.02216071359216,39.74640502925597],[-75.02280171412777,39.740073027903456],[-75.020454712389,39.73550302736161],[-75.02425371358576,39.73059002623215],[-75.01567271072562,39.72604302534308],[-74.9984817049644,39.71921302469745],[-74.99438770278381,39.71602802444291],[-74.99423570231387,39.71123202352349],[-74.98755270010314,39.706709022134014],[-74.97180469522478,39.70224702224321],[-74.95919169170604,39.70307302311077],[-74.95308068964373,39.69908302247503],[-74.94367868595177,39.69836902269876],[-74.93652568338928,39.69494002159802],[-74.92709468018148,39.684980020134496],[-74.91856467709886,39.677799018918336],[-74.91492867560089,39.67053101796518],[-74.90886167325348,39.665310017017994],[-74.908633671549,39.648370013887],[-74.90481367023003,39.635229011140765],[-74.9027266697037,39.63188701090653],[-74.89235166588269,39.62487100998283],[-74.89248266539143,39.61918600830567],[-74.87726165959303,39.608360006558314],[-74.82063964502977,39.65716401813183],[-74.73621762230161,39.72978303644815]]]},properties:{geoid:”34007″,name:”Camden”,state_name:”New Jersey”,county_state_name:”Camden County, New Jersey”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:84.32,”60_65k_diff”:696.41,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:483.91,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.05,”27_65k_eptc”:446.7,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:446.7,”40_95k_eptc”:544.74,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:446.7,”40_65k_no_eptc”:544.74,”60_65k_no_eptc”:1156.83,”27_95k_no_eptc”:446.7,”40_95k_no_eptc”:544.74,”60_95k_no_eptc”:1156.83}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-75.27648380856465,39.976967065663814],[-75.28026780983244,39.97497206542008],[-75.27560780762192,39.97021906474194],[-75.26544980364223,39.96526506443908],[-75.26049280288733,39.96632106444813],[-75.25668780155495,39.963727064491216],[-75.2516047992097,39.96536406436446],[-75.24748079823507,39.96353606420025],[-75.25085179956602,39.95910706368437],[-75.24900779856233,39.95691506268733],[-75.25137779838263,39.94907306123053],[-75.24647079631123,39.94267505997928],[-75.24015079487219,39.94209406025893],[-75.2395717936933,39.938047059502395],[-75.23500379251298,39.938135060161436],[-75.23740879255114,39.93265605847782],[-75.24218779458201,39.9334340584135],[-75.24430279489678,39.92636105697975],[-75.24735779591492,39.9224450558541],[-75.24706979539987,39.91378605442581],[-75.25123879607685,39.91011805393618],[-75.25128979578021,39.90441105226635],[-75.25911379757001,39.89244404948053],[-75.2617447978604,39.89178204992937],[-75.26492979911272,39.881120047602096],[-75.26252979802,39.87656904618976],[-75.2484327928191,39.876493047064464],[-75.24047179077284,39.87238904624741],[-75.23412378842394,39.877189048087914],[-75.21977178410572,39.87548704824398],[-75.21146478134423,39.86701204694292],[-75.19985877817089,39.87323004793899],[-75.19273977591357,39.87901404980854],[-75.18789077464392,39.88110305023549],[-75.18011377152233,39.88220505071881],[-75.15065476239805,39.88351205179301],[-75.14374776080756,39.88500605286967],[-75.13983375930421,39.88832505327637],[-75.13729775883013,39.889974053871384],[-75.13136475797998,39.89914605581192],[-75.12825475744691,39.91317205894587],[-75.13448575989705,39.92617606128306],[-75.13615276089004,39.932982062389286],[-75.13626976176727,39.94329006482181],[-75.13524076198945,39.95068506615781],[-75.130592761085,39.958616067999394],[-75.11949275804984,39.96538006898689],[-75.10809075472568,39.970340070377866],[-75.0963737514276,39.973989071649896],[-75.08583274758331,39.975110072730914],[-75.07560674489496,39.97804907320192],[-75.06417674130488,39.98603507576272],[-75.05991474009213,39.99153707655212],[-75.05809074031995,39.99741207763138],[-75.05340673939644,40.004576079473544],[-75.04709173786219,40.00994908119662],[-75.04126873609978,40.012722081712305],[-75.02750173150193,40.01708708283509],[-75.01323872707184,40.02031108409219],[-75.00061872418942,40.02870808626663],[-74.97398271719369,40.0486030908],[-74.98489472090672,40.05729509224836],[-74.98037971945197,40.060357092846374],[-74.9808797205287,40.06603609418966],[-74.97106371743347,40.07373909613464],[-74.96314671533425,40.07733409723991],[-74.95884271371749,40.08251109853826],[-74.9579007147133,40.09057910003612],[-74.9557647138953,40.09499010103175],[-74.96134371508282,40.097504101309],[-74.96088771534161,40.10311210269701],[-74.96536071748805,40.10803210342569],[-74.96313071759009,40.114986104732324],[-74.96499271753848,40.11864310519633],[-74.97012072015207,40.11720910447144],[-74.97322072078013,40.11989910528396],[-74.98194872301495,40.12025310548229],[-74.98295972453359,40.12336110537968],[-74.99788672915464,40.127824105787525],[-75.01506773526432,40.13800010728869],[-75.02057273702499,40.13228210607614],[-75.05834374720045,40.10590009912808],[-75.07780675140404,40.08577809521407],[-75.08119075298815,40.08412409474058],[-75.0967347568816,40.068997091148304],[-75.08742675392568,40.063607090171274],[-75.09405775564326,40.056779088160766],[-75.10627175819961,40.04955608628073],[-75.10943275904889,40.045882085345696],[-75.13519476909268,40.061039087579026],[-75.17643978272574,40.08465709121581],[-75.18846278579434,40.07275808834632],[-75.22361179884183,40.09291509088647],[-75.25628780662858,40.06108908359789],[-75.26443280905767,40.05410208167315],[-75.25765680602933,40.04761908111073],[-75.2490408029551,40.041856079564916],[-75.246171802713,40.038298079265424],[-75.23232479731793,40.02811507750171],[-75.21805779294993,40.02095107677427],[-75.21222079025412,40.01546907627975],[-75.20577278807748,40.01163707511861],[-75.21062078938643,40.008660074478556],[-75.25612080202016,39.987309068486105],[-75.2636888049855,39.982666067605194],[-75.27648380856465,39.976967065663814]]]},properties:{geoid:”42101″,name:”Philadelphia”,state_name:”Pennsylvania”,county_state_name:”Philadelphia County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:7.86,”60_65k_diff”:534.04,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:321.54,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:384,”40_65k_eptc”:460.42,”60_65k_eptc”:460.41,”27_95k_eptc”:384,”40_95k_eptc”:468.28,”60_95k_eptc”:672.91,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.87,”27_65k_no_eptc”:384,”40_65k_no_eptc”:468.28,”60_65k_no_eptc”:994.45,”27_95k_no_eptc”:384,”40_95k_no_eptc”:468.28,”60_95k_no_eptc”:994.45}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-74.41739451131605,39.55726301275352],[-74.4143995101198,39.5609850137836],[-74.41883451262028,39.56859101471522],[-74.4103965094646,39.57102901578878],[-74.40516050847594,39.569601015739565],[-74.40082050665721,39.57225001642267],[-74.39767050578374,39.577794017416906],[-74.39760150667088,39.58152401825005],[-74.39230250518763,39.59456802050158],[-74.3904005044205,39.59604502085508],[-74.39036550689188,39.62980502852291],[-74.38970951486999,39.77329105705914],[-74.42941653124554,39.84541106955408],[-74.43422453428096,39.85516507145637],[-74.47151255034181,39.92493008414693],[-74.50637356446258,39.991233095911745],[-74.52869157466299,40.03745710435611],[-74.55310658464879,40.079138112480855],[-74.57950859650835,40.123550120190274],[-74.5878365995023,40.13826212303293],[-74.60242060439204,40.13698412191526],[-74.60330460476789,40.13863212211801],[-74.62338361156188,40.14271912183471],[-74.62316161119104,40.14864612379188],[-74.63022761310447,40.148829123240404],[-74.63799961661698,40.151897123624906],[-74.6385196170822,40.154364123614194],[-74.64885561977843,40.155794123743874],[-74.65198762127439,40.15898012448182],[-74.6614866242973,40.16220212483173],[-74.66202462469153,40.16493812537479],[-74.66970162719824,40.165238125111564],[-74.67675162911556,40.168528125067155],[-74.67562462934963,40.17267612662666],[-74.6844876328261,40.17796212744656],[-74.6905686343913,40.17688812696207],[-74.6962306362561,40.18276412749339],[-74.70828064029463,40.18191212737372],[-74.7126716416723,40.17441612510306],[-74.70842463995645,40.17185412476296],[-74.70627063858713,40.16180112274879],[-74.71292164056436,40.156103121614],[-74.71387464010259,40.1526611206345],[-74.72204964307696,40.15031911987713],[-74.72437064328328,40.14642011920948],[-74.74118564803922,40.13517311617581],[-74.75313165216582,40.13504111645373],[-74.76232465438055,40.132889115495985],[-74.78155666043655,40.12146211271386],[-74.7882886618967,40.12058711226329],[-74.79942266563017,40.122711112125714],[-74.81547767070428,40.12770211246821],[-74.82253267282333,40.12685211233942],[-74.8262276739847,40.12407411148847],[-74.83310467559953,40.11198010917348],[-74.8358696765202,40.103474106803],[-74.8422166776716,40.09851010543579],[-74.85374668148484,40.09393410442236],[-74.85763568191524,40.09022310393814],[-74.85972268277672,40.085319102763776],[-74.86549068430503,40.08214110204357],[-74.87753468821349,40.07996510123933],[-74.8859796900999,40.07697809979136],[-74.90731969706599,40.07080809828024],[-74.92189970203376,40.07145409707911],[-74.93504370571024,40.06784409604274],[-74.96689271495896,40.05272409184128],[-74.97398271719369,40.0486030908],[-75.00061872418942,40.02870808626663],[-75.01323872707184,40.02031108409219],[-75.02750173150193,40.01708708283509],[-75.04126873609978,40.012722081712305],[-75.04709173786219,40.00994908119662],[-75.05340673939644,40.004576079473544],[-75.05809074031995,39.99741207763138],[-75.05991474009213,39.99153707655212],[-75.04942073732101,39.991269077473035],[-75.0478947362736,39.994092077997365],[-75.03635573278125,39.99608907849716],[-75.02839573025787,39.991952078334265],[-75.01838872755296,39.9889620776347],[-75.01468772535576,39.985072076878474],[-75.01350472456076,39.9776810757354],[-75.01619872551248,39.97014807362419],[-75.019867726964,39.969369074112805],[-75.01760172473737,39.959383071684854],[-75.01309372345303,39.95663607173432],[-75.01616072423859,39.95046106995658],[-75.01508272307868,39.94682106951897],[-75.00906672183157,39.94512806952767],[-75.00415071963911,39.94147306863483],[-74.99442971621596,39.9393730688828],[-74.99181171597596,39.94092306926654],[-74.97558171064306,39.939621069129224],[-74.97508571058775,39.93781906918423],[-74.98142371248946,39.93111906744786],[-74.9838747130442,39.92680406669065],[-74.97428470903579,39.921429065509734],[-74.96420670564146,39.920684065777124],[-74.95590570325355,39.91322506465835],[-74.95253170095725,39.907126063722025],[-74.95194870129062,39.90168006284819],[-74.94936070015756,39.89817206178203],[-74.93074669345403,39.88591606072224],[-74.90554368027108,39.80106304429857],[-74.90296467871418,39.79111604226434],[-74.89863467733723,39.78970104223056],[-74.89482367609203,39.78332004072358],[-74.88981567457091,39.78199004134288],[-74.8761096690931,39.78148104141946],[-74.86948366723479,39.78434204245255],[-74.85322966290616,39.78731804307828],[-74.8432096594984,39.789927044410554],[-74.81942065235768,39.78800904496196],[-74.81711265068311,39.785794044317136],[-74.8061016477775,39.78302104410134],[-74.79072564146587,39.771311042729906],[-74.78529563973495,39.76576504148045],[-74.78120563777297,39.75859504031816],[-74.776938636333,39.757798039815455],[-74.77209163512897,39.75044403880141],[-74.76638663270714,39.74657003858943],[-74.75578162868815,39.74221503789601],[-74.73621762230161,39.72978303644815],[-74.67614260078523,39.69162503077289],[-74.67381560026969,39.68722002975509],[-74.669510598408,39.685035029513],[-74.66432859620309,39.676771028195674],[-74.66494059688242,39.67479202757367],[-74.66048059420172,39.66880702609458],[-74.65709659194387,39.64485002184694],[-74.65987759231568,39.63941702066975],[-74.65929659216648,39.63124101888618],[-74.6544655906084,39.62992601860689],[-74.65299958999766,39.62659501861209],[-74.64796558831347,39.625082017883926],[-74.63558858490353,39.62712401918918],[-74.63139758240465,39.625014018816486],[-74.627613581096,39.62039501795633],[-74.62474758137918,39.625765018758],[-74.62102957965547,39.62669901923382],[-74.6163285776076,39.62345201927493],[-74.61099657653655,39.6227790188195],[-74.59726657190386,39.614692017467],[-74.5887195681601,39.611810017905015],[-74.58512756695741,39.60496001598508],[-74.5801745653759,39.60286401577331],[-74.57575056388889,39.598403015138445],[-74.57171256229556,39.59894701517768],[-74.56333255927792,39.59672301531636],[-74.55324155673138,39.597748015998434],[-74.54904855459387,39.590320014343625],[-74.54198255234814,39.58582401416647],[-74.54264255190476,39.57912801269332],[-74.53851155084288,39.57452601203947],[-74.53239054850499,39.57337801188067],[-74.52763854669733,39.56963801093824],[-74.52354154585484,39.5695600117045],[-74.51702454331179,39.57415901273749],[-74.51223254178326,39.56996001197022],[-74.50591853949184,39.569653012163585],[-74.49486953539709,39.561348010589015],[-74.49398353492087,39.556221010007214],[-74.48635153348103,39.55821901079005],[-74.48049853086022,39.557047010642094],[-74.47566552963997,39.551468009492275],[-74.47183452776672,39.552002010002255],[-74.46776052656861,39.55567501087521],[-74.46216552512102,39.556102010804004],[-74.4595775242554,39.54858300972671],[-74.45344752211908,39.548581009545195],[-74.45261652226243,39.55692301088835],[-74.44672352003866,39.55906901211542],[-74.44356751982089,39.55476601082311],[-74.44613651966753,39.54975100988194],[-74.4419995186153,39.54278700854027],[-74.43612051646107,39.54127300884802],[-74.43344851595359,39.543847009101206],[-74.43835151700493,39.55132101045312],[-74.43536951659028,39.555439011287774],[-74.42539351398851,39.55352901149502],[-74.41739451131605,39.55726301275352]]]},properties:{geoid:”34005″,name:”Burlington”,state_name:”New Jersey”,county_state_name:”Burlington County, New Jersey”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:84.32,”60_65k_diff”:696.41,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:483.91,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.05,”27_65k_eptc”:446.7,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:446.7,”40_95k_eptc”:544.74,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:446.7,”40_65k_no_eptc”:544.74,”60_65k_no_eptc”:1156.83,”27_95k_no_eptc”:446.7,”40_95k_no_eptc”:544.74,”60_95k_no_eptc”:1156.83}},{type:”Feature”,geometry:{type:”MultiPolygon”,coordinates:[[[[-75.59488189980355,39.837533026428815],[-75.59774390170347,39.84115502703176],[-75.59486690107482,39.84490702826954],[-75.59199890015077,39.852543029914884],[-75.59873890304111,39.85420802990197],[-75.60138590322504,39.85684203053564],[-75.596407901847,39.86297903197943],[-75.59363190229317,39.8700040331102],[-75.59791590301599,39.87447203415682],[-75.5711638953457,39.888144037444846],[-75.57425489758769,39.89216103835564],[-75.57338289687539,39.89640503883524],[-75.54641788999645,39.90973904282703],[-75.55045589129811,39.91493904388387],[-75.54249588920796,39.91842504434274],[-75.54439688967663,39.92340904535605],[-75.54273588945748,39.927189046718844],[-75.53611088719758,39.92993404712199],[-75.53023988529385,39.922131046143434],[-75.52350688269358,39.923150046820346],[-75.53047688586032,39.93205704762766],[-75.52396088385011,39.93180604813067],[-75.51896488182055,39.93431004916667],[-75.51954288276414,39.9389640500684],[-75.52381788468112,39.94413205041961],[-75.50213687843824,39.954375053704794],[-75.46195586682663,39.97281905841016],[-75.43581785925566,39.98506706205117],[-75.43563185890932,39.98883806282589],[-75.44310186154269,39.99371606371632],[-75.4537728649486,39.99359706286096],[-75.42260185686298,40.0147110681606],[-75.40439585147054,40.02744207117973],[-75.41499285651433,40.04179507350612],[-75.36106783995939,40.06555108012171],[-75.3666888426253,40.07236308129776],[-75.39263384953115,40.060982078213875],[-75.40564885565985,40.07856808191291],[-75.42012586126087,40.09720908467141],[-75.4378658659182,40.0895810826318],[-75.44072286789972,40.094330083389686],[-75.45618787201956,40.08778408146829],[-75.45666787272945,40.094461083047584],[-75.4629278743461,40.09726108277284],[-75.46173087503037,40.10304308417319],[-75.46896287715671,40.107069085220395],[-75.47160487822006,40.11186108546304],[-75.47036287783406,40.11573508631903],[-75.46322987549541,40.11922308719879],[-75.46128987616535,40.12209308765784],[-75.46351087605042,40.126157089160024],[-75.47245187980738,40.129306089446544],[-75.4810848822364,40.12680408853447],[-75.49368988641507,40.12650108744598],[-75.50562589060385,40.13264208827148],[-75.51038989193017,40.13830308924822],[-75.50865489160248,40.146539091513894],[-75.50330289015409,40.15110309183376],[-75.50065789068874,40.15562709317128],[-75.50271989057715,40.15920409414345],[-75.50896789344752,40.16009909412036],[-75.51321589378144,40.158304093357316],[-75.5185208955468,40.14851009147598],[-75.52594689761081,40.1486190910595],[-75.52777789849407,40.15311509138315],[-75.52661689877549,40.15857009310739],[-75.52894290035755,40.16840409486562],[-75.54098790398295,40.17595909544525],[-75.54938290811222,40.190045098555004],[-75.55339290943652,40.200362100042454],[-75.55714991123025,40.20722110096788],[-75.56112691307196,40.20982310174031],[-75.56490791341112,40.206193100539316],[-75.56253891270893,40.20207410003471],[-75.56287991271837,40.19736909922404],[-75.56701691380471,40.194288098049746],[-75.57333991551167,40.19531109810817],[-75.57973691797187,40.201829099356736],[-75.58109991870141,40.206412099986984],[-75.58775892153263,40.21445710193059],[-75.59474892412118,40.23038110454336],[-75.59667592582869,40.23658310547881],[-75.60423692803357,40.23787210525315],[-75.60746992936313,40.23278110450186],[-75.60317492693513,40.22701410323691],[-75.61237492937786,40.22300510269539],[-75.61627993078706,40.2249191028569],[-75.61893693207013,40.229448103776996],[-75.63449793710899,40.2357541042799],[-75.64025593968655,40.2370621044159],[-75.65107594276307,40.24208510499035],[-75.65759694471552,40.24140110440724],[-75.66403794727525,40.24490810451071],[-75.67120095029023,40.24458410401852],[-75.6766719517506,40.24230110336042],[-75.68557995362755,40.23658310236091],[-75.69055595500556,40.23664110191797],[-75.6967839577076,40.241871102616024],[-75.72986496743619,40.224497098742056],[-75.74317997133569,40.21672909626344],[-75.82098199284783,40.16972408396817],[-75.84651799951325,40.153806080524966],[-75.8546130021137,40.14926907931486],[-75.87337700684066,40.13711507552625],[-75.89045901154005,40.12953907385453],[-75.9125500178963,40.12064107142718],[-75.94299902722952,40.109274067827414],[-75.9361370228447,40.07859306235227],[-75.93622702203871,40.06529305914588],[-75.93433402014583,40.04757405595825],[-75.93587202029454,40.03747405423364],[-75.96748002714119,39.99444704430827],[-75.98670403215702,39.967248037993805],[-75.98616503210916,39.96389503705363],[-75.99463103391935,39.952437035001225],[-75.99104203203079,39.947584034288525],[-75.98880203077377,39.94084903254068],[-75.98096802856189,39.9334870312919],[-75.99146903106299,39.929011030754424],[-75.99713403209313,39.92207002881219],[-75.99489803196586,39.916593027593564],[-75.99751803160089,39.90989902642681],[-75.99333102985932,39.89900402448507],[-75.98682502769736,39.89220002335736],[-75.99126002826097,39.88759902201258],[-75.99234902845535,39.88216802109731],[-75.986700026534,39.87438502009404],[-75.99164602731103,39.86872101850446],[-76.00243403108041,39.874361018964436],[-76.00447403123238,39.87218601850451],[-76.00857703123432,39.851973014582825],[-76.01991203492175,39.853532014145195],[-76.0228250355705,39.849852013946254],[-76.01781103422925,39.83818101152455],[-76.01647503293113,39.8314890104066],[-76.02282803488636,39.830808009288106],[-76.02703603525897,39.82416100784893],[-76.0379550389226,39.82591700809677],[-76.03107403665031,39.817534007190716],[-76.02992703604818,39.8125130055108],[-76.0352180380907,39.81184300586898],[-76.03512503688907,39.80815100439025],[-76.03850303770592,39.80173800351471],[-76.04574003980373,39.80099700316967],[-76.04136703878639,39.79720400248761],[-76.04852704045996,39.789248000187754],[-76.04968004074301,39.783791999209654],[-76.05839904247232,39.77986899864349],[-76.0605260431944,39.775018997371895],[-76.06492504477254,39.77029099597582],[-76.0624700436269,39.76510599509829],[-76.06742904397755,39.75965799355292],[-76.07646304796523,39.761820994017484],[-76.0818540491762,39.76135899378987],[-76.08579605019615,39.75589799262164],[-76.08260104917642,39.75305799221489],[-76.08433604900421,39.74834999096716],[-76.09204205096992,39.7431239895248],[-76.09687905317664,39.74311898983771],[-76.10205205455156,39.73989198880991],[-76.096190051579,39.737243988037385],[-76.09262205086745,39.733541987589945],[-76.10248105375963,39.72404098519086],[-76.10796205514053,39.725381986084166],[-76.11117905620132,39.728528986590284],[-76.10856705619726,39.73484398787865],[-76.11361805746253,39.737132988133304],[-76.11992605991716,39.736371987698156],[-76.12030605874176,39.72985598626015],[-76.11852305897672,39.72643998575101],[-76.12225405965525,39.72341498467617],[-76.12826406195263,39.72766498541913],[-76.1364530640474,39.72568998452688],[-76.13548606317389,39.721154983394364],[-76.02557802888273,39.72174498756716],[-75.96215200943685,39.72179999022777],[-75.84173297122351,39.721978995130044],[-75.78859795420743,39.72220699721962],[-75.77378794930112,39.722207997710704],[-75.76636494831922,39.737494000527256],[-75.75405794530192,39.75618600522821],[-75.74203094237079,39.77026400796413],[-75.73299793992243,39.77911501016377],[-75.71950393638274,39.79037301323469],[-75.70009093168886,39.80348601623808],[-75.6804699260872,39.8139470186002],[-75.66660192191412,39.81997102078859],[-75.64234591433524,39.82822502357378],[-75.62434890893473,39.83270302519231],[-75.61036590508304,39.835368025415335],[-75.59488189980355,39.837533026428815]]],[[[-75.59310089976104,39.8377310267107],[-75.5799278957566,39.83887002766236],[-75.58382689745486,39.84303002792042],[-75.58917189903828,39.843221028418206],[-75.59310089976104,39.8377310267107]]]]},properties:{geoid:”42029″,name:”Chester”,state_name:”Pennsylvania”,county_state_name:”Chester County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:49.1,”60_65k_diff”:621.62,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:409.12,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:417.82,”40_65k_eptc”:460.42,”60_65k_eptc”:460.41,”27_95k_eptc”:417.82,”40_95k_eptc”:509.52,”60_95k_eptc”:672.91,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.87,”27_65k_no_eptc”:417.82,”40_65k_no_eptc”:509.52,”60_65k_no_eptc”:1082.03,”27_95k_no_eptc”:417.82,”40_95k_no_eptc”:509.52,”60_95k_no_eptc”:1082.03}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-74.87726165959303,39.608360006558314],[-74.89248266539143,39.61918600830567],[-74.89235166588269,39.62487100998283],[-74.9027266697037,39.63188701090653],[-74.90481367023003,39.635229011140765],[-74.908633671549,39.648370013887],[-74.90886167325348,39.665310017017994],[-74.91492867560089,39.67053101796518],[-74.91856467709886,39.677799018918336],[-74.92709468018148,39.684980020134496],[-74.93652568338928,39.69494002159802],[-74.94367868595177,39.69836902269876],[-74.95308068964373,39.69908302247503],[-74.95919169170604,39.70307302311077],[-74.97180469522478,39.70224702224321],[-74.98755270010314,39.706709022134014],[-74.99423570231387,39.71123202352349],[-74.99438770278381,39.71602802444291],[-74.9984817049644,39.71921302469745],[-75.01567271072562,39.72604302534308],[-75.02425371358576,39.73059002623215],[-75.020454712389,39.73550302736161],[-75.02280171412777,39.740073027903456],[-75.02216071359216,39.74640502925597],[-75.03543771791013,39.75511403018072],[-75.040681719968,39.760935031348474],[-75.05008272395057,39.77388703348681],[-75.04932672428087,39.77848603479284],[-75.05651872652295,39.78241703540723],[-75.06472672982186,39.78460103530898],[-75.07200473123082,39.7797930343176],[-75.06969773071995,39.77611103323307],[-75.07441473248441,39.77397003292234],[-75.07798773379135,39.78087203434442],[-75.08707173620826,39.77958403354383],[-75.08194073491235,39.79133803583594],[-75.07673973311364,39.790064036457636],[-75.0704927318203,39.79360503676321],[-75.0764927341125,39.798430037428886],[-75.07368473349874,39.803049038673244],[-75.08052973648819,39.807839039859395],[-75.086384737992,39.81348204004139],[-75.08856173881586,39.82045904180725],[-75.0827777380278,39.827065043324666],[-75.08495373823263,39.8305320436286],[-75.08311473821068,39.83364404463776],[-75.0870207401366,39.83819404520299],[-75.0832737393581,39.84165904583625],[-75.08886074079987,39.844146046607406],[-75.09412374234647,39.851956048031695],[-75.10539074671274,39.85741504801099],[-75.10698774785986,39.86339004914096],[-75.1130567487399,39.85936304879299],[-75.11352374977912,39.86440904996678],[-75.11746675069632,39.86686005004458],[-75.12189775210982,39.86625604941526],[-75.12550775366094,39.87421505103696],[-75.13139175663898,39.87734905118881],[-75.12748475577101,39.8814880528113],[-75.13983375930421,39.88832505327637],[-75.14374776080756,39.88500605286967],[-75.15065476239805,39.88351205179301],[-75.18011377152233,39.88220505071881],[-75.18789077464392,39.88110305023549],[-75.19273977591357,39.87901404980854],[-75.19985877817089,39.87323004793899],[-75.21146478134423,39.86701204694292],[-75.2286357855709,39.85856804422963],[-75.24615079081717,39.85399004280193],[-75.27220379899049,39.84908404115056],[-75.29337780582593,39.84879004008671],[-75.30967581104208,39.85018603953145],[-75.33043381763127,39.84902103842327],[-75.3424238205916,39.845853037736966],[-75.35440282400224,39.83992503571415],[-75.37173182880403,39.827567032759106],[-75.39841883657019,39.81047502816283],[-75.41506384127008,39.80192702624302],[-75.4054908380238,39.79637602586484],[-75.41933084148889,39.789733023821064],[-75.41739984099821,39.78563402333688],[-75.41351183946632,39.785019022931074],[-75.4075188376215,39.787248023714504],[-75.40592983697928,39.78113002268537],[-75.40232583667202,39.78247702301841],[-75.40010583536198,39.77736202204997],[-75.40039583470097,39.772978020999126],[-75.39736883405463,39.76924202023228],[-75.40492383638721,39.76905102026999],[-75.40596083647276,39.763492019029535],[-75.40320583514153,39.76126101818425],[-75.39611983329586,39.761388018534696],[-75.38996683064995,39.759667018604404],[-75.39117183071309,39.7553170182631],[-75.39466383235144,39.75312501745697],[-75.39184083058144,39.75001601707078],[-75.38790482995934,39.75176201766853],[-75.38584882880467,39.74697701611485],[-75.37862882677369,39.747038016196335],[-75.37481082527053,39.73716201457364],[-75.376636824705,39.72658001262332],[-75.36929482245344,39.72199301174676],[-75.36724082125572,39.717573011504456],[-75.3606178189232,39.7140310103799],[-75.35025381495625,39.71125501075545],[-75.34742981451429,39.7071160095282],[-75.33683581126692,39.70429900990095],[-75.3345838094952,39.69980500867344],[-75.32742380679463,39.696623008795726],[-75.32672180702605,39.690380007280744],[-75.31671580335603,39.691405008032596],[-75.31039480182429,39.68903800748629],[-75.30645280012415,39.689540008066544],[-75.29514679685767,39.686162007325244],[-75.28600079348728,39.6795960063291],[-75.27602279053916,39.680432007214186],[-75.26846978802641,39.682271007313425],[-75.26197078514454,39.68172400752399],[-75.25122778233515,39.67661600757918],[-75.25070578118712,39.66862800571761],[-75.24747577988437,39.66449400458014],[-75.23345477557088,39.6614380047638],[-75.22393177298777,39.66308500505683],[-75.2193747707489,39.66183000561467],[-75.21294676941305,39.66451200638528],[-75.19979476460819,39.66700400670331],[-75.10992773284912,39.603325997452636],[-75.07705572084431,39.57939199368372],[-75.06185571524799,39.568753991917795],[-74.98527268889309,39.51497498419964],[-74.87726165959303,39.608360006558314]]]},properties:{geoid:”34015″,name:”Gloucester”,state_name:”New Jersey”,county_state_name:”Gloucester County, New Jersey”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:84.32,”60_65k_diff”:696.41,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:483.91,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.05,”27_65k_eptc”:446.7,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:446.7,”40_95k_eptc”:544.74,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:446.7,”40_65k_no_eptc”:544.74,”60_65k_no_eptc”:1156.83,”27_95k_no_eptc”:446.7,”40_95k_no_eptc”:544.74,”60_95k_no_eptc”:1156.83}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-75.01506773526432,40.13800010728869],[-75.12627777403594,40.20381911612004],[-75.15977778599002,40.22414111930843],[-75.19768179929923,40.24765612286578],[-75.29430583383282,40.304367129996116],[-75.3253418453356,40.32343313309034],[-75.42223587959006,40.38169914032937],[-75.42566888076662,40.38443814053879],[-75.48405890155193,40.41845914544603],[-75.52969591821261,40.447003149286964],[-75.54271092043132,40.43061514547811],[-75.58783893106536,40.375062133343455],[-75.60028993402975,40.360173129461955],[-75.62489494055846,40.32978112305517],[-75.6967839577076,40.241871102616024],[-75.69055595500556,40.23664110191797],[-75.68557995362755,40.23658310236091],[-75.6766719517506,40.24230110336042],[-75.67120095029023,40.24458410401852],[-75.66403794727525,40.24490810451071],[-75.65759694471552,40.24140110440724],[-75.65107594276307,40.24208510499035],[-75.64025593968655,40.2370621044159],[-75.63449793710899,40.2357541042799],[-75.61893693207013,40.229448103776996],[-75.61627993078706,40.2249191028569],[-75.61237492937786,40.22300510269539],[-75.60317492693513,40.22701410323691],[-75.60746992936313,40.23278110450186],[-75.60423692803357,40.23787210525315],[-75.59667592582869,40.23658310547881],[-75.59474892412118,40.23038110454336],[-75.58775892153263,40.21445710193059],[-75.58109991870141,40.206412099986984],[-75.57973691797187,40.201829099356736],[-75.57333991551167,40.19531109810817],[-75.56701691380471,40.194288098049746],[-75.56287991271837,40.19736909922404],[-75.56253891270893,40.20207410003471],[-75.56490791341112,40.206193100539316],[-75.56112691307196,40.20982310174031],[-75.55714991123025,40.20722110096788],[-75.55339290943652,40.200362100042454],[-75.54938290811222,40.190045098555004],[-75.54098790398295,40.17595909544525],[-75.52894290035755,40.16840409486562],[-75.52661689877549,40.15857009310739],[-75.52777789849407,40.15311509138315],[-75.52594689761081,40.1486190910595],[-75.5185208955468,40.14851009147598],[-75.51321589378144,40.158304093357316],[-75.50896789344752,40.16009909412036],[-75.50271989057715,40.15920409414345],[-75.50065789068874,40.15562709317128],[-75.50330289015409,40.15110309183376],[-75.50865489160248,40.146539091513894],[-75.51038989193017,40.13830308924822],[-75.50562589060385,40.13264208827148],[-75.49368988641507,40.12650108744598],[-75.4810848822364,40.12680408853447],[-75.47245187980738,40.129306089446544],[-75.46351087605042,40.126157089160024],[-75.46128987616535,40.12209308765784],[-75.46322987549541,40.11922308719879],[-75.47036287783406,40.11573508631903],[-75.47160487822006,40.11186108546304],[-75.46896287715671,40.107069085220395],[-75.46173087503037,40.10304308417319],[-75.4629278743461,40.09726108277284],[-75.45666787272945,40.094461083047584],[-75.45618787201956,40.08778408146829],[-75.44072286789972,40.094330083389686],[-75.4378658659182,40.0895810826318],[-75.42012586126087,40.09720908467141],[-75.40564885565985,40.07856808191291],[-75.39263384953115,40.060982078213875],[-75.3666888426253,40.07236308129776],[-75.36106783995939,40.06555108012171],[-75.35653583918408,40.06279507982717],[-75.3494588358136,40.052913078506336],[-75.32070082406942,40.016224072133156],[-75.31143382189082,40.019818072940176],[-75.29282681410075,39.996886069513955],[-75.28392981087089,39.98722506795518],[-75.27648380856465,39.976967065663814],[-75.2636888049855,39.982666067605194],[-75.25612080202016,39.987309068486105],[-75.21062078938643,40.008660074478556],[-75.20577278807748,40.01163707511861],[-75.21222079025412,40.01546907627975],[-75.21805779294993,40.02095107677427],[-75.23232479731793,40.02811507750171],[-75.246171802713,40.038298079265424],[-75.2490408029551,40.041856079564916],[-75.25765680602933,40.04761908111073],[-75.26443280905767,40.05410208167315],[-75.25628780662858,40.06108908359789],[-75.22361179884183,40.09291509088647],[-75.18846278579434,40.07275808834632],[-75.17643978272574,40.08465709121581],[-75.13519476909268,40.061039087579026],[-75.10943275904889,40.045882085345696],[-75.10627175819961,40.04955608628073],[-75.09405775564326,40.056779088160766],[-75.08742675392568,40.063607090171274],[-75.0967347568816,40.068997091148304],[-75.08119075298815,40.08412409474058],[-75.07780675140404,40.08577809521407],[-75.05834374720045,40.10590009912808],[-75.02057273702499,40.13228210607614],[-75.01506773526432,40.13800010728869]]]},properties:{geoid:”42091″,name:”Montgomery”,state_name:”Pennsylvania”,county_state_name:”Montgomery County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:7.86,”60_65k_diff”:534.04,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:321.54,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:384,”40_65k_eptc”:460.42,”60_65k_eptc”:460.41,”27_95k_eptc”:384,”40_95k_eptc”:468.28,”60_95k_eptc”:672.91,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.87,”27_65k_no_eptc”:384,”40_65k_no_eptc”:468.28,”60_65k_no_eptc”:994.45,”27_95k_no_eptc”:384,”40_95k_no_eptc”:468.28,”60_95k_no_eptc”:994.45}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-75.41506384127008,39.80192702624302],[-75.39841883657019,39.81047502816283],[-75.37173182880403,39.827567032759106],[-75.35440282400224,39.83992503571415],[-75.3424238205916,39.845853037736966],[-75.33043381763127,39.84902103842327],[-75.30967581104208,39.85018603953145],[-75.29337780582593,39.84879004008671],[-75.27220379899049,39.84908404115056],[-75.24615079081717,39.85399004280193],[-75.2286357855709,39.85856804422963],[-75.21146478134423,39.86701204694292],[-75.21977178410572,39.87548704824398],[-75.23412378842394,39.877189048087914],[-75.24047179077284,39.87238904624741],[-75.2484327928191,39.876493047064464],[-75.26252979802,39.87656904618976],[-75.26492979911272,39.881120047602096],[-75.2617447978604,39.89178204992937],[-75.25911379757001,39.89244404948053],[-75.25128979578021,39.90441105226635],[-75.25123879607685,39.91011805393618],[-75.24706979539987,39.91378605442581],[-75.24735779591492,39.9224450558541],[-75.24430279489678,39.92636105697975],[-75.24218779458201,39.9334340584135],[-75.23740879255114,39.93265605847782],[-75.23500379251298,39.938135060161436],[-75.2395717936933,39.938047059502395],[-75.24015079487219,39.94209406025893],[-75.24647079631123,39.94267505997928],[-75.25137779838263,39.94907306123053],[-75.24900779856233,39.95691506268733],[-75.25085179956602,39.95910706368437],[-75.24748079823507,39.96353606420025],[-75.2516047992097,39.96536406436446],[-75.25668780155495,39.963727064491216],[-75.26049280288733,39.96632106444813],[-75.26544980364223,39.96526506443908],[-75.27560780762192,39.97021906474194],[-75.28026780983244,39.97497206542008],[-75.27648380856465,39.976967065663814],[-75.28392981087089,39.98722506795518],[-75.29282681410075,39.996886069513955],[-75.31143382189082,40.019818072940176],[-75.32070082406942,40.016224072133156],[-75.3494588358136,40.052913078506336],[-75.35653583918408,40.06279507982717],[-75.36106783995939,40.06555108012171],[-75.41499285651433,40.04179507350612],[-75.40439585147054,40.02744207117973],[-75.42260185686298,40.0147110681606],[-75.4537728649486,39.99359706286096],[-75.44310186154269,39.99371606371632],[-75.43563185890932,39.98883806282589],[-75.43581785925566,39.98506706205117],[-75.46195586682663,39.97281905841016],[-75.50213687843824,39.954375053704794],[-75.52381788468112,39.94413205041961],[-75.51954288276414,39.9389640500684],[-75.51896488182055,39.93431004916667],[-75.52396088385011,39.93180604813067],[-75.53047688586032,39.93205704762766],[-75.52350688269358,39.923150046820346],[-75.53023988529385,39.922131046143434],[-75.53611088719758,39.92993404712199],[-75.54273588945748,39.927189046718844],[-75.54439688967663,39.92340904535605],[-75.54249588920796,39.91842504434274],[-75.55045589129811,39.91493904388387],[-75.54641788999645,39.90973904282703],[-75.57338289687539,39.89640503883524],[-75.57425489758769,39.89216103835564],[-75.5711638953457,39.888144037444846],[-75.59791590301599,39.87447203415682],[-75.59363190229317,39.8700040331102],[-75.596407901847,39.86297903197943],[-75.60138590322504,39.85684203053564],[-75.59873890304111,39.85420802990197],[-75.59199890015077,39.852543029914884],[-75.59486690107482,39.84490702826954],[-75.59774390170347,39.84115502703176],[-75.59488189980355,39.837533026428815],[-75.59310089976104,39.8377310267107],[-75.58917189903828,39.843221028418206],[-75.58382689745486,39.84303002792042],[-75.5799278957566,39.83887002766236],[-75.55740488861024,39.83951502845034],[-75.53497888103709,39.838539029448185],[-75.52030787631298,39.83701302916815],[-75.49834686986841,39.83338802972945],[-75.48104086406371,39.829327029295946],[-75.46818885973654,39.82557902905007],[-75.45349185457304,39.820465028949954],[-75.44050885059772,39.81515002770103],[-75.42310584380418,39.806717026961586],[-75.41506384127008,39.80192702624302]]]},properties:{geoid:”42045″,name:”Delaware”,state_name:”Pennsylvania”,county_state_name:”Delaware County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:7.86,”60_65k_diff”:534.04,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:321.54,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:384,”40_65k_eptc”:460.42,”60_65k_eptc”:460.41,”27_95k_eptc”:384,”40_95k_eptc”:468.28,”60_95k_eptc”:672.91,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.87,”27_65k_no_eptc”:384,”40_65k_no_eptc”:468.28,”60_65k_no_eptc”:994.45,”27_95k_no_eptc”:384,”40_95k_no_eptc”:468.28,”60_95k_no_eptc”:994.45}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-74.94291072506262,40.34169115003049],[-74.94451872557475,40.34507115032733],[-74.94712372708234,40.360217153729764],[-74.95578673097813,40.38003615716636],[-74.96147973314658,40.38894315840807],[-74.96443273547577,40.39595616005761],[-74.96750073652979,40.39882116095418],[-74.9831327408949,40.40460716144947],[-74.98841474291659,40.40850216185527],[-74.99586174621854,40.4103921621123],[-75.02302975368815,40.403701159295224],[-75.03177975692786,40.40482115895903],[-75.04552776197731,40.41368716091873],[-75.05762076647699,40.41734416115614],[-75.0609187672136,40.42174516134633],[-75.06651677062334,40.447184166099944],[-75.07060977276417,40.45620416848184],[-75.06701777235786,40.465316170327995],[-75.06771677216157,40.473677171439256],[-75.06276277200092,40.48003417339753],[-75.0625777721967,40.494082175798276],[-75.06484377347168,40.5035111774267],[-75.06568977464873,40.522114180748964],[-75.065091775338,40.52628618197333],[-75.06810177664502,40.54149618469968],[-75.07513977893316,40.54558718552901],[-75.09982878824623,40.5674061890322],[-75.11553779418186,40.5728681896667],[-75.13499680039676,40.575670189497686],[-75.1401738016437,40.57537818924043],[-75.14875880410855,40.571827188072575],[-75.15785380661316,40.565432185918276],[-75.16231580805844,40.56420118575598],[-75.17287881228086,40.56443118551487],[-75.18125281463931,40.566723185254055],[-75.18827181666082,40.570555186373724],[-75.19549782030921,40.57863518703029],[-75.19415182010557,40.58285118858486],[-75.18969381798873,40.58767918989849],[-75.18960181860332,40.59178419017929],[-75.19229282053661,40.6026841922697],[-75.19680482235896,40.60858819294119],[-75.23684983409146,40.59075618799709],[-75.25815283944443,40.58201718539675],[-75.29352985026722,40.56198618065717],[-75.3335158607908,40.53706517411074],[-75.33863486251805,40.53407617314423],[-75.36661187064225,40.51543216858609],[-75.40973488230416,40.48799216160751],[-75.48405890155193,40.41845914544603],[-75.42566888076662,40.38443814053879],[-75.42223587959006,40.38169914032937],[-75.3253418453356,40.32343313309034],[-75.29430583383282,40.304367129996116],[-75.19768179929923,40.24765612286578],[-75.15977778599002,40.22414111930843],[-75.12627777403594,40.20381911612004],[-75.01506773526432,40.13800010728869],[-74.99788672915464,40.127824105787525],[-74.98295972453359,40.12336110537968],[-74.98194872301495,40.12025310548229],[-74.97322072078013,40.11989910528396],[-74.97012072015207,40.11720910447144],[-74.96499271753848,40.11864310519633],[-74.96313071759009,40.114986104732324],[-74.96536071748805,40.10803210342569],[-74.96088771534161,40.10311210269701],[-74.96134371508282,40.097504101309],[-74.9557647138953,40.09499010103175],[-74.9579007147133,40.09057910003612],[-74.95884271371749,40.08251109853826],[-74.96314671533425,40.07733409723991],[-74.97106371743347,40.07373909613464],[-74.9808797205287,40.06603609418966],[-74.98037971945197,40.060357092846374],[-74.98489472090672,40.05729509224836],[-74.97398271719369,40.0486030908],[-74.96689271495896,40.05272409184128],[-74.93504370571024,40.06784409604274],[-74.92189970203376,40.07145409707911],[-74.90731969706599,40.07080809828024],[-74.8859796900999,40.07697809979136],[-74.87753468821349,40.07996510123933],[-74.86549068430503,40.08214110204357],[-74.85972268277672,40.085319102763776],[-74.85763568191524,40.09022310393814],[-74.85374668148484,40.09393410442236],[-74.8422166776716,40.09851010543579],[-74.8358696765202,40.103474106803],[-74.83310467559953,40.11198010917348],[-74.8262276739847,40.12407411148847],[-74.82253267282333,40.12685211233942],[-74.81547767070428,40.12770211246821],[-74.79942266563017,40.122711112125714],[-74.7882886618967,40.12058711226329],[-74.78155666043655,40.12146211271386],[-74.76232465438055,40.132889115495985],[-74.75313165216582,40.13504111645373],[-74.74118564803922,40.13517311617581],[-74.72437064328328,40.14642011920948],[-74.72204964307696,40.15031911987713],[-74.72232664386269,40.16073512188688],[-74.73380564792959,40.174517124655296],[-74.73720664987542,40.17761712495054],[-74.75430665497106,40.18521712631619],[-74.75950665758184,40.19691712797242],[-74.76699066107916,40.20668213014578],[-74.77140566266358,40.21515213168926],[-74.78120766643461,40.22151613249026],[-74.79530767046431,40.22941613308115],[-74.81950867919748,40.23851613447006],[-74.82390868083233,40.24151613471451],[-74.83630868533632,40.24621613481809],[-74.84230968719118,40.250516136039096],[-74.84800968989063,40.26171613771238],[-74.85310969178018,40.269715139211534],[-74.86049369543751,40.28459214161986],[-74.86820969765078,40.2952141436736],[-74.8871107055738,40.31031514605346],[-74.89641070797572,40.31511514700284],[-74.90831171215304,40.31691514624341],[-74.9174117154447,40.32241414706429],[-74.93971272344207,40.338014149372235],[-74.94291072506262,40.34169115003049]]]},properties:{geoid:”42017″,name:”Bucks”,state_name:”Pennsylvania”,county_state_name:”Bucks County, Pennsylvania”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.18,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:7.86,”60_65k_diff”:534.04,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:321.54,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.04,”27_65k_eptc”:384,”40_65k_eptc”:460.42,”60_65k_eptc”:460.41,”27_95k_eptc”:384,”40_95k_eptc”:468.28,”60_95k_eptc”:672.91,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.18,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.87,”27_65k_no_eptc”:384,”40_65k_no_eptc”:468.28,”60_65k_no_eptc”:994.45,”27_95k_no_eptc”:384,”40_95k_no_eptc”:468.28,”60_95k_no_eptc”:994.45}},{type:”Feature”,geometry:{type:”Polygon”,coordinates:[[[-74.48496357336015,40.25333314887041],[-74.48192857401183,40.2738301532803],[-74.49761857980387,40.28054215360073],[-74.50162758058933,40.27951615365521],[-74.50881158268841,40.281891153571536],[-74.51485658544321,40.287146154567665],[-74.51976258731437,40.287070154159395],[-74.52157658722764,40.290042154745336],[-74.52939459052133,40.29425515559322],[-74.53658359206374,40.289494154536136],[-74.54215959391915,40.29168915501512],[-74.55669959825482,40.291664154073395],[-74.56087760046438,40.29601815451986],[-74.57952260701995,40.30382115593071],[-74.58407060907251,40.308193156723064],[-74.58558860989045,40.31325015754974],[-74.59505161304139,40.31585915757581],[-74.60025961368504,40.315469157477466],[-74.6033236150457,40.32141015843454],[-74.61404261958734,40.32459815891694],[-74.62265262177075,40.32532215860921],[-74.62438262309018,40.329328158879484],[-74.62327562242803,40.334433160497134],[-74.63059762504047,40.339613161084635],[-74.62582862445404,40.35640416478318],[-74.62521762541195,40.36312916573454],[-74.62024162405832,40.37375716810516],[-74.61759762336425,40.37727716911724],[-74.62252062569804,40.384304170300005],[-74.6539296358565,40.39105617001987],[-74.67450664209176,40.38429116847247],[-74.70080865045682,40.38065116619413],[-74.71816465549215,40.376787165527524],[-74.72206265604497,40.37521316475652],[-74.7349936616968,40.39905716858833],[-74.74814866781051,40.42416417347584],[-74.80847168615138,40.416672169440076],[-74.80201768251733,40.38498016379092],[-74.86967970383932,40.377782159612416],[-74.85626369719441,40.34670415403421],[-74.932278721511,40.33943515027951],[-74.94291072506262,40.34169115003049],[-74.93971272344207,40.338014149372235],[-74.9174117154447,40.32241414706429],[-74.90831171215304,40.31691514624341],[-74.89641070797572,40.31511514700284],[-74.8871107055738,40.31031514605346],[-74.86820969765078,40.2952141436736],[-74.86049369543751,40.28459214161986],[-74.85310969178018,40.269715139211534],[-74.84800968989063,40.26171613771238],[-74.84230968719118,40.250516136039096],[-74.83630868533632,40.24621613481809],[-74.82390868083233,40.24151613471451],[-74.81950867919748,40.23851613447006],[-74.79530767046431,40.22941613308115],[-74.78120766643461,40.22151613249026],[-74.77140566266358,40.21515213168926],[-74.76699066107916,40.20668213014578],[-74.75950665758184,40.19691712797242],[-74.75430665497106,40.18521712631619],[-74.73720664987542,40.17761712495054],[-74.73380564792959,40.174517124655296],[-74.72232664386269,40.16073512188688],[-74.72204964307696,40.15031911987713],[-74.71387464010259,40.1526611206345],[-74.71292164056436,40.156103121614],[-74.70627063858713,40.16180112274879],[-74.70842463995645,40.17185412476296],[-74.7126716416723,40.17441612510306],[-74.70828064029463,40.18191212737372],[-74.6962306362561,40.18276412749339],[-74.6905686343913,40.17688812696207],[-74.6844876328261,40.17796212744656],[-74.67562462934963,40.17267612662666],[-74.67675162911556,40.168528125067155],[-74.66970162719824,40.165238125111564],[-74.66202462469153,40.16493812537479],[-74.6614866242973,40.16220212483173],[-74.65198762127439,40.15898012448182],[-74.64885561977843,40.155794123743874],[-74.6385196170822,40.154364123614194],[-74.63799961661698,40.151897123624906],[-74.63022761310447,40.148829123240404],[-74.62316161119104,40.14864612379188],[-74.62338361156188,40.14271912183471],[-74.60330460476789,40.13863212211801],[-74.60242060439204,40.13698412191526],[-74.5878365995023,40.13826212303293],[-74.60402960640529,40.165428127324326],[-74.60929560827101,40.172019128515004],[-74.614577610273,40.18239113050463],[-74.59963660637793,40.18679913163061],[-74.5970936051282,40.18615013212174],[-74.5936766040533,40.17942913027156],[-74.58606160208139,40.184064131431775],[-74.5742935983779,40.187050132681094],[-74.57124259747604,40.18530113297325],[-74.56259259398442,40.189951133952704],[-74.5574115929312,40.199424135736244],[-74.54860159124449,40.2076931373882],[-74.54326958980442,40.21670013949693],[-74.48147757182058,40.242898147547876],[-74.48566057320403,40.248828148209064],[-74.48496357336015,40.25333314887041]]]},properties:{geoid:”34021″,name:”Mercer”,state_name:”New Jersey”,county_state_name:”Mercer County, New Jersey”,”27_22k_diff”:66.18,”40_22k_diff”:66.18,”60_22k_diff”:66.19,”27_35k_diff”:131.83,”40_35k_diff”:131.84,”60_35k_diff”:131.83,”27_65k_diff”:0,”40_65k_diff”:84.32,”60_65k_diff”:696.41,”27_95k_diff”:0,”40_95k_diff”:0,”60_95k_diff”:483.91,”27_22k_eptc”:0,”40_22k_eptc”:0,”60_22k_eptc”:0,”27_35k_eptc”:86.04,”40_35k_eptc”:86.04,”60_35k_eptc”:86.05,”27_65k_eptc”:446.7,”40_65k_eptc”:460.42,”60_65k_eptc”:460.42,”27_95k_eptc”:446.7,”40_95k_eptc”:544.74,”60_95k_eptc”:672.92,”27_22k_no_eptc”:66.18,”40_22k_no_eptc”:66.18,”60_22k_no_eptc”:66.19,”27_35k_no_eptc”:217.87,”40_35k_no_eptc”:217.88,”60_35k_no_eptc”:217.88,”27_65k_no_eptc”:446.7,”40_65k_no_eptc”:544.74,”60_65k_no_eptc”:1156.83,”27_95k_no_eptc”:446.7,”40_95k_no_eptc”:544.74,”60_95k_no_eptc”:1156.83}}]}});var _4=”http://www.w3.org/1999/xhtml”,G4={svg:”http://www.w3.org/2000/svg”,xhtml:_4,xlink:”http://www.w3.org/1999/xlink”,xml:”http://www.w3.org/XML/1998/namespace”,xmlns:”http://www.w3.org/2000/xmlns/”};function X(t){var e=t+=””,_=e.indexOf(“:”);return _>=0&&(e=t.slice(0,_))!==”xmlns”&&(t=t.slice(_+1)),G4.hasOwnProperty(e)?{space:G4[e],local:t}:t}function T5(t){return function(){var e=this.ownerDocument,_=this.namespaceURI;return _===_4&&e.documentElement.namespaceURI===_4?e.createElement(t):e.createElementNS(_,t)}}function L5(t){return function(){return this.ownerDocument.createElementNS(t.space,t.local)}}function n4(t){var e=X(t);return(e.local?L5:T5)(e)}function $5(){}function f7(t){return t==null?$5:function(){return this.querySelector(t)}}function G0(t){typeof t!=”function”&&(t=f7(t));for(var e=this._groups,_=e.length,n=new Array(_),o=0;o<_;++o)for(var r=e[o],i=r.length,f=n[o]=new Array(i),c,p,k=0;k<i;++k)(c=r[k])&&(p=t.call(c,c.__data__,k,r))&&("__data__"in c&&(p.__data__=c.__data__),f[k]=p);return new x(n,this._parents)}function I5(){return[]}function E7(t){return t==null?I5:function(){return this.querySelectorAll(t)}}function U0(t){typeof t!="function"&&(t=E7(t));for(var e=this._groups,_=e.length,n=[],o=[],r=0;r<_;++r)for(var i=e[r],f=i.length,c,p=0;p<f;++p)(c=i[p])&&(n.push(t.call(c,c.__data__,p,i)),o.push(c));return new x(n,o)}function F7(t){return function(){return this.matches(t)}}function K0(t){typeof t!="function"&&(t=F7(t));for(var e=this._groups,_=e.length,n=new Array(_),o=0;o<_;++o)for(var r=e[o],i=r.length,f=n[o]=[],c,p=0;p<i;++p)(c=r[p])&&t.call(c,c.__data__,p,r)&&f.push(c);return new x(n,this._parents)}function o4(t){return new Array(t.length)}function Q0(){return new x(this._enter||this._groups.map(o4),this._parents)}function T7(t,e){this.ownerDocument=t.ownerDocument,this.namespaceURI=t.namespaceURI,this._next=null,this._parent=t,this.__data__=e}T7.prototype={constructor:T7,appendChild:function(t){return this._parent.insertBefore(t,this._next)},insertBefore:function(t,e){return this._parent.insertBefore(t,e)},querySelector:function(t){return this._parent.querySelector(t)},querySelectorAll:function(t){return this._parent.querySelectorAll(t)}};function Z0(t){return function(){return t}}var j0="$";function q5(t,e,_,n,o,r){for(var i=0,f,c=e.length,p=r.length;i<p;++i)(f=e[i])?(f.__data__=r[i],n[i]=f):_[i]=new T7(t,r[i]);for(;i<c;++i)(f=e[i])&&(o[i]=f)}function O5(t,e,_,n,o,r,i){var f,c,p={},k=e.length,s=r.length,a=new Array(k),u;for(f=0;f<k;++f)(c=e[f])&&(a[f]=u=j0+i.call(c,c.__data__,f,e),u in p?o[f]=c:p[u]=c);for(f=0;f<s;++f)u=j0+i.call(t,r[f],f,r),(c=p[u])?(n[f]=c,c.__data__=r[f],p[u]=null):_[f]=new T7(t,r[f]);for(f=0;f<k;++f)(c=e[f])&&p[a[f]]===c&&(o[f]=c)}function t1(t,e){if(!t)return u=new Array(this.size()),p=-1,this.each(function(L){u[++p]=L}),u;var _=e?O5:q5,n=this._parents,o=this._groups;typeof t!="function"&&(t=Z0(t));for(var r=o.length,i=new Array(r),f=new Array(r),c=new Array(r),p=0;p<r;++p){var k=n[p],s=o[p],a=s.length,u=t.call(k,k&&k.__data__,p,n),l=u.length,d=f[p]=new Array(l),h=i[p]=new Array(l),b=c[p]=new Array(a);_(k,s,d,h,b,u,e);for(var M=0,C=0,B,g;M=C&&(C=M+1);!(g=h[C])&&++C<l;);B._next=g||null}}return i=new x(i,n),i._enter=f,i._exit=c,i}function e1(){return new x(this._exit||this._groups.map(o4),this._parents)}function _1(t,e,_){var n=this.enter(),o=this,r=this.exit();return n=typeof t=="function"?t(n):n.append(t+""),e!=null&&(o=e(o)),_==null?r.remove():_(r),n&&o?n.merge(o).order():o}function n1(t){for(var e=this._groups,_=t._groups,n=e.length,o=_.length,r=Math.min(n,o),i=new Array(n),f=0;f<r;++f)for(var c=e[f],p=_[f],k=c.length,s=i[f]=new Array(k),a,u=0;u<k;++u)(a=c[u]||p[u])&&(s[u]=a);for(;f<n;++f)i[f]=e[f];return new x(i,this._parents)}function o1(){for(var t=this._groups,e=-1,_=t.length;++e=0;)(i=n[o])&&(r&&i.compareDocumentPosition(r)^4&&r.parentNode.insertBefore(i,r),r=i);return this}function r1(t){t||(t=D5);function e(s,a){return s&&a?t(s.__data__,a.__data__):!s-!a}for(var _=this._groups,n=_.length,o=new Array(n),r=0;r<n;++r){for(var i=_[r],f=i.length,c=o[r]=new Array(f),p,k=0;k<f;++k)(p=i[k])&&(c[k]=p);c.sort(e)}return new x(o,this._parents).order()}function D5(t,e){return te?1:t>=e?0:NaN}function i1(){var t=arguments[0];return arguments[0]=this,t.apply(null,arguments),this}function f1(){var t=new Array(this.size()),e=-1;return this.each(function(){t[++e]=this}),t}function c1(){for(var t=this._groups,e=0,_=t.length;e<_;++e)for(var n=t[e],o=0,r=n.length;o<r;++o){var i=n[o];if(i)return i}return null}function a1(){var t=0;return this.each(function(){++t}),t}function p1(){return!this.node()}function k1(t){for(var e=this._groups,_=0,n=e.length;_<n;++_)for(var o=e[_],r=0,i=o.length,f;r<i;++r)(f=o[r])&&t.call(f,f.__data__,r,o);return this}function R5(t){return function(){this.removeAttribute(t)}}function B5(t){return function(){this.removeAttributeNS(t.space,t.local)}}function H5(t,e){return function(){this.setAttribute(t,e)}}function z5(t,e){return function(){this.setAttributeNS(t.space,t.local,e)}}function J5(t,e){return function(){var _=e.apply(this,arguments);_==null?this.removeAttribute(t):this.setAttribute(t,_)}}function V5(t,e){return function(){var _=e.apply(this,arguments);_==null?this.removeAttributeNS(t.space,t.local):this.setAttributeNS(t.space,t.local,_)}}function s1(t,e){var _=X(t);if(arguments.length1?this.each((e==null?W5:typeof e==”function”?X5:Y5)(t,e,_??””)):K(this.node(),t)}function K(t,e){return t.style.getPropertyValue(e)||r4(t).getComputedStyle(t,null).getPropertyValue(e)}function G5(t){return function(){delete this[t]}}function U5(t,e){return function(){this[t]=e}}function K5(t,e){return function(){var _=e.apply(this,arguments);_==null?delete this[t]:this[t]=_}}function l1(t,e){return arguments.length>1?this.each((e==null?G5:typeof e==”function”?K5:U5)(t,e)):this.node()[t]}function d1(t){return t.trim().split(/^|s+/)}function U4(t){return t.classList||new m1(t)}function m1(t){this._node=t,this._names=d1(t.getAttribute(“class”)||””)}m1.prototype={add:function(t){var e=this._names.indexOf(t);e=0&&(this._names.splice(e,1),this._node.setAttribute(“class”,this._names.join(” “)))},contains:function(t){return this._names.indexOf(t)>=0}};function h1(t,e){for(var _=U4(t),n=-1,o=e.length;++n<o;)_.add(e[n])}function y1(t,e){for(var _=U4(t),n=-1,o=e.length;++n<o;)_.remove(e[n])}function Q5(t){return function(){h1(this,t)}}function Z5(t){return function(){y1(this,t)}}function j5(t,e){return function(){(e.apply(this,arguments)?h1:y1)(this,t)}}function g1(t,e){var _=d1(t+"");if(arguments.length<2){for(var n=U4(this.node()),o=-1,r=_.length;++o<r;)if(!n.contains(_[o]))return!1;return!0}return this.each((typeof e=="function"?j5:e?Q5:Z5)(_,e))}function t6(){this.textContent=""}function e6(t){return function(){this.textContent=t}}function _6(t){return function(){var e=t.apply(this,arguments);this.textContent=e??""}}function x1(t){return arguments.length?this.each(t==null?t6:(typeof t=="function"?_6:e6)(t)):this.node().textContent}function n6(){this.innerHTML=""}function o6(t){return function(){this.innerHTML=t}}function r6(t){return function(){var e=t.apply(this,arguments);this.innerHTML=e??""}}function w1(t){return arguments.length?this.each(t==null?n6:(typeof t=="function"?r6:o6)(t)):this.node().innerHTML}function i6(){this.nextSibling&&this.parentNode.appendChild(this)}function v1(){return this.each(i6)}function f6(){this.previousSibling&&this.parentNode.insertBefore(this,this.parentNode.firstChild)}function P1(){return this.each(f6)}function b1(t){var e=typeof t=="function"?t:n4(t);return this.select(function(){return this.appendChild(e.apply(this,arguments))})}function c6(){return null}function M1(t,e){var _=typeof t=="function"?t:n4(t),n=e==null?c6:typeof e=="function"?e:f7(e);return this.select(function(){return this.insertBefore(_.apply(this,arguments),n.apply(this,arguments)||null)})}function a6(){var t=this.parentNode;t&&t.removeChild(this)}function C1(){return this.each(a6)}function p6(){var t=this.cloneNode(!1),e=this.parentNode;return e?e.insertBefore(t,this.nextSibling):t}function k6(){var t=this.cloneNode(!0),e=this.parentNode;return e?e.insertBefore(t,this.nextSibling):t}function S1(t){return this.select(t?k6:p6)}function N1(t){return arguments.length?this.property("__data__",t):this.node().__data__}var E1={},K4=null;typeof document=0&&(_=e.slice(n+1),e=e.slice(0,n)),{type:e,name:_}})}function l6(t){return function(){var e=this.__on;if(e){for(var _=0,n=-1,o=e.length,r;_<o;++_)r=e[_],(!t.type||r.type===t.type)&&r.name===t.name?this.removeEventListener(r.type,r.listener,r.capture):e[++n]=r;++n?e.length=n:delete this.__on}}}function d6(t,e,_){var n=E1.hasOwnProperty(t.type)?s6:F1;return function(o,r,i){var f=this.__on,c,p=n(e,r,i);if(f){for(var k=0,s=f.length;k<s;++k)if((c=f[k]).type===t.type&&c.name===t.name){this.removeEventListener(c.type,c.listener,c.capture),this.addEventListener(c.type,c.listener=p,c.capture=_),c.value=e;return}}this.addEventListener(t.type,p,_),c={type:t.type,name:t.name,value:e,listener:p,capture:_},f?f.push(c):this.__on=[c]}}function T1(t,e,_){var n=u6(t+""),o,r=n.length,i;if(arguments.length<2){var f=this.node().__on;if(f){for(var c=0,p=f.length,k;c<p;++c)for(o=0,k=f[c];o<r;++o)if((i=n[o]).type===k.type&&i.name===k.name)return k.value}return}for(f=e?d6:l6,_==null&&(_=!1),o=0;o<r;++o)this.each(f(n[o],e,_));return this}function L1(t,e,_){var n=r4(t),o=n.CustomEvent;typeof o=="function"?o=new o(e,_):(o=n.document.createEvent("Event"),_?(o.initEvent(e,_.bubbles,_.cancelable),o.detail=_.detail):o.initEvent(e,!1,!1)),t.dispatchEvent(o)}function m6(t,e){return function(){return L1(this,t,e)}}function h6(t,e){return function(){return L1(this,t,e.apply(this,arguments))}}function $1(t,e){return this.each((typeof e=="function"?h6:m6)(t,e))}var Q4=[null];function x(t,e){this._groups=t,this._parents=e}function I1(){return new x([[document.documentElement]],Q4)}x.prototype=I1.prototype={constructor:x,select:G0,selectAll:U0,filter:K0,data:t1,enter:Q0,exit:e1,join:_1,merge:n1,order:o1,sort:r1,call:i1,nodes:f1,node:c1,size:a1,empty:p1,each:k1,attr:s1,style:u1,property:l1,classed:g1,text:x1,html:w1,raise:v1,lower:P1,append:b1,insert:M1,remove:C1,clone:S1,datum:N1,on:T1,dispatch:$1};var G=I1;function i4(t){return typeof t=="string"?new x([[document.querySelector(t)]],[document.documentElement]):new x([[t]],Q4)}function z(t,e){return te?1:t>=e?0:NaN}function f4(t){return t.length===1&&(t=y6(t)),{left:function(e,_,n,o){for(n==null&&(n=0),o==null&&(o=e.length);n>>1;t(e[r],_)<0?n=r+1:o=r}return n},right:function(e,_,n,o){for(n==null&&(n=0),o==null&&(o=e.length);n>>1;t(e[r],_)>0?o=r:n=r+1}return n}}}function y6(t){return function(e,_){return z(t(e),_)}}var q1=f4(z),O1=q1.right,g6=q1.left,Q=O1;var D1=Array.prototype,w6=D1.slice,v6=D1.map;function a4(t,e,_){t=+t,e=+e,_=(o=arguments.length)<2?(e=t,t=0,1):o<3?1:+_;for(var n=-1,o=Math.max(0,Math.ceil((e-t)/_))|0,r=new Array(o);++n0)return[t];if((n=e0)for(t=Math.ceil(t/f),e=Math.floor(e/f),i=new Array(r=Math.ceil(e-t+1));++o<r;)i[o]=(t+o)*f;else for(t=Math.floor(t*f),e=Math.ceil(e*f),i=new Array(r=Math.ceil(t-e+1));++o=0?(r>=Z4?10:r>=j4?5:r>=t0?2:1)*Math.pow(10,o):-Math.pow(10,-o)/(r>=Z4?10:r>=j4?5:r>=t0?2:1)}function L7(t,e,_){var n=Math.abs(e-t)/Math.max(0,_),o=Math.pow(10,Math.floor(Math.log(n)/Math.LN10)),r=n/o;return r>=Z4?o*=10:r>=j4?o*=5:r>=t0&&(o*=2),e<t?-o:o}function k4(t,e){var _=t.length,n=-1,o,r;if(e==null){for(;++n=o)for(r=o;++nr&&(r=o)}else for(;++n=o)for(r=o;++nr&&(r=o);return r}function T(t,e){switch(arguments.length){case 0:break;case 1:this.range(t);break;default:this.range(e).domain(t);break}return this}var $=”$”;function s4(){}s4.prototype=R1.prototype={constructor:s4,has:function(t){return $+t in this},get:function(t){return this[$+t]},set:function(t,e){return this[$+t]=e,this},remove:function(t){var e=$+t;return e in this&&delete this[e]},clear:function(){for(var t in this)t[0]===$&&delete this[t]},keys:function(){var t=[];for(var e in this)e[0]===$&&t.push(e.slice(1));return t},values:function(){var t=[];for(var e in this)e[0]===$&&t.push(this[e]);return t},entries:function(){var t=[];for(var e in this)e[0]===$&&t.push({key:e.slice(1),value:this[e]});return t},size:function(){var t=0;for(var e in this)e[0]===$&&++t;return t},empty:function(){for(var t in this)if(t[0]===$)return!1;return!0},each:function(t){for(var e in this)e[0]===$&&t(this[e],e.slice(1),this)}};function R1(t,e){var _=new s4;if(t instanceof s4)t.each(function(f,c){_.set(c,f)});else if(Array.isArray(t)){var n=-1,o=t.length,r;if(e==null)for(;++n<o;)_.set(n,t[n]);else for(;++n<o;)_.set(e(r=t[n],n,t),r)}else if(t)for(var i in t)_.set(i,t[i]);return _}var c7=R1;function u4(){}var a7=c7.prototype;u4.prototype=N6.prototype={constructor:u4,has:a7.has,add:function(t){return t+="",this[$+t]=t,this},remove:a7.remove,clear:a7.clear,values:a7.keys,size:a7.size,empty:a7.empty,each:a7.each};function N6(t,e){var _=new u4;if(t instanceof u4)t.each(function(r){_.add(r)});else if(t){var n=-1,o=t.length;if(e==null)for(;++n<o;)_.add(t[n]);else for(;++n<o;)_.add(e(t[n],n,t))}return _}var B1=Array.prototype,l4=B1.map,Z=B1.slice;var _0={name:"implicit"};function $7(){var t=c7(),e=[],_=[],n=_0;function o(r){var i=r+"",f=t.get(i);if(!f){if(n!==_0)return n;t.set(i,f=e.push(r))}return _[(f-1)%_.length]}return o.domain=function(r){if(!arguments.length)return e.slice();e=[],t=c7();for(var i=-1,f=r.length,c,p;++i<f;)t.has(p=(c=r[i])+"")||t.set(p,e.push(c));return o},o.range=function(r){return arguments.length?(_=Z.call(r),o):_.slice()},o.unknown=function(r){return arguments.length?(n=r,o):n},o.copy=function(){return $7(e,_).unknown(n)},T.apply(o,arguments),o}function I7(){var t=$7().unknown(void 0),e=t.domain,_=t.range,n=[0,1],o,r,i=!1,f=0,c=0,p=.5;delete t.unknown;function k(){var s=e().length,a=n[1]>8&15|e>>4&240,e>>4&15|e&240,(e&15)<>24&255,e>>16&255,e>>8&255,(e&255)/255):_===4?m4(e>>12&15|e>>8&240,e>>8&15|e>>4&240,e>>4&15|e&240,((e&15)<>16&255,t>>8&255,t&255,1)}function m4(t,e,_,n){return n<=0&&(t=e=_=NaN),new I(t,e,_,n)}function O6(t){return t instanceof D7||(t=H(t)),t?(t=t.rgb(),new I(t.r,t.g,t.b,t.opacity)):new I}function x7(t,e,_,n){return arguments.length===1?O6(t):new I(t,e,_,n??1)}function I(t,e,_,n){this.r=+t,this.g=+e,this.b=+_,this.opacity=+n}d4(I,x7,n0(D7,{brighter:function(t){return t=t==null?h4:Math.pow(h4,t),new I(this.r*t,this.g*t,this.b*t,this.opacity)},darker:function(t){return t=t==null?q7:Math.pow(q7,t),new I(this.r*t,this.g*t,this.b*t,this.opacity)},rgb:function(){return this},displayable:function(){return-.5<=this.r&&this.r<255.5&&-.5<=this.g&&this.g<255.5&&-.5<=this.b&&this.b<255.5&&0<=this.opacity&&this.opacity<=1},hex:W1,formatHex:W1,formatRgb:Y1,toString:Y1}));function W1(){return"#"+o0(this.r)+o0(this.g)+o0(this.b)}function Y1(){var t=this.opacity;return t=isNaN(t)?1:Math.max(0,Math.min(1,t)),(t===1?"rgb(":"rgba(")+Math.max(0,Math.min(255,Math.round(this.r)||0))+", "+Math.max(0,Math.min(255,Math.round(this.g)||0))+", "+Math.max(0,Math.min(255,Math.round(this.b)||0))+(t===1?")":", "+t+")")}function o0(t){return t=Math.max(0,Math.min(255,Math.round(t)||0)),(t<16?"0":"")+t.toString(16)}function X1(t,e,_,n){return n<=0?t=e=_=NaN:_=1?t=e=NaN:e<=0&&(t=NaN),new J(t,e,_,n)}function G1(t){if(t instanceof J)return new J(t.h,t.s,t.l,t.opacity);if(t instanceof D7||(t=H(t)),!t)return new J;if(t instanceof J)return t;t=t.rgb();var e=t.r/255,_=t.g/255,n=t.b/255,o=Math.min(e,_,n),r=Math.max(e,_,n),i=NaN,f=r-o,c=(r+o)/2;return f?(e===r?i=(_-n)/f+(_<n)*6:_===r?i=(n-e)/f+2:i=(e-_)/f+4,f/=c0&&c<1?0:i,new J(i,f,c,t.opacity)}function U1(t,e,_,n){return arguments.length===1?G1(t):new J(t,e,_,n??1)}function J(t,e,_,n){this.h=+t,this.s=+e,this.l=+_,this.opacity=+n}d4(J,U1,n0(D7,{brighter:function(t){return t=t==null?h4:Math.pow(h4,t),new J(this.h,this.s,this.l*t,this.opacity)},darker:function(t){return t=t==null?q7:Math.pow(q7,t),new J(this.h,this.s,this.l*t,this.opacity)},rgb:function(){var t=this.h%360+(this.h<0)*360,e=isNaN(t)||isNaN(this.s)?0:this.s,_=this.l,n=_+(_=240?t-240:t+120,o,n),r0(t,o,n),r0(t<120?t+240:t-120,o,n),this.opacity)},displayable:function(){return(0<=this.s&&this.s<=1||isNaN(this.s))&&0<=this.l&&this.l<=1&&0<=this.opacity&&this.opacity<=1},formatHsl:function(){var t=this.opacity;return t=isNaN(t)?1:Math.max(0,Math.min(1,t)),(t===1?"hsl(":"hsla(")+(this.h||0)+", "+(this.s||0)*100+"%, "+(this.l||0)*100+"%"+(t===1?")":", "+t+")")}}));function r0(t,e,_){return(t<60?e+(_-e)*t/60:t<180?_:t<240?e+(_-e)*(240-t)/60:e)*255}function i0(t,e,_,n,o){var r=t*t,i=r*t;return((1-3*t+3*r-i)*e+(4-6*r+3*i)*_+(1+3*t+3*r-3*i)*n+i*o)/6}function K1(t){var e=t.length-1;return function(_){var n=_=1?(_=1,e-1):Math.floor(_*e),o=t[n],r=t[n+1],i=n>0?t[n-1]:2*o-r,f=n<e-1?t[n+2]:2*r-o;return i0((_-n/e)*e,i,o,r,f)}}function Q1(t){var e=t.length;return function(_){var n=Math.floor(((_%=1)<0?++_:_)*e),o=t[(n+e-1)%e],r=t[n%e],i=t[(n+1)%e],f=t[(n+2)%e];return i0((_-n/e)*e,o,r,i,f)}}function R7(t){return function(){return t}}function D6(t,e){return function(_){return t+_*e}}function R6(t,e,_){return t=Math.pow(t,_),e=Math.pow(e,_)-t,_=1/_,function(n){return Math.pow(t+n*e,_)}}function Z1(t){return(t=+t)==1?y4:function(e,_){return _-e?R6(e,_,t):R7(isNaN(e)?_:e)}}function y4(t,e){var _=e-t;return _?D6(t,_):R7(isNaN(t)?e:t)}var p7=function t(e){var _=Z1(e);function n(o,r){var i=_((o=x7(o)).r,(r=x7(r)).r),f=_(o.g,r.g),c=_(o.b,r.b),p=y4(o.opacity,r.opacity);return function(k){return o.r=i(k),o.g=f(k),o.b=c(k),o.opacity=p(k),o+""}}return n.gamma=t,n}(1);function j1(t){return function(e){var _=e.length,n=new Array(_),o=new Array(_),r=new Array(_),i,f;for(i=0;i<_;++i)f=x7(e[i]),n[i]=f.r||0,o[i]=f.g||0,r[i]=f.b||0;return n=t(n),o=t(o),r=t(r),f.opacity=1,function(c){return f.r=n(c),f.g=o(c),f.b=r(c),f+""}}}var B6=j1(K1),H6=j1(Q1);function t9(t,e){e||(e=[]);var _=t?Math.min(e.length,t.length):0,n=e.slice(),o;return function(r){for(o=0;o<_;++o)n[o]=t[o]*(1-r)+e[o]*r;return n}}function e9(t){return ArrayBuffer.isView(t)&&!(t instanceof DataView)}function _9(t,e){var _=e?e.length:0,n=t?Math.min(_,t.length):0,o=new Array(n),r=new Array(_),i;for(i=0;i<n;++i)o[i]=k7(t[i],e[i]);for(;i<_;++i)r[i]=e[i];return function(f){for(i=0;i_&&(r=e.slice(_,r),f[i]?f[i]+=r:f[++i]=r),(n=n[0])===(o=o[0])?f[i]?f[i]+=o:f[++i]=o:(f[++i]=null,c.push({i,x:S(n,o)})),_=f0.lastIndex;return _<e.length&&(r=e.slice(_),f[i]?f[i]+=r:f[++i]=r),f.length<2?c[0]?J6(c[0].x):z6(e):(e=c.length,function(p){for(var k=0,s;k<e;++k)f[(s=c[k]).i]=s.x(p);return f.join("")})}function k7(t,e){var _=typeof e,n;return e==null||_==="boolean"?R7(e):(_==="number"?S:_==="string"?(n=H(e))?(e=n,p7):B7:e instanceof H?p7:e instanceof Date?n9:e9(e)?t9:Array.isArray(e)?_9:typeof e.valueOf!="function"&&typeof e.toString!="function"||isNaN(e)?o9:S)(t,e)}function a0(t,e){return t=+t,e=+e,function(_){return Math.round(t*(1-_)+e*_)}}var r9=180/Math.PI,g4={translateX:0,translateY:0,rotate:0,skewX:0,scaleX:1,scaleY:1};function p0(t,e,_,n,o,r){var i,f,c;return(i=Math.sqrt(t*t+e*e))&&(t/=i,e/=i),(c=t*_+e*n)&&(_-=t*c,n-=e*c),(f=Math.sqrt(_*_+n*n))&&(_/=f,n/=f,c/=f),t*n180?k+=360:k-p>180&&(p+=360),a.push({i:s.push(o(s)+”rotate(“,null,n)-2,x:S(p,k)})):k&&s.push(o(s)+”rotate(“+k+n)}function f(p,k,s,a){p!==k?a.push({i:s.push(o(s)+”skewX(“,null,n)-2,x:S(p,k)}):k&&s.push(o(s)+”skewX(“+k+n)}function c(p,k,s,a,u,l){if(p!==s||k!==a){var d=u.push(o(u)+”scale(“,null,”,”,null,”)”);l.push({i:d-4,x:S(p,s)},{i:d-2,x:S(k,a)})}else(s!==1||a!==1)&&u.push(o(u)+”scale(“+s+”,”+a+”)”)}return function(p,k){var s=[],a=[];return p=t(p),k=t(k),r(p.translateX,p.translateY,k.translateX,k.translateY,s,a),i(p.rotate,k.rotate,s,a),f(p.skewX,k.skewX,s,a),c(p.scaleX,p.scaleY,k.scaleX,k.scaleY,s,a),p=k=null,function(u){for(var l=-1,d=a.length,h;++l_&&(n=e,e=_,_=n),function(o){return Math.max(e,Math.min(_,o))}}function V6(t,e,_){var n=t[0],o=t[1],r=e[0],i=e[1];return o<n?(n=d0(o,n),r=_(i,r)):(n=d0(n,o),r=_(r,i)),function(f){return r(n(f))}}function W6(t,e,_){var n=Math.min(t.length,e.length)-1,o=new Array(n),r=new Array(n),i=-1;for(t[n]<t[0]&&(t=t.slice().reverse(),e=e.slice().reverse());++i2?W6:V6,c=p=null,s}function s(a){return isNaN(a=+a)?r:(c||(c=f(t.map(n),e,_)))(n(i(a)))}return s.invert=function(a){return i(o((p||(p=f(e,t.map(n),S)))(a)))},s.domain=function(a){return arguments.length?(t=l4.call(a,l0),i===R||(i=s9(t)),k()):t.slice()},s.range=function(a){return arguments.length?(e=Z.call(a),k()):e.slice()},s.rangeRound=function(a){return e=Z.call(a),_=a0,k()},s.clamp=function(a){return arguments.length?(i=a?s9(t):R,s):i!==R},s.interpolate=function(a){return arguments.length?(_=a,k()):_},s.unknown=function(a){return arguments.length?(r=a,s):r},function(a,u){return n=a,o=u,k()}}function v4(t,e){return w4()(t,e)}function u9(t){return Math.abs(t=Math.round(t))>=1e21?t.toLocaleString(“en”).replace(/,/g,””):t.toString(10)}function s7(t,e){if((_=(t=e?t.toExponential(e-1):t.toExponential()).indexOf(“e”))1?n[0]+n.slice(2):n,+t.slice(_+1)]}function W(t){return t=s7(Math.abs(t)),t?t[1]:NaN}function l9(t,e){return function(_,n){for(var o=_.length,r=[],i=0,f=t[0],c=0;o>0&&f>0&&(c+f+1>n&&(f=Math.max(1,n-c)),r.push(_.substring(o-=f,o+f)),!((c+=f+1)>n));)f=t[i=(i+1)%t.length];return r.reverse().join(e)}}function d9(t){return function(e){return e.replace(/[0-9]/g,function(_){return t[+_]})}}var Y6=/^(?:(.)?([=^]))?([+-( ])?([$#])?(0)?(d+)?(,)?(.d+)?(~)?([a-z%])?$/i;function j(t){if(!(e=Y6.exec(t)))throw new Error(“invalid format: “+t);var e;return new P4({fill:e[1],align:e[2],sign:e[3],symbol:e[4],zero:e[5],width:e[6],comma:e[7],precision:e[8]&&e[8].slice(1),trim:e[9],type:e[10]})}j.prototype=P4.prototype;function P4(t){this.fill=t.fill===void 0?” “:t.fill+””,this.align=t.align===void 0?”>”:t.align+””,this.sign=t.sign===void 0?”-“:t.sign+””,this.symbol=t.symbol===void 0?””:t.symbol+””,this.zero=!!t.zero,this.width=t.width===void 0?void 0:+t.width,this.comma=!!t.comma,this.precision=t.precision===void 0?void 0:+t.precision,this.trim=!!t.trim,this.type=t.type===void 0?””:t.type+””}P4.prototype.toString=function(){return this.fill+this.align+this.sign+this.symbol+(this.zero?”0″:””)+(this.width===void 0?””:Math.max(1,this.width|0))+(this.comma?”,”:””)+(this.precision===void 0?””:”.”+Math.max(0,this.precision|0))+(this.trim?”~”:””)+this.type};function m9(t){t:for(var e=t.length,_=1,n=-1,o;_0&&(n=0);break}return n>0?t.slice(0,n)+t.slice(o+1):t}var m0;function h9(t,e){var _=s7(t,e);if(!_)return t+””;var n=_[0],o=_[1],r=o-(m0=Math.max(-8,Math.min(8,Math.floor(o/3)))*3)+1,i=n.length;return r===i?n:r>i?n+new Array(r-i+1).join(“0″):r>0?n.slice(0,r)+”.”+n.slice(r):”0.”+new Array(1-r).join(“0″)+s7(t,Math.max(0,e+r-1))[0]}function h0(t,e){var _=s7(t,e);if(!_)return t+””;var n=_[0],o=_[1];return oo+1?n.slice(0,o+1)+”.”+n.slice(o+1):n+new Array(o-n.length+2).join(“0”)}var y0={“%”:function(t,e){return(t*100).toFixed(e)},b:function(t){return Math.round(t).toString(2)},c:function(t){return t+””},d:u9,e:function(t,e){return t.toExponential(e)},f:function(t,e){return t.toFixed(e)},g:function(t,e){return t.toPrecision(e)},o:function(t){return Math.round(t).toString(8)},p:function(t,e){return h0(t*100,e)},r:h0,s:h9,X:function(t){return Math.round(t).toString(16).toUpperCase()},x:function(t){return Math.round(t).toString(16)}};function g0(t){return t}var y9=Array.prototype.map,g9=[“y”,”z”,”a”,”f”,”p”,”n”,”xB5″,”m”,””,”k”,”M”,”G”,”T”,”P”,”E”,”Z”,”Y”];function x9(t){var e=t.grouping===void 0||t.thousands===void 0?g0:l9(y9.call(t.grouping,Number),t.thousands+””),_=t.currency===void 0?””:t.currency[0]+””,n=t.currency===void 0?””:t.currency[1]+””,o=t.decimal===void 0?”.”:t.decimal+””,r=t.numerals===void 0?g0:d9(y9.call(t.numerals,String)),i=t.percent===void 0?”%”:t.percent+””,f=t.minus===void 0?”-“:t.minus+””,c=t.nan===void 0?”NaN”:t.nan+””;function p(s){s=j(s);var a=s.fill,u=s.align,l=s.sign,d=s.symbol,h=s.zero,b=s.width,M=s.comma,C=s.precision,B=s.trim,g=s.type;g===”n”?(M=!0,g=”g”):y0[g]||(C===void 0&&(C=12),B=!0,g=”g”),(h||a===”0″&&u===”=”)&&(h=!0,a=”0″,u=”=”);var L=d===”$”?_:d===”#”&&/[boxX]/.test(g)?”0″+g.toLowerCase():””,A7=d===”$”?n:/[%p]/.test(g)?i:””,r7=y0[g],i7=/[defgprs%]/.test(g);C=C===void 0?6:/[gprs]/.test(g)?Math.max(1,Math.min(21,C)):Math.max(0,Math.min(20,C));function U(m){var O=L,D=A7,h7,Y0,j7;if(g===”c”)D=r7(m)+D,m=””;else{m=+m;var t4=m<0||1/m<0;if(m=isNaN(m)?c:r7(Math.abs(m),C),B&&(m=m9(m)),t4&&+m==0&&l!=="+"&&(t4=!1),O=(t4?l==="("?l:f:l==="-"||l==="("?"":l)+O,D=(g==="s"?g9[8+m0/3]:"")+D+(t4&&l==="("?")":""),i7){for(h7=-1,Y0=m.length;++h7j7||j7>57){D=(j7===46?o+m.slice(h7+1):m.slice(h7))+D,m=m.slice(0,h7);break}}}M&&!h&&(m=e(m,1/0));var e4=O.length+m.length+D.length,Y=e4<b?new Array(b-e4+1).join(a):"";switch(M&&h&&(m=e(Y+m,Y.length?b-D.length:1/0),Y=""),u){case">1)+O+m+D+Y.slice(e4);break;default:m=Y+O+m+D;break}return r(m)}return U.toString=function(){return s+””},U}function k(s,a){var u=p((s=j(s),s.type=”f”,s)),l=Math.max(-8,Math.min(8,Math.floor(W(a)/3)))*3,d=Math.pow(10,-l),h=g9[8+l/3];return function(b){return u(d*b)+h}}return{format:p,formatPrefix:k}}var b4,M4,C4;x0({decimal:”.”,thousands:”,”,grouping:[3],currency:[“$”,””],minus:”-“});function x0(t){return b4=x9(t),M4=b4.format,C4=b4.formatPrefix,b4}function w0(t){return Math.max(0,-W(Math.abs(t)))}function v0(t,e){return Math.max(0,Math.max(-8,Math.min(8,Math.floor(W(e)/3)))*3-W(Math.abs(t)))}function P0(t,e){return t=Math.abs(t),e=Math.abs(e)-t,Math.max(0,W(e)-W(t))+1}function b0(t,e,_,n){var o=L7(t,e,_),r;switch(n=j(n??”,f”),n.type){case”s”:{var i=Math.max(Math.abs(t),Math.abs(e));return n.precision==null&&!isNaN(r=v0(o,i))&&(n.precision=r),C4(n,i)}case””:case”e”:case”g”:case”p”:case”r”:{n.precision==null&&!isNaN(r=P0(o,Math.max(Math.abs(t),Math.abs(e))))&&(n.precision=r-(n.type===”e”));break}case”f”:case”%”:{n.precision==null&&!isNaN(r=w0(o))&&(n.precision=r-(n.type===”%”)*2);break}}return M4(n)}function u7(t){var e=t.domain;return t.ticks=function(_){var n=e();return p4(n[0],n[n.length-1],_??10)},t.tickFormat=function(_,n){var o=e();return b0(o[0],o[o.length-1],_??10,n)},t.nice=function(_){_==null&&(_=10);var n=e(),o=0,r=n.length-1,i=n[o],f=n[r],c;return f0?(i=Math.floor(i/c)*c,f=Math.ceil(f/c)*c,c=y7(i,f,_)):c0?(n[o]=Math.floor(i/c)*c,n[r]=Math.ceil(f/c)*c,e(n)):c<0&&(n[o]=Math.ceil(i*c)/c,n[r]=Math.floor(f*c)/c,e(n)),t},t}function v7(){var t=v4(R,R);return t.copy=function(){return w7(t,v7())},T.apply(t,arguments),u7(t)}var G6=1e3,U6=G6*60,K6=U6*60,M0=K6*24,Dr=M0*7,Rr=M0*30,Br=M0*365;var S4=Array.prototype.slice;function v9(t){return t}var C0=1,S0=2,N0=3,z7=4,P9=1e-6;function t2(t){return"translate("+(t+.5)+",0)"}function e2(t){return"translate(0,"+(t+.5)+")"}function _2(t){return function(e){return+t(e)}}function n2(t){var e=Math.max(0,t.bandwidth()-1)/2;return t.round()&&(e=Math.round(e)),function(_){return+t(_)+e}}function o2(){return!this.__axis}function b9(t,e){var _=[],n=null,o=null,r=6,i=6,f=3,c=t===C0||t===z7?-1:1,p=t===z7||t===S0?"x":"y",k=t===C0||t===N0?t2:e2;function s(a){var u=n??(e.ticks?e.ticks.apply(e,_):e.domain()),l=o??(e.tickFormat?e.tickFormat.apply(e,_):v9),d=Math.max(r,0)+f,h=e.range(),b=+h[0]+.5,M=+h[h.length-1]+.5,C=(e.bandwidth?n2:_2)(e.copy()),B=a.selection?a.selection():a,g=B.selectAll(".domain").data([null]),L=B.selectAll(".tick").data(u,e).order(),A7=L.exit(),r7=L.enter().append("g").attr("class","tick"),i7=L.select("line"),U=L.select("text");g=g.merge(g.enter().insert("path",".tick").attr("class","domain").attr("stroke","currentColor")),L=L.merge(r7),i7=i7.merge(r7.append("line").attr("stroke","currentColor").attr(p+"2",c*r)),U=U.merge(r7.append("text").attr("fill","currentColor").attr(p,c*d).attr("dy",t===C0?"0em":t===N0?"0.71em":"0.32em")),a!==B&&(g=g.transition(a),L=L.transition(a),i7=i7.transition(a),U=U.transition(a),A7=A7.transition(a).attr("opacity",P9).attr("transform",function(m){return isFinite(m=C(m))?k(m):this.getAttribute("transform")}),r7.attr("opacity",P9).attr("transform",function(m){var O=this.parentNode.__axis;return k(O&&isFinite(O=O(m))?O:C(m))})),A7.remove(),g.attr("d",t===z7||t==S0?i?"M"+c*i+","+b+"H0.5V"+M+"H"+c*i:"M0.5,"+b+"V"+M:i?"M"+b+","+c*i+"V0.5H"+M+"V"+c*i:"M"+b+",0.5H"+M),L.attr("opacity",1).attr("transform",function(m){return k(C(m))}),i7.attr(p+"2",c*r),U.attr(p,c*d).text(l),B.filter(o2).attr("fill","none").attr("font-size",10).attr("font-family","sans-serif").attr("text-anchor",t===S0?"start":t===z7?"end":"middle"),B.each(function(){this.__axis=C})}return s.scale=function(a){return arguments.length?(e=a,s):e},s.ticks=function(){return _=S4.call(arguments),s},s.tickArguments=function(a){return arguments.length?(_=a==null?[]:S4.call(a),s):_.slice()},s.tickValues=function(a){return arguments.length?(n=a==null?null:S4.call(a),s):n&&n.slice()},s.tickFormat=function(a){return arguments.length?(o=a,s):o},s.tickSize=function(a){return arguments.length?(r=i=+a,s):r},s.tickSizeInner=function(a){return arguments.length?(r=+a,s):r},s.tickSizeOuter=function(a){return arguments.length?(i=+a,s):i},s.tickPadding=function(a){return arguments.length?(f=+a,s):f},s}function N4(t){return b9(N0,t)}function A0(t){return b9(z7,t)}var r2={value:function(){}};function C9(){for(var t=0,e=arguments.length,_={},n;t=0&&(n=_.slice(o+1),_=_.slice(0,o)),_&&!e.hasOwnProperty(_))throw new Error(“unknown type: “+_);return{type:_,name:n}})}A4.prototype=C9.prototype={constructor:A4,on:function(t,e){var _=this._,n=i2(t+””,_),o,r=-1,i=n.length;if(arguments.length<2){for(;++r<i;)if((o=(t=n[r]).type)&&(o=f2(_[o],t.name)))return o;return}if(e!=null&&typeof e!="function")throw new Error("invalid callback: "+e);for(;++r0)for(var _=new Array(o),n=0,o,r;n<o;++n)_[n]=arguments[n+2];if(!this._.hasOwnProperty(t))throw new Error("unknown type: "+t);for(r=this._[t],n=0,o=r.length;n<o;++n)r[n].value.apply(e,_)},apply:function(t,e,_){if(!this._.hasOwnProperty(t))throw new Error("unknown type: "+t);for(var n=this._[t],o=0,r=n.length;o<r;++o)n[o].value.apply(e,_)}};function f2(t,e){for(var _=0,n=t.length,o;_<n;++_)if((o=t[_]).name===e)return o.value}function M9(t,e,_){for(var n=0,o=t.length;n=0&&t._call.call(null,e),t=t._next;–P7}function S9(){l7=(F4=Y7.now())+T4,P7=V7=0;try{E9()}finally{P7=0,p2(),l7=0}}function a2(){var t=Y7.now(),e=t-F4;e>N9&&(T4-=e,F4=t)}function p2(){for(var t,e=E4,_,n=1/0;e;)e._call?(n>e._time&&(n=e._time),t=e,e=e._next):(_=e._next,e._next=null,e=t?t._next=_:E4=_);W7=t,F0(n)}function F0(t){if(!P7){V7&&(V7=clearTimeout(V7));var e=t-l7;e>24?(tT9)throw new Error(“too late; already scheduled”);return _}function E(t,e){var _=v(t,e);if(_.state>I4)throw new Error(“too late; already running”);return _}function v(t,e){var _=t.__transition;if(!_||!(_=_[e]))throw new Error(“transition not found”);return _}function u2(t,e,_){var n=t.__transition,o;n[e]=_,_.timer=L4(r,0,_.time);function r(p){_.state=T0,_.timer.restart(i,_.delay,_.time),_.delay<=p&&i(p-_.delay)}function i(p){var k,s,a,u;if(_.state!==T0)return c();for(k in n)if(u=n[k],u.name===_.name){if(u.state===I4)return $4(i);u.state===F9?(u.state=G7,u.timer.stop(),u.on.call("interrupt",t,t.__data__,u.index,u.group),delete n[k]):+k<e&&(u.state=G7,u.timer.stop(),u.on.call("cancel",t,t.__data__,u.index,u.group),delete n[k])}if($4(function(){_.state===I4&&(_.state=F9,_.timer.restart(f,_.delay,_.time),f(p))}),_.state=q4,_.on.call("start",t,t.__data__,_.index,_.group),_.state===q4){for(_.state=I4,o=new Array(a=_.tween.length),k=0,s=-1;k<a;++k)(u=_.tween[k].value.call(t,t.__data__,_.index,_.group))&&(o[++s]=u);o.length=s+1}}function f(p){for(var k=p<_.duration?_.ease.call(null,p/_.duration):(_.timer.restart(c),_.state=O4,1),s=-1,a=o.length;++sq4&&n.state<O4,n.state=G7,n.timer.stop(),n.on.call(o?"interrupt":"cancel",t,t.__data__,n.index,n.group),delete _[i]}r&&delete t.__transition}}function L9(t){return this.each(function(){L0(this,t)})}function l2(t,e){var _,n;return function(){var o=E(this,t),r=o.tween;if(r!==_){n=_=r;for(var i=0,f=n.length;i<f;++i)if(n[i].name===e){n=n.slice(),n.splice(i,1);break}}o.tween=n}}function d2(t,e,_){var n,o;if(typeof _!="function")throw new Error;return function(){var r=E(this,t),i=r.tween;if(i!==n){o=(n=i).slice();for(var f={name:e,value:_},c=0,p=o.length;c<p;++c)if(o[c].name===e){o[c]=f;break}c===p&&o.push(f)}r.tween=o}}function $9(t,e){var _=this._id;if(t+="",arguments.length<2){for(var n=v(this.node(),_).tween,o=0,r=n.length,i;o<r;++o)if((i=n[o]).name===t)return i.value;return null}return this.each((e==null?l2:d2)(_,t,e))}function M7(t,e,_){var n=t._id;return t.each(function(){var o=E(this,n);(o.value||(o.value={}))[e]=_.apply(this,arguments)}),function(o){return v(o,n).value[e]}}function D4(t,e){var _;return(typeof e=="number"?S:e instanceof H?p7:(_=H(e))?(e=_,p7):B7)(t,e)}function m2(t){return function(){this.removeAttribute(t)}}function h2(t){return function(){this.removeAttributeNS(t.space,t.local)}}function y2(t,e,_){var n,o=_+"",r;return function(){var i=this.getAttribute(t);return i===o?null:i===n?r:r=e(n=i,_)}}function g2(t,e,_){var n,o=_+"",r;return function(){var i=this.getAttributeNS(t.space,t.local);return i===o?null:i===n?r:r=e(n=i,_)}}function x2(t,e,_){var n,o,r;return function(){var i,f=_(this),c;return f==null?void this.removeAttribute(t):(i=this.getAttribute(t),c=f+"",i===c?null:i===n&&c===o?r:(o=c,r=e(n=i,f)))}}function w2(t,e,_){var n,o,r;return function(){var i,f=_(this),c;return f==null?void this.removeAttributeNS(t.space,t.local):(i=this.getAttributeNS(t.space,t.local),c=f+"",i===c?null:i===n&&c===o?r:(o=c,r=e(n=i,f)))}}function I9(t,e){var _=X(t),n=_==="transform"?u0:D4;return this.attrTween(t,typeof e=="function"?(_.local?w2:x2)(_,n,M7(this,"attr."+t,e)):e==null?(_.local?h2:m2)(_):(_.local?g2:y2)(_,n,e))}function v2(t,e){return function(_){this.setAttribute(t,e.call(this,_))}}function P2(t,e){return function(_){this.setAttributeNS(t.space,t.local,e.call(this,_))}}function b2(t,e){var _,n;function o(){var r=e.apply(this,arguments);return r!==n&&(_=(n=r)&&P2(t,r)),_}return o._value=e,o}function M2(t,e){var _,n;function o(){var r=e.apply(this,arguments);return r!==n&&(_=(n=r)&&v2(t,r)),_}return o._value=e,o}function q9(t,e){var _="attr."+t;if(arguments.length<2)return(_=this.tween(_))&&_._value;if(e==null)return this.tween(_,null);if(typeof e!="function")throw new Error;var n=X(t);return this.tween(_,(n.local?b2:M2)(n,e))}function C2(t,e){return function(){U7(this,t).delay=+e.apply(this,arguments)}}function S2(t,e){return e=+e,function(){U7(this,t).delay=e}}function O9(t){var e=this._id;return arguments.length?this.each((typeof t=="function"?C2:S2)(e,t)):v(this.node(),e).delay}function N2(t,e){return function(){E(this,t).duration=+e.apply(this,arguments)}}function A2(t,e){return e=+e,function(){E(this,t).duration=e}}function D9(t){var e=this._id;return arguments.length?this.each((typeof t=="function"?N2:A2)(e,t)):v(this.node(),e).duration}function E2(t,e){if(typeof e!="function")throw new Error;return function(){E(this,t).ease=e}}function R9(t){var e=this._id;return arguments.length?this.each(E2(e,t)):v(this.node(),e).ease}function B9(t){typeof t!="function"&&(t=F7(t));for(var e=this._groups,_=e.length,n=new Array(_),o=0;o<_;++o)for(var r=e[o],i=r.length,f=n[o]=[],c,p=0;p<i;++p)(c=r[p])&&t.call(c,c.__data__,p,r)&&f.push(c);return new N(n,this._parents,this._name,this._id)}function H9(t){if(t._id!==this._id)throw new Error;for(var e=this._groups,_=t._groups,n=e.length,o=_.length,r=Math.min(n,o),i=new Array(n),f=0;f<r;++f)for(var c=e[f],p=_[f],k=c.length,s=i[f]=new Array(k),a,u=0;u<k;++u)(a=c[u]||p[u])&&(s[u]=a);for(;f=0&&(e=e.slice(0,_)),!e||e===”start”})}function T2(t,e,_){var n,o,r=F2(e)?U7:E;return function(){var i=r(this,t),f=i.on;f!==n&&(o=(n=f).copy()).on(e,_),i.on=o}}function z9(t,e){var _=this._id;return arguments.length<2?v(this.node(),_).on.on(t):this.each(T2(_,t,e))}function L2(t){return function(){var e=this.parentNode;for(var _ in this.__transition)if(+_!==t)return;e&&e.removeChild(this)}}function J9(){return this.on("end.remove",L2(this._id))}function V9(t){var e=this._name,_=this._id;typeof t!="function"&&(t=f7(t));for(var n=this._groups,o=n.length,r=new Array(o),i=0;i<o;++i)for(var f=n[i],c=f.length,p=r[i]=new Array(c),k,s,a=0;a<c;++a)(k=f[a])&&(s=t.call(k,k.__data__,a,f))&&("__data__"in k&&(s.__data__=k.__data__),p[a]=s,t7(p[a],e,_,a,p,v(k,_)));return new N(r,this._parents,e,_)}function W9(t){var e=this._name,_=this._id;typeof t!="function"&&(t=E7(t));for(var n=this._groups,o=n.length,r=[],i=[],f=0;f<o;++f)for(var c=n[f],p=c.length,k,s=0;s<p;++s)if(k=c[s]){for(var a=t.call(k,k.__data__,s,c),u,l=v(k,_),d=0,h=a.length;d<h;++d)(u=a[d])&&t7(u,e,_,d,a,l);r.push(a),i.push(k)}return new N(r,i,e,_)}var $2=G.prototype.constructor;function Y9(){return new $2(this._groups,this._parents)}function I2(t,e){var _,n,o;return function(){var r=K(this,t),i=(this.style.removeProperty(t),K(this,t));return r===i?null:r===_&&i===n?o:o=e(_=r,n=i)}}function X9(t){return function(){this.style.removeProperty(t)}}function q2(t,e,_){var n,o=_+"",r;return function(){var i=K(this,t);return i===o?null:i===n?r:r=e(n=i,_)}}function O2(t,e,_){var n,o,r;return function(){var i=K(this,t),f=_(this),c=f+"";return f==null&&(c=f=(this.style.removeProperty(t),K(this,t))),i===c?null:i===n&&c===o?r:(o=c,r=e(n=i,f))}}function D2(t,e){var _,n,o,r="style."+e,i="end."+r,f;return function(){var c=E(this,t),p=c.on,k=c.value[r]==null?f||(f=X9(e)):void 0;(p!==_||o!==k)&&(n=(_=p).copy()).on(i,o=k),c.on=n}}function G9(t,e,_){var n=(t+="")=="transform"?s0:D4;return e==null?this.styleTween(t,I2(t,n)).on("end.style."+t,X9(t)):typeof e=="function"?this.styleTween(t,O2(t,n,M7(this,"style."+t,e))).each(D2(this._id,t)):this.styleTween(t,q2(t,n,e),_).on("end.style."+t,null)}function R2(t,e,_){return function(n){this.style.setProperty(t,e.call(this,n),_)}}function B2(t,e,_){var n,o;function r(){var i=e.apply(this,arguments);return i!==o&&(n=(o=i)&&R2(t,i,_)),n}return r._value=e,r}function U9(t,e,_){var n="style."+(t+="");if(arguments.length<2)return(n=this.tween(n))&&n._value;if(e==null)return this.tween(n,null);if(typeof e!="function")throw new Error;return this.tween(n,B2(t,e,_??""))}function H2(t){return function(){this.textContent=t}}function z2(t){return function(){var e=t(this);this.textContent=e??""}}function K9(t){return this.tween("text",typeof t=="function"?z2(M7(this,"text",t)):H2(t==null?"":t+""))}function J2(t){return function(e){this.textContent=t.call(this,e)}}function V2(t){var e,_;function n(){var o=t.apply(this,arguments);return o!==_&&(e=(_=o)&&J2(o)),e}return n._value=t,n}function Q9(t){var e="text";if(arguments.length<1)return(e=this.tween(e))&&e._value;if(t==null)return this.tween(e,null);if(typeof t!="function")throw new Error;return this.tween(e,V2(t))}function Z9(){for(var t=this._name,e=this._id,_=R4(),n=this._groups,o=n.length,r=0;r<o;++r)for(var i=n[r],f=i.length,c,p=0;p<f;++p)if(c=i[p]){var k=v(c,e);t7(c,t,_,p,i,{time:k.time+k.delay+k.duration,delay:0,duration:k.duration,ease:k.ease})}return new N(n,this._parents,t,_)}function j9(){var t,e,_=this,n=_._id,o=_.size();return new Promise(function(r,i){var f={value:i},c={value:function(){–o===0&&r()}};_.each(function(){var p=E(this,n),k=p.on;k!==t&&(e=(t=k).copy(),e._.cancel.push(f),e._.interrupt.push(f),e._.end.push(c)),p.on=e})})}var W2=0;function N(t,e,_,n){this._groups=t,this._parents=e,this._name=_,this._id=n}function $0(t){return G().transition(t)}function R4(){return++W2}var C7=G.prototype;N.prototype=$0.prototype={constructor:N,select:V9,selectAll:W9,filter:B9,merge:H9,selection:Y9,transition:Z9,call:C7.call,nodes:C7.nodes,node:C7.node,size:C7.size,empty:C7.empty,each:C7.each,on:z9,attr:I9,attrTween:q9,style:G9,styleTween:U9,text:K9,textTween:Q9,remove:J9,tween:$9,delay:O9,duration:D9,ease:R9,end:j9};function B4(t){return((t*=2)<=1?t*t*t:(t-=2)*t*t+2)/2}var I0={time:null,delay:0,duration:250,ease:B4};function Y2(t,e){for(var _;!(_=t.__transition)||!(_=_[e]);)if(!(t=t.parentNode))return I0.time=b7(),I0;return _}function t5(t){var e,_;t instanceof N?(e=t._id,t=t._name):(e=R4(),(_=I0).time=b7(),t=t==null?null:t+"");for(var n=this._groups,o=n.length,r=0;r<o;++r)for(var i=n[r],f=i.length,c,p=0;p{if(t)return t.trim().toLowerCase().normalize(“NFD”).replace(/[u0300-u036f]/g,””).replace(/[^A-Z0-9 ]/gi,””).trim().replace(/ /g,”-“)},K7=(t=null)=>{let e=e5.split(`
`),_={};return e.forEach(n=>{let o=n.trim().match(/^$color-([w-]+):s*([^;]+);/);if(o){let r=o[1],i=o[2];_[r]=i}}),t&&_[t]?_[t]:_};var c5=()=>/Android|webOS|iPhone|iPad|iPod|BlackBerry|IEMobile|Opera Mini/i.test(navigator.userAgent);var q0=(t,e=null,_=null)=>{_||(_=document.querySelector(“head”));let n=document.createElement(“script”);n.type=”text/javascript”,n.src=t,e&&(n.onload=e),_.appendChild(n)},z4=()=>(window.PMNdataLayer?.[0]!==void 0&&window.PMNdataLayer[0])?.analytics?.user?.state===”Subscribed”,J4=()=>{let e=(window.PMNdataLayer?.[0]!==void 0&&window.PMNdataLayer[0])?.analytics?.user?.state;return window.location.host.includes(“zzz-systest”)||window.location.host.includes(“pmn.arcpublishing.com”)||window.location.host.includes(“stage.fusion.inquirer.com”)||typeof e>”u”},a5=()=>{let e=(window.PMNdataLayer?.[0]!==void 0&&window.PMNdataLayer[0])?.analytics?.user?.hasAdsFreeReading;return!!(e&&e==1)},Q7=()=>window.location.host.includes(“localhost”);var p5=(t,e)=>{let _=[…t.querySelectorAll(“[data-populate]”)];t.dataset.populate&&_.unshift(t);let n=_.filter(o=>{let r=o.closest(“[data-populate-context]”);return!r||r==t});for(let o of n){let i=o.dataset.populate.trim().split(/s*,s*/).map(f=>f.split(/s*:s*/));for(let[f,c]of i){let k=f.split(“.”).reduce((u,l)=>u?.[l],e),s=k==null||k==null,a=c?.split(/s+/)||[“innerHTML”];for(let u of a)u.startsWith(“.”)&&o.classList.toggle(u.substring(1),s?!1:k),!s&&(u==”innerHTML”?o.innerHTML=k:u.startsWith(“@”)?o.setAttribute(u.substring(1),k):u.startsWith(“–“)&&o.style.setProperty(u,k))}}};var _3=k5(),n3=”27_35k”,y={top:80,right:40,bottom:80,left:80},V4,o3=document.querySelector(“.js-select-county”).dataset.fips,w,P,A,S7,_7,n7,s5=(t,e=””,_)=>{let n=_3.features.find(p=>p.properties.geoid===t).properties,o=[],r=Object.keys(n),i=new Set;r.forEach(p=>{let k=p.substring(0,p.lastIndexOf(“_”));i.add(k)});let f=Array.isArray(_)?_:_?_.split(“,”).map(p=>p.trim()).filter(Boolean):[];i.forEach(p=>{let k=p+”_eptc”,s=p+”_no_eptc”;n.hasOwnProperty(k)&&n.hasOwnProperty(s)&&o.push({state:n.state_name,county:n.name,county_state_name:n.county_state_name,group:p,yesEPTC:Math.round(n[k]),noEPTC:Math.round(n[s]),diffEPTC:Math.round(n[s]-n[k]),active:f.length===0?!0:f.some(a=>p.includes(a)||a.includes(p))})});let c=e?e.split(“,”).map(p=>p.trim()):[];return c.length>0&&(o=o.filter(p=>c.some(k=>p.group.includes(k)))),o.sort((p,k)=>p.group.localeCompare(k.group)),console.log(o),o},O0=()=>N4(P).ticks(4).tickFormat(t=>`$${t}`),D0=()=>A0(A).tickFormat(t=>{if(t.startsWith(“Age “))return t;let e=t.split(“_”);return e.length>1?`$${e[1]}`:t}),R0=()=>N4(P).ticks(4).tickSize(-(A.range()[1]-40)).tickFormat(“”),r3=t=>{chartEl=document.querySelector(“.js-arrow-chart”),width=chartEl.getBoundingClientRect().width,height=chartEl.getBoundingClientRect().height,w=i4(“.js-arrow-chart-svg”).attr(“viewBox”,`0 0 ${width} ${height}`).attr(“preserveAspectRatio”,”none”).append(“g”).attr(“transform”,`translate(${y.left},${y.top})`),w.append(“text”).attr(“class”,”inno-arrow-chart__title inno-arrow-chart__title–1″).attr(“x”,(width-y.left-y.right)/2).attr(“y”,-35).text(“ACA Premiums Increases in”),w.append(“text”).attr(“class”,”inno-arrow-chart__title inno-arrow-chart__title–2″).attr(“x”,(width-y.left-y.right)/2).attr(“y”,-4),w.append(“text”).attr(“class”,”inno-arrow-chart__axis-title inno-arrow-chart__axis-title–x”).attr(“x”,(width-y.left-y.right)/2).attr(“y”,height-y.top-y.bottom+60).attr(“text-anchor”,”middle”).text(“Estimated Monthly Premium ($)”);let e=k4(t,r=>r.noEPTC);P=v7().domain([0,e*1]).range([0,width-y.left-y.right]);let _=1659;S7=v7().domain([_*.2,_*.6,_]).range([K7(“orange”),K7(“red”),K7(“purple”)]),_7=w.append(“g”).attr(“class”,”inno-arrow-chart__x-axis”).attr(“transform”,`translate(0,${height-y.top-y.bottom})`).call(O0()),_7.selectAll(“line”).attr(“class”,r=>`inno-arrow-chart__x-axis-line inno-arrow-chart__x-axis-line–${q(r+””)}`),_7.selectAll(“text”).attr(“class”,r=>`inno-arrow-chart__x-axis-label inno-arrow-chart__x-axis-label–${q(r+””)}`);let n=[],o=””;t.forEach(r=>{let i=r.group.split(“_”)[0];o!==i&&(n.push(“Age “+i),o=i),n.push(r.group)}),A=I7().range([0,height-y.top-y.bottom]).domain(n).padding(1),n7=w.append(“g”).attr(“class”,”inno-arrow-chart__y-axis”).call(D0()),n7.selectAll(“line”).attr(“class”,r=>`inno-arrow-chart__y-axis-line inno-arrow-chart__y-axis-line–${q(r+””)}`),n7.selectAll(“text”).attr(“class”,r=>`inno-arrow-chart__y-axis-label inno-arrow-chart__y-axis-label–${q(r+””)}`),w.append(“g”).attr(“class”,”inno-arrow-chart__grid-x”).attr(“transform”,`translate(0,${height-y.top-y.bottom})`).call(R0()),u5(t)},u5=t=>{let e=w.select(“.inno-arrow-chart__title–2”),_=+e.attr(“x”),n=+e.attr(“y”);e.text()!=t[0].county_state_name&&e.transition().duration(400).text(`${t[0].county_state_name}`).attr(“transform”,`translate(${_},${n}) scale(1.1) translate(${-_},${-n})`).transition().duration(400).attr(“transform”,`translate(${_},${n}) scale(1) translate(${-_},${-n})`);let o=k4(t,a=>a.noEPTC);P.domain([0,o*1.1]);let r=[],i=””;t.forEach(a=>{let u=a.group.split(“_”)[0];i!==u&&(r.push(“Age “+u),i=u),r.push(a.group)}),A.domain(r),w.select(“.inno-arrow-chart__grid-x”).transition().duration(800).call(R0()),_7.transition().duration(800).call(O0()).selectAll(“line”).attr(“class”,a=>`inno-arrow-chart__x-axis-line inno-arrow-chart__x-axis-line–${q(a+””)}`),_7.selectAll(“text”).attr(“class”,a=>`inno-arrow-chart__x-axis-label inno-arrow-chart__x-axis-label–${q(a+””)}`),n7.transition().duration(800).call(D0()).selectAll(“line”).attr(“class”,a=>`inno-arrow-chart__y-axis-line inno-arrow-chart__y-axis-line–${q(a+””)}`),n7.selectAll(“text”).attr(“class”,a=>`inno-arrow-chart__y-axis-label inno-arrow-chart__y-axis-label–${q(a+””)}`);let f=w.selectAll(“.inno-arrow-chart__arrow”).data(t,a=>a.group);console.log(f),f.exit().remove(),f.enter().append(“path”).attr(“class”,”inno-arrow-chart__arrow”).attr(“opacity”,0).merge(f).transition().duration(800).attr(“d”,a=>{let u=P(a.yesEPTC),l=P(a.noEPTC),d=A(a.group),h=3,b=6,M=6;if(a.diffEPTC>0)return`
M ${u},${d-h/2}
L ${l-b},${d-h/2}
L ${l-b},${d-M}
L ${l},${d}
L ${l-b},${d+M}
L ${l-b},${d+h/2}
L ${u},${d+h/2}
Z`}).attr(“fill”,a=>S7(Math.abs(a.diffEPTC))).style(“opacity”,a=>a.active?1:.3);let c=w.selectAll(“.inno-arrow-chart__label-delta”).data(t,a=>a.group);c.exit().transition().duration(400).style(“opacity”,0).remove(),c.enter().append(“text”).attr(“class”,”inno-arrow-chart__label-delta”).attr(“x”,a=>(P(a.yesEPTC)+P(a.noEPTC))/2).attr(“y”,a=>A(a.group)-12).attr(“dy”,”0.15em”).style(“opacity”,0).merge(c).transition().duration(800).attr(“fill”,a=>Math.abs(a.yesEPTC-a.noEPTC)/a.yesEPTC(P(a.yesEPTC)+P(a.noEPTC))/2).attr(“y”,a=>A(a.group)-12).attr(“fill”,a=>a.active?S7(Math.abs(a.diffEPTC)):”lightgray”).text(a=>a.diffEPTC==0?”No increase”:`+$${Math.round(a.diffEPTC)}`).style(“opacity”,a=>a.active?1:.3);let p=w.selectAll(“.inno-arrow-chart__label-end”).data(t,a=>a.group);p.exit().transition().duration(400).style(“opacity”,0).remove(),p.enter().append(“text”).attr(“class”,”inno-arrow-chart__label-end”).attr(“y”,a=>A(a.group)).attr(“dy”,”0.35em”).style(“opacity”,0).merge(p).transition().duration(800).attr(“x”,a=>P(a.noEPTC)+10).attr(“y”,a=>A(a.group)).text(a=>`$${Math.round(a.noEPTC)}`).style(“opacity”,a=>a.active?1:.3);let k=w.selectAll(“.circle-eptc”).data(t,a=>a.group);k.enter().append(“circle”).attr(“class”,”circle-eptc”).attr(“r”,5).attr(“cx”,a=>P(a.yesEPTC)).attr(“cy”,a=>A(a.group)).style(“fill”,K7(“light-gray”)).merge(k).transition().duration(800).attr(“cx”,a=>P(a.yesEPTC)).attr(“cy”,a=>A(a.group)).style(“opacity”,a=>a.active?a.diffEPTC>0&&a.diffEPTC{let u=Object.keys(a).reduce((l,d)=>{let h=typeof a[d]==”number”?`$${Math.round(a[d]).toLocaleString()}`:null;return{…l,[`${a.group}_${d}`]:h||a[d]}},{});s.forEach(l=>{if(p5(l,{…u,…a}),l.dataset.populate!==”county_state_name”&&!l.dataset.populate.includes(“yes”)&&!l.dataset.populate.includes(“no”)){let d=S7(a.diffEPTC);l.style.color=d,l.style.borderBottom=`solid 2px ${d}`,l.style.fontWeight=”bold”}})})},i3=()=>{let t=document.querySelector(“.js-arrow-chart”),e=t.getBoundingClientRect().width-y.left-y.right,_=t.getBoundingClientRect().height-y.top-y.bottom;i4(“.js-arrow-chart-svg”).attr(“viewBox”,`0 0 ${e+y.left+y.right} ${_+y.top+y.bottom}`),w.select(“.inno-arrow-chart__title–1”).attr(“x”,e/2),w.select(“.inno-arrow-chart__title–2”).attr(“x”,e/2),w.select(“.inno-arrow-chart__axis-title–x”).attr(“x”,e/2).attr(“y”,_+60),P.range([0,e]),A.range([0,_]),_7.attr(“transform”,`translate(0, ${_})`).transition().duration(500).call(O0()),_7.selectAll(“line”).attr(“class”,n=>`inno-arrow-chart__x-axis-line inno-arrow-chart__x-axis-line–${q(n+””)}`),_7.selectAll(“text”).attr(“class”,n=>`inno-arrow-chart__x-axis-label inno-arrow-chart__x-axis-label–${q(n+””)}`),n7.transition().duration(500).call(D0()),n7.selectAll(“line”).attr(“class”,n=>`inno-arrow-chart__y-axis-line inno-arrow-chart__y-axis-line–${q(n+””)}`),n7.selectAll(“text”).attr(“class”,n=>`inno-arrow-chart__y-axis-label inno-arrow-chart__y-axis-label–${q(n+””)}`),w.select(“.inno-arrow-chart__grid-x”).attr(“transform”,`translate(0, ${_})`).transition().duration(500).call(R0()),w.selectAll(“.inno-arrow-chart__line”).transition().duration(500).attr(“x1”,n=>P(n.yesEPTC)).attr(“x2”,n=>P(n.noEPTC)).attr(“y1”,n=>A(n.group)).attr(“y2”,n=>A(n.group)),w.selectAll(“.inno-arrow-chart__label-delta”).transition().duration(500).attr(“x”,n=>P(n.yesEPTC)).attr(“y”,n=>A(n.group)-15).attr(“fill”,n=>n.active?Math.abs(n.diffEPTC)/n.yesEPTC<.01||n.yesEPTCn.diffEPTC==0?”No increase”:`+$${Math.round(n.diffEPTC)}`).style(“opacity”,n=>n.active?n.yesEPTCP(n.noEPTC)+10).text(n=>`$${Math.round(n.noEPTC)}`).attr(“y”,n=>A(n.group))},o7={init:()=>{V4=s5(o3,n3),r3(V4),window.addEventListener(“resize”,i3)},updateChart:(t,e,_)=>{V4=s5(t,e,_),u5(V4)}};var B0=document.querySelectorAll(“.js-select-county”),H0=document.querySelector(“.js-steps–arrow-chart”),Ma=document.querySelector(“.js-spanner–county”),z0,f3=()=>{B0.forEach(t=>{t&&t.addEventListener(“change”,e=>{let _=e.target.options[e.target.selectedIndex],n=_.dataset.fips;n?(z0=_.value,H0.dataset.county=n,B0.forEach(o=>{o.value!==_.value&&(o.value=_.value)}),o7.updateChart(n,H0.dataset.groups)):console.warn(“u26A0uFE0F No FIPS code found on selected option”)})})},c3=()=>{B0.forEach(t=>{if(t){let e=t.dataset.fips;H0.dataset.county=e,z0=t.dataset.county}})},a3=()=>z0,W4={init:()=>{f3(),c3()},getCurrent:()=>a3()};var p3=()=>{a5()&&document.querySelectorAll(“.js-adbox”).forEach(e=>{e.classList.add(“is-hidden”)})},l5={init:()=>{p3()}};var d7,d5,k3=()=>{d7=document.getElementById(“js-inno-toast”)},s3=t=>{if(!d7)return;d7.innerHTML=t,d7.classList.add(“is-active”);let e=()=>{d7.addEventListener(“transitionend”,u3,{once:!0}),d7.classList.remove(“is-active”)};clearTimeout(d5),d5=setTimeout(e,5e3)},u3=()=>{d7.innerHTML=””},m7={init:()=>{k3()},showToast:s3};var Y4,m5=!1,l3=async()=>new Promise(t=>{setTimeout(()=>{console.log(“simulating createShareLink for localhost”),t(“https://inquirer.com/interactives”),d3()},100)}),d3=()=>{let t=document.querySelector(“.js-gift-toast-receiver”);!t||!(t instanceof HTMLElement)||setTimeout(()=>{let e=t?.querySelector(“span”);e&&(e.innerHTML=”Gift link copied to clipboard“)},20)},m3=()=>{let t=window.services?.createShareLink;t&&(Y4=t),Q7()&&(Y4=l3),Y4&&y3()},h3=async t=>{let e=”text/plain”,_=async()=>{try{return await Y4(window.location.pathname)}catch{t.dataset.state=”error”,m7.showToast(“Hmm, we couldn’t generate a gift link…”)}},n=new ClipboardItem({[e]:_()});await navigator.clipboard.write([n]).catch(o=>{console.log(o),m7.showToast(“Couldn’t copy to clipboard, try again?”),t.dataset.state=”error”}),m7.showToast(“Gift link copied to clipboard!”),t.dataset.state=”complete”},y3=()=>{document.querySelectorAll(“.js-gift”).forEach(e=>{(z4()||Q7()||J4())&&e.classList.add(“is-available”)}),document.querySelectorAll(“.js-gift-button”).forEach(e=>{e instanceof HTMLButtonElement&&e.addEventListener(“click”,()=>{e.classList.contains(“disabled”)||(e.dataset.state=”loading”,m5=!0,h3(e),setTimeout(()=>{e.dataset.state=”ready”},2e3))})});let t=document.querySelector(“.js-gift-toast-receiver”);!t||!(t instanceof HTMLElement)||g3(t)},g3=t=>{new MutationObserver(_=>{for(let n of _){let o=[…n.addedNodes].at(0);if(!(o instanceof HTMLElement))return;m5&&m7.showToast(o.outerHTML)}}).observe(t,{subtree:!0,childList:!0})},h5={init:()=>{m3()}};var x3=()=>{window.addEventListener(“message”,t=>{if(t.data[“datawrapper-height”]){let e=t.data[“datawrapper-height”];for(let _ in e)document.querySelector(`#datawrapper-chart-${_}`).setAttribute(“height”,e[_])}})},w3=()=>{document.querySelectorAll(“.js-datawrapper-graphic”).forEach(t=>{q0(`https://datawrapper.dwcdn.net/${t.dataset.id}/embed.js`,null,t)})},v3=()=>{window.addEventListener(“message”,t=>{let e=t.data;document.querySelectorAll(`iframe[src*=”${e.id}”]`).forEach(n=>{n.style.height=`${e.height}px`})},!1)},P3=()=>{document.querySelectorAll(“.js-pym-graphic”).forEach(t=>{if(typeof window{new window.pym.Parent(t.id,t.dataset.iframe)};typeof window.pym>”u”?q0(“https://pym.nprapps.org/pym.v1.min.js”,e):e()}})},y5={init:()=>{x3(),w3(),P3(),v3()}};var Z7,b3=()=>{document.querySelectorAll(“.js-hover”).forEach(t=>{t.addEventListener(“click”,()=>{g5(t)}),t.addEventListener(“mouseenter”,()=>{g5(t)}),t.addEventListener(“mouseout”,()=>{x5(t)})}),window.addEventListener(“scroll”,()=>{Z7!==null&&M3()})},M3=()=>{(Z7>window.scrollY+100||Z7{x5(t)})},g5=t=>{t.classList.add(“is-visible”),Z7=window.scrollY},x5=t=>{t.classList.remove(“is-visible”),Z7=null},w5={init:()=>{b3()}};var X4,C3=(t,e)=>{X4=X4||window.PMNdataLayer,X4?X4.push({event:”misc_event”,eventAction:t,eventLabel:e}):window.location.hostname.includes(“localhost”)?console.log(“Analytics event:”,t,e,”(not actually being sent due to localhost)”):console.log(“Failed to push analytics event”,t,e)},v5={event:(t,e)=>{C3(t,e)}};var P5=1,J0=class{constructor(e){this.el=e,this.contentPosition=”default”,this.possibleSteps=new Array,this.currentStep=null,this.currentCounty=null,this.offset=window.innerHeight*.9,this.instanceOfSteps=P5,P5++,this.setPossibleSteps(),this.updateContent(),this.bindings()}setPossibleSteps(){this.el.querySelectorAll(“.js-steps-step”).forEach(e=>{e.dataset.step&&this.possibleSteps.push(e.dataset.step)})}bindings(){window.addEventListener(“scroll”,()=>{this.updateContent()}),window.addEventListener(“resize”,()=>{this.updateContent()})}updateContent(){this.updateCurrentStep()}updateCurrentStep(){let e,_=this.el.querySelectorAll(“.js-steps-step”);if(_.forEach((n,o)=>{n.getBoundingClientRect().top{let i=”is-“+o,f=”is-“+r;this.possibleSteps.indexOf(o){document.querySelectorAll(“.js-steps”).forEach(t=>{new J0(t)})}};var S3=(t,e,_)=>{document.querySelectorAll(“.js-subscribe”).forEach(n=>{n.classList.toggle(“is-unsubscribed”,!t),n.classList.toggle(“is-preview”,e),n.classList.toggle(“is-dev”,_)})},M5={init:()=>{S3(z4(),J4(),Q7())}};var N3=()=>{},C5={init:()=>{N3()}};var N7,V0,W0=!0,A3=()=>{N7=document.querySelectorAll(“.js-video-autoplay”)},E3=()=>{window.addEventListener(“resize”,()=>{S5()}),window.addEventListener(“scroll”,()=>{S5()}),N7.forEach(t=>{t.addEventListener(“volumechange”,e=>{t.muted!==W0&&!c5()&&(W0=t.muted,F3())})})},S5=()=>{let t;N7.forEach((e,_)=>{let n=e.getBoundingClientRect(),o=n.height/2;n.y-o&&(t=e)}),t!==V0&&(V0=t,N7.forEach(e=>{e.pause()}),t?t.play():V0=null)},F3=()=>{N7.forEach(t=>{t.muted=W0})},N5={init:()=>{A3(),N7&&E3()}};var A5={init:()=>{o7.init?.(),W4.init?.(),l5.init?.(),h5.init?.(),y5.init?.(),w5.init?.(),b5.init?.(),M5.init?.(),C5.init?.(),N5.init?.(),m7.init?.()}};var T3=()=>{},E5={init:()=>{T3()}};var L3=document.querySelector(“.js-inno”),F5=()=>{A5.init(),E5.init()};L3?F5():new MutationObserver((e,_)=>{if(document.querySelector(“.js-inno”)){_.disconnect(),F5();return}}).observe(document,{attributes:!0,childList:!0,subtree:!0});})();