NEW YORK — The U.S. has finalized its withdrawal from the World Health Organization, one year after President Donald Trump announced America was ending its 78-year-old commitment, federal officials said Thursday.
But it’s hardly a clean break.
The U.S. owes about $280 million to the global health agency, according to WHO. And Trump administration officials acknowledge that they haven’t finished working out some issues, such as lost access to data from other countries that could give America an early warning of a new pandemic.
The withdrawal will hurt the global response to new outbreaks and will hobble the ability of U.S. scientists and pharmaceutical companies to develop vaccines and medicines against new threats, said Lawrence Gostin, a public health law expert at Georgetown University.
“In my opinion, it’s the most ruinous presidential decision in my lifetime,” he said.
The WHO is the United Nations’ specialized health agency and is mandated to coordinate the response to global health threats, such as outbreaks of mpox, Ebola, and polio. It also provides technical assistance to poorer countries; helps distribute scarce vaccines, supplies, and treatments; and sets guidelines for hundreds of health conditions, including mental health and cancer.
Nearly every country in the world is a member.
Trump cited COVID-19 in pulling U.S. from WHO
U.S. officials helped lead the WHO’s creation, and America has long been among the organization’s biggest donors, providing hundreds of millions of dollars and hundreds of staffers with specialized public health expertise.
On average, the U.S. pays $111 million a year in member dues to the WHO and roughly $570 million more in annual voluntary contributions, according to the U.S. Department of Health and Human Services.
In an executive order issued right after taking office, Trump said the U.S. was withdrawing from WHO due to the organization’s mishandling of the COVID-19 pandemic and other global health crises. He also cited the agency’s “failure to adopt urgently needed reforms” and its “inability to demonstrate independence from the inappropriate political influence of WHO member states.”
WHO, like other public health organizations, made costly mistakes during the pandemic, including at one point advising people against wearing masks. It also asserted that COVID-19 wasn’t airborne, a stance it didn’t officially reverse until 2024.
Another Trump administration complaint: None of WHO’s chief executives — there have been nine since the organization was created in 1948 — have been Americans. Administration officials view that as unfair given how much the WHO relies on U.S. financial contributions and on U.S. Centers for Disease Control and Prevention personnel.
Public health experts say U.S. exit will hobble responses to threats
Experts say the U.S. exit could cripple numerous global health initiatives, including the effort to eradicate polio, maternal and child health programs, and research to identify new viral threats.
Ronald Nahass, president of the Infectious Diseases Society of America, called the U.S. withdrawal “shortsighted and misguided” and “scientifically reckless.”
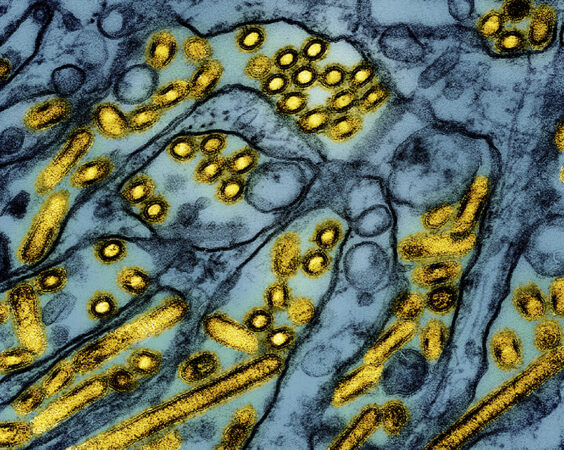
The U.S. has ceased official participation in WHO-sponsored committees, leadership bodies, governance structures and technical working groups. That would seem to include the WHO group that assesses what flu strains are circulating and makes critical decisions about updating flu shots.
It also signals the U.S. is no longer participating in global flu information-sharing that guides vaccine decisions.
Such disease intelligence has helped Americans be “at the front of the line” when new outbreaks occur and new vaccines and medicines are quickly needed to counteract them and save lives, Gostin said.
Trump administration officials say they already have public health relationships with many countries and are working to ensure direct sharing of that kind of information, rather than having WHO serve as a middleman. But U.S. officials did not give specifics about how many such arrangements are in place.
Gostin, an expert on international public health treaties and collaborations, said it’s unlikely the U.S. will reach agreements with more than a couple dozen countries.
Many emerging viruses are first spotted in China, but “is China going to sign a contract with the United States?” Gostin said. “Are countries in Africa going to do it? Are the countries Trump has slapped with a huge tariff going to send us their data? The claim is almost laughable.”
Gostin also believes Trump overstepped his authority in pulling out of WHO. The U.S. joined the organization through an act of Congress and it is supposed to take an act of Congress to withdraw, he argued.
U.S. still owes money, WHO says
The U.S. is legally required to give notice one year in advance of withdrawal — which it did — but also to pay any outstanding financial obligations.
The U.S. has not paid any of its dues for 2024 and 2025, leaving a balance of about $280 million at current exchange rates, according to WHO.
An administration official denied that requirement Thursday, saying the U.S. had no obligation to pay prior to withdrawing as a member.