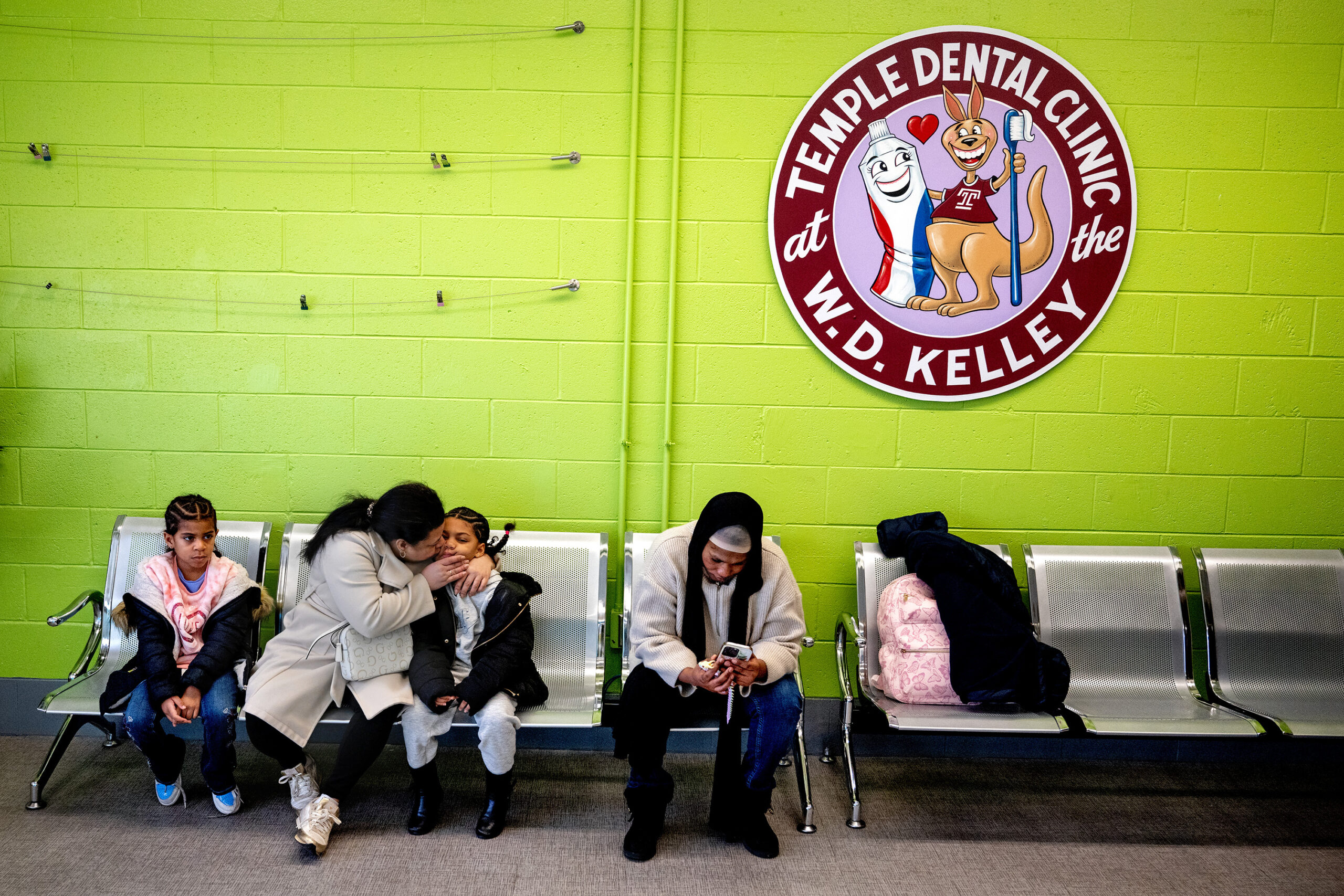
Crystal Edwards didn’t see a dentist until she had a deep cavity at age 10: growing up in a struggling Philadelphia family, the resources to access dental checkups just weren’t there.
So she jumped at the opportunity to locate a dental clinic in the school where she is now principal, W.D. Kelley, a K-8 in North Philadelphia.
“This dental clinic is saving lives,” said Edwards.
Tucked into a converted science lab on the school’s third floor, the Dental Clinic at William. D. Kelley, operated by Temple University’s Maurice H. Kornberg School of Dentistry, is nearing its third year of operation. It is open to all Philadelphia children, including those who do not attend Kelley, regardless of insurance status.
School district officials have pointed to the Kelley clinic as a model as it prepares to make facilities master plan decisions, which will result in closing, combining, and reconfiguring some school buildings. The clinic is an example, they say, of how the system could use available space in some of its schools for public good.

“This is certainly a great example of what can happen when a university partners with a school district to create life-changing opportunities and outcomes for young people,” Superintendent Tony B. Watlington Sr. said in a statement in 2023, when the clinic opened.
Temple dental school officials said more clinics could follow elsewhere in the city.
Taking care of every child
The underlying concept is simple, said Eileen Barfuss, the Temple dental professor who leads the clinic.
“If your tooth hurts, if you’re not feeling well, you’re not going to learn,” said Barfuss. “In the past, there have been a lot of barriers to care for dentistry that weren’t there for medicine, but preventative care is so important so it doesn’t get to the point of pain.”
The clinic accepts all comers, including those who are uninsured or underinsured, and sometimes treats students’ parents. (Most, but not all, patients have Medicaid dental, and grants help cover treatment for those without insurance.)

“We try to take care of every child in the Philadelphia School District,” said Barfuss. “There’s a place that they can come and get comprehensive care and establish a dental home.”
To date, the clinic has seen nearly 700 patients, some of whom are repeat visitors. Patients are treated both by Barfuss and dental students she supervises.
Students do come from other schools to the clinic; Barfuss said her team does outreach at community events and spreads the word through the district’s school nurses, who often send patients to the clinic. And staff teach lessons in Kelley classrooms on oral health and the importance of seeing a dentist twice a year.
Being in a school helps normalize the dentist for many kids, who might poke their heads into the clinic to look around and see the friendly dental staff in their scrubs in the hallways, Barfuss said.
‘This is a good dentist’
On Thursday, Fatoumata Bathily, a fourth grader with pink glasses and a bright smile, swung her legs down from a Kelley clinic dentist chair after a successful checkup.

“It’s good here,” said Fatoumata, who attends nearby Robert Morris Elementary, and came for preventive care along with her brother, Abubakr. “This is a good dentist. I like that it’s colorful, and the people are nice.”
Amid Ismail has wanted to bring such a model to the city since he became dean of Temple’s dental school in 2008. Decades ago, some schools offered dental care via city services, but as funding dried up, those clinics went away, Ismail said.
Ismail raised the idea of a Temple-district partnership, but it took several years to get off the ground. Edwards, an award-winning principal who takes pride in bringing the community into Kelley, got the vision intuitively, he said.
Temple paid to transform a large science lab into the dental clinic; the district provides the space and does not charge rent. There are four chairs, including one in a space specifically designed for patients with autism who might need a quieter environment and more room. Rooms are bright and modern.
“The message to the parents and caregivers is that this is a nice place where all treatment is provided,” Ismail said. “A lot of children do have dental problems, but here we can treat them easily — they miss one class, max, and they don’t have to stay a long time.”
The clinic, which is about to celebrate its third anniversary, just expanded its schedule — it’s open four days a week, and officials eventually hope it will be open five days.
Edwards fought for the clinic to come to Kelley, and it’s been just the boon she had hoped, she said.
“This is a historic community that was really devastated and hard hit by the crack and drug pandemic,” said Edwards. “The dental office has really given us leverage on how to serve the community better.”